View This Issue in Pdf Format
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

JRA 29 1 Bookreview 190..192
Reviews of Books In , Deyell published his book Living Without Silver,3 which has become the definitive work on the monetary history of early medieval north India. In this new book, he has stretched back in time by a couple of centuries and has produced what is destined to become the definitive work on the coinage of that period. <[email protected]> PANKAJ TANDON Boston University MUSLIMS AGAINST THE MUSLIM LEAGUE:CRITIQUES OF THE IDEA OF PAKISTAN. Edited by ALI USMAN QASMI and MEGAN EATON ROBB. pp. vii, . Delhi, Cambridge University Press, . doi:./S One of the great developments of the last ten years of British rule in India was the transformation of the position of the All-India Muslim League. In the elections it won just five per cent of the Muslim vote; it could not be regarded as a serious political player. Yet, in the elections of – it won about per cent of the Muslim vote, winning out of seats in the central and provincial legislatures, a result which meant that the British and the Indian National Congress had to take seriously the League’s demand for the creation of Pakistan at independence, a demand which it had formally voiced in March . With the creation of Pakistan in , which was also the formation of the most populous Muslim nation in the world at the time, the narrative of how some Muslims, mainly from the old Mughal service class of northern India, began a movement for the reassertion and protection of their interests in the nineteenth century which ended up as the foundation of a separate Muslim state in the twentieth century, was the dominant Muslim story of British India. -

Download Download
Nisan / The Levantine Review Volume 4 Number 2 (Winter 2015) Identity and Peoples in History Speculating on Ancient Mediterranean Mysteries Mordechai Nisan* We are familiar with a philo-Semitic disposition characterizing a number of communities, including Phoenicians/Lebanese, Kabyles/Berbers, and Ismailis/Druze, raising the question of a historical foundation binding them all together. The ethnic threads began in the Galilee and Mount Lebanon and later conceivably wound themselves back there in the persona of Al-Muwahiddun [Unitarian] Druze. While DNA testing is a fascinating methodology to verify the similarity or identity of a shared gene pool among ostensibly disparate peoples, we will primarily pursue our inquiry using conventional historical materials, without however—at the end—avoiding the clues offered by modern science. Our thesis seeks to substantiate an intuition, a reading of the contours of tales emanating from the eastern Mediterranean basin, the Levantine area, to Africa and Egypt, and returning to Israel and Lebanon. The story unfolds with ancient biblical tribes of Israel in the north of their country mixing with, or becoming Lebanese Phoenicians, travelling to North Africa—Tunisia, Algeria, and Libya in particular— assimilating among Kabyle Berbers, later fusing with Shi’a Ismailis in the Maghreb, who would then migrate to Egypt, and during the Fatimid period evolve as the Druze. The latter would later flee Egypt and return to Lebanon—the place where their (biological) ancestors had once dwelt. The original core group was composed of Hebrews/Jews, toward whom various communities evince affinity and identity today with the Jewish people and the state of Israel. -

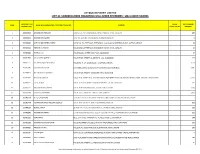
Unclaimed Deposits
1 / 7 Bank Name : INDUSTRIAL DEVELOPMENT BANK OF PAKISTAN Branch NAME AND ADDRESS OF DEPOSITORS Account Instrument,if any Transaction Nature of Last date of deposit or S. NAME OF Account Type Currency FCS Deposit Instrument Type Rate Type withdrawal (DD- Reasons if any, why not operated upon CNIC No/ ( e.g Current, (USD,EUR,G Contract Rate of PKR Rate applied date (LCY,UFZ,FZ) Account Number (DD,PO,FDD,TDR, Instrument NO (MTM,FCS Amount Outstanding Eqv.PKR surrendered MON-YYYY) No code Name PROVINCE Name Address Saving, Fixed BP,AED,JPY No (if conversion (DD-MON-YYYY) Passport No CO) R) or any other) ,CHF) any) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 1 10 Main Br. Karachi SD 517-90-218324 M/s. Linex International (Pvt) Ltd F-382 Metrovill S.I.T.E. Karachi LCY 1110802 CURR PKR 5,533.08 5,533.08 9-Feb-2000 lack of interest 2 10 Main Br. Karachi SD 502-93-307155 Nadir Badruddin 422 Sector-A North Nazimabad Karachi LCY 1110835 CURR PKR 10,425.00 10,425.00 26-Sep-2000 lack of interest 3 10 Main Br. Karachi SD 271-64-039991 Estern Frighter Services 3-A 1st Floor Dinar Chamber West Wharf Road Karachi LCY 1110861 CURR PKR 3,000.00 3,000.00 19-Jan-2000 lack of interest 42202-0303162-1 4 10 Main Br. Karachi SD Yousuf Raza Hussain & Mrs. Tahira C-169/3 K.D.A. -

Remembering Partition: Violence, Nationalism and History in India
Remembering Partition: Violence, Nationalism and History in India Gyanendra Pandey CAMBRIDGE UNIVERSITY PRESS Remembering Partition Violence, Nationalism and History in India Through an investigation of the violence that marked the partition of British India in 1947, this book analyses questions of history and mem- ory, the nationalisation of populations and their pasts, and the ways in which violent events are remembered (or forgotten) in order to en- sure the unity of the collective subject – community or nation. Stressing the continuous entanglement of ‘event’ and ‘interpretation’, the author emphasises both the enormity of the violence of 1947 and its shifting meanings and contours. The book provides a sustained critique of the procedures of history-writing and nationalist myth-making on the ques- tion of violence, and examines how local forms of sociality are consti- tuted and reconstituted by the experience and representation of violent events. It concludes with a comment on the different kinds of political community that may still be imagined even in the wake of Partition and events like it. GYANENDRA PANDEY is Professor of Anthropology and History at Johns Hopkins University. He was a founder member of the Subaltern Studies group and is the author of many publications including The Con- struction of Communalism in Colonial North India (1990) and, as editor, Hindus and Others: the Question of Identity in India Today (1993). This page intentionally left blank Contemporary South Asia 7 Editorial board Jan Breman, G.P. Hawthorn, Ayesha Jalal, Patricia Jeffery, Atul Kohli Contemporary South Asia has been established to publish books on the politics, society and culture of South Asia since 1947. -

CASTE SYSTEM in INDIA Iwaiter of Hibrarp & Information ^Titntt
CASTE SYSTEM IN INDIA A SELECT ANNOTATED BIBLIOGRAPHY Submitted in partial fulfilment of the requirements for the award of the degree of iWaiter of Hibrarp & information ^titntt 1994-95 BY AMEENA KHATOON Roll No. 94 LSM • 09 Enroiament No. V • 6409 UNDER THE SUPERVISION OF Mr. Shabahat Husaln (Chairman) DEPARTMENT OF LIBRARY & INFORMATION SCIENCE ALIGARH MUSLIM UNIVERSITY ALIGARH (INDIA) 1995 T: 2 8 K:'^ 1996 DS2675 d^ r1^ . 0-^' =^ Uo ulna J/ f —> ^^^^^^^^K CONTENTS^, • • • Acknowledgement 1 -11 • • • • Scope and Methodology III - VI Introduction 1-ls List of Subject Heading . 7i- B$' Annotated Bibliography 87 -^^^ Author Index .zm - 243 Title Index X4^-Z^t L —i ACKNOWLEDGEMENT I would like to express my sincere and earnest thanks to my teacher and supervisor Mr. Shabahat Husain (Chairman), who inspite of his many pre Qoccupat ions spared his precious time to guide and inspire me at each and every step, during the course of this investigation. His deep critical understanding of the problem helped me in compiling this bibliography. I am highly indebted to eminent teacher Mr. Hasan Zamarrud, Reader, Department of Library & Information Science, Aligarh Muslim University, Aligarh for the encourage Cment that I have always received from hijft* during the period I have ben associated with the department of Library Science. I am also highly grateful to the respect teachers of my department professor, Mohammadd Sabir Husain, Ex-Chairman, S. Mustafa Zaidi, Reader, Mr. M.A.K. Khan, Ex-Reader, Department of Library & Information Science, A.M.U., Aligarh. I also want to acknowledge Messrs. Mohd Aslam, Asif Farid, Jamal Ahmad Siddiqui, who extended their 11 full Co-operation, whenever I needed. -

Group Housing
LIST OF ALLOTED PROPERTIES DEPARTMENT NAME- GROUP HOUSING S# RID PROPERTY NO. APPLICANT NAME AREA 1 60244956 29/1013 SEEMA KAPUR 2,000 2 60191186 25/K-056 CAPT VINOD KUMAR, SAROJ KUMAR 128 3 60232381 61/E-12/3008/RG DINESH KUMAR GARG & SEEMA GARG 154 4 60117917 21/B-036 SUDESH SINGH 200 5 60036547 25/G-033 SUBHASH CH CHOPRA & SHWETA CHOPRA 124 6 60234038 33/146/RV GEETA RANI & ASHOK KUMAR GARG 200 7 60006053 37/1608 ATEET IMPEX PVT. LTD. 55 8 39000209 93A/1473 ATS VI MADHU BALA 163 9 60233999 93A/01/1983/ATS NAMRATA KAPOOR 163 10 39000200 93A/0672/ATS ASHOK SOOD SOOD 0 11 39000208 93A/1453 /14/AT AMIT CHIBBA 163 12 39000218 93A/2174/ATS ARUN YADAV YADAV YADAV 163 13 39000229 93A/P-251/P2/AT MAMTA SAHNI 260 14 39000203 93A/0781/ATS SHASHANK SINGH SINGH 139 15 39000210 93A/1622/ATS RAJEEV KUMAR 0 16 39000220 93A/6-GF-2/ATS SUNEEL GALGOTIA GALGOTIA 228 17 60232078 93A/P-381/ATS PURNIMA GANDHI & MS SHAFALI GA 200 18 60233531 93A/001-262/ATS ATUULL METHA 260 19 39000207 93A/0984/ATS GR RAVINDRA KUMAR TYAGI 163 20 39000212 93A/1834/ATS GR VIJAY AGARWAL 0 21 39000213 93A/2012/1 ATS KUNWAR ADITYA PRAKASH SINGH 139 22 39000211 93A/1652/01/ATS J R MALHOTRA, MRS TEJI MALHOTRA, ADITYA 139 MALHOTRA 23 39000214 93A/2051/ATS SHASHI MADAN VARTI MADAN 139 24 39000202 93A/0761/ATS GR PAWAN JOSHI 139 25 39000223 93A/F-104/ATS RAJESH CHATURVEDI 113 26 60237850 93A/1952/03 RAJIV TOMAR 139 27 39000215 93A/2074 ATS UMA JAITLY 163 28 60237921 93A/722/01 DINESH JOSHI 139 29 60237832 93A/1762/01 SURESH RAINA & RUHI RAINA 139 30 39000217 93A/2152/ATS CHANDER KANTA -

List of Life Members As on 20Th January 2021
LIST OF LIFE MEMBERS AS ON 20TH JANUARY 2021 10. Dr. SAURABH CHANDRA SAXENA(2154) ALIGARH S/O NAGESH CHANDRA SAXENA POST HARDNAGANJ 1. Dr. SAAD TAYYAB DIST ALIGARH 202 125 UP INTERDISCIPLINARY BIOTECHNOLOGY [email protected] UNIT, ALIGARH MUSLIM UNIVERSITY ALIGARH 202 002 11. Dr. SHAGUFTA MOIN (1261) [email protected] DEPT. OF BIOCHEMISTRY J. N. MEDICAL COLLEGE 2. Dr. HAMMAD AHMAD SHADAB G. G.(1454) ALIGARH MUSLIM UNIVERSITY 31 SECTOR OF GENETICS ALIGARH 202 002 DEPT. OF ZOOLOGY ALIGARH MUSLIM UNIVERSITY 12. SHAIK NISAR ALI (3769) ALIGARH 202 002 DEPT. OF BIOCHEMISTRY FACULTY OF LIFE SCIENCE 3. Dr. INDU SAXENA (1838) ALIGARH MUSLIM UNIVERSITY, ALIGARH 202 002 HIG 30, ADA COLONY [email protected] AVANTEKA PHASE I RAMGHAT ROAD, ALIGARH 202 001 13. DR. MAHAMMAD REHAN AJMAL KHAN (4157) 4/570, Z-5, NOOR MANZIL COMPOUND 4. Dr. (MRS) KHUSHTAR ANWAR SALMAN(3332) DIDHPUR, CIVIL LINES DEPT. OF BIOCHEMISTRY ALIGARH UP 202 002 JAWAHARLAL NEHRU MEDICAL COLLEGE [email protected] ALIGARH MUSLIM UNIVERSITY ALIGARH 202 002 14. DR. HINA YOUNUS (4281) [email protected] INTERDISCIPLINARY BIOTECHNOLOGY UNIT ALIGARH MUSLIM UNIVERSITY 5. Dr. MOHAMMAD TABISH (2226) ALIGARH U.P. 202 002 DEPT. OF BIOCHEMISTRY [email protected] FACULTY OF LIFE SCIENCES ALIGARH MUSLIM UNIVERSITY 15. DR. IMTIYAZ YOUSUF (4355) ALIGARH 202 002 DEPT OF CHEMISTRY, [email protected] ALIGARH MUSLIM UNIVERSITY, ALIGARH, UP 202002 6. Dr. MOHAMMAD AFZAL (1101) [email protected] DEPT. OF ZOOLOGY [email protected] ALIGARH MUSLIM UNIVERSITY ALIGARH 202 002 ALLAHABAD 7. Dr. RIAZ AHMAD(1754) SECTION OF GENETICS 16. -

Institute of Business Administration, Karachi Bba, Bs
FINAL RESULT - FALL 2020 ROUND 1 Announced on Tuesday, February 25, 2020 INSTITUTE OF BUSINESS ADMINISTRATION, KARACHI BBA, BS (ACCOUNTING & FINANCE), BS (ECONOMICS) & BS (SOCIAL SCIENCES) ADMISSIONS TEST HELD ON SUNDAY, FEBRUARY 9, 2020 (FALL 2020, ROUND 1) LIST OF SUCCESSFUL CANDIDATES FOR DIRECT ADMISSION (BSAF PROGRAM) SAT Test Math Eng TOTAL Maximum Marks 800 800 1600 Cut-Off Marks 600 600 1410 Math Eng Total IBA Test MCQ MCQ MCQ Maximum Marks 180 180 360 Cut-Off Marks 100 100 256 Seat S. No. App No. Name Father's Name No. 1 18 845 FABIHA SHAHID SHAHIDSIDDIQUI 132 136 268 2 549 1510 MUHAMMAD QASIM MAHMOOD AKHTAR 148 132 280 3 558 426 MUHAMMAD MUTAHIR ABBAS AMAR ABBAS 144 128 272 4 563 2182 ALI ABDULLAH MUHAMMAD ASLAM 136 128 264 5 1272 757 MUHAMMAD DANISH NADEEM MUHAMMAD NADEEM TAHIR 136 128 264 6 2001 1 MUHAMMAD JAWWAD HABIB MUHAMMAD NADIR HABIB 160 100 260 7 2047 118 MUHAMMAD ANAS LIAQUAT ALI 148 128 276 8 2050 125 HAFSA AZIZ AZIZAHMED 128 136 264 9 2056 139 MUHAMMAD SALMAN ANWAR MUHAMMAD ANWAR 156 132 288 10 2086 224 MOHAMMAD BADRUDDIN RIND BALOCH BAHAUDDIN BALOCH 144 112 256 11 2089 227 AHSAN KAMAL LAGHARI GHULAM ALI LAGHARI 136 160 296 12 2098 247 SYED MUHAMMAD RAED SYED MUJTABA NADEEM 152 132 284 13 2121 304 AREEB AHMED BAIG ILHAQAHMED BAIG 108 152 260 14 2150 379 SHAHERBANO ‐ ABDULSAMAD SURAHIO 148 124 272 15 2158 389 AIMEN ATIQ SYED ATIQ UR REHMAN 148 124 272 16 2194 463 MUHAMMAD SAAD MUHAMMAD ABBAS 152 136 288 17 2203 481 FARAZ NAWAZ MUHAMMAD NAWAZ 132 128 260 18 2210 495 HASNAIN IRFAN IRFAN ABDULAZIZ 128 132 260 19 2230 -

Copyright by Mohammad Raisur Rahman 2008
Copyright by Mohammad Raisur Rahman 2008 The Dissertation Committee for Mohammad Raisur Rahman certifies that this is the approved version of the following dissertation: Islam, Modernity, and Educated Muslims: A History of Qasbahs in Colonial India Committee: _____________________________________ Gail Minault, Supervisor _____________________________________ Cynthia M. Talbot _____________________________________ Denise A. Spellberg _____________________________________ Michael H. Fisher _____________________________________ Syed Akbar Hyder Islam, Modernity, and Educated Muslims: A History of Qasbahs in Colonial India by Mohammad Raisur Rahman, B.A. Honors; M.A.; M.Phil. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin August 2008 Dedication This dissertation is dedicated to the fond memories of my parents, Najma Bano and Azizur Rahman, and to Kulsum Acknowledgements Many people have assisted me in the completion of this project. This work could not have taken its current shape in the absence of their contributions. I thank them all. First and foremost, I owe my greatest debt of gratitude to my advisor Gail Minault for her guidance and assistance. I am grateful for her useful comments, sharp criticisms, and invaluable suggestions on the earlier drafts, and for her constant encouragement, support, and generous time throughout my doctoral work. I must add that it was her path breaking scholarship in South Asian Islam that inspired me to come to Austin, Texas all the way from New Delhi, India. While it brought me an opportunity to work under her supervision, I benefited myself further at the prospect of working with some of the finest scholars and excellent human beings I have ever known. -

Acknowledgement
Acknowledgement We are extremely grateful to the following members of the medical profession from Pakistan and Overseas for sparing their precious time to review the manuscript during the year, 2012. Reviewer’s No. of Reviewer’s No. of Reviewer’s No. of Name Manuscript Name Manuscript Name Manuscript Reviewed Reviewed Reviewed A Razaque Shaihk, Hyderabad 2 Jahan Ara Pal, Karachi 5 Saba Sohail, Karachi 5 A Sattar Hashim, Karachi 2 Kamaran Hafeez, Karachi 6 Saeed Minhas, Karachi 4 Abdul Basit, Karachi 3 Khadigeh Nasri, Iran 1 Sajid Rashid, Multan 2 Abdul Haque, Faisalabad 1 Khaleeq-uz-Zaman, Islamabad 1 Saleem Marfani, Karachi 1 Abdul Rehman, Bahawalpur 3 Khalid Nawaz, Lahore 1 Saleem Sadiq, Karachi 3 Abdul Salam, Bangladesh 6 Khan Shah Zaman Khan, Karachi 2 Salman Ahmed Tipu, Rawalpindi 3 Abdul Samad, Oman 4 Laiq Hussain Siddiqui, Lahore 2 Sameen Afzal Junejo, Hyderabad 3 Ahmad Badar, Saudi Arabia 2 M Asif Qureshi, Karachi 1 Sarwat Ara, Faisalabad 1 Akhtar Sherin, Kohat 2 M Aslam, Lahore 4 Seema Bibi, Hyderabad 3 Ali Mohammad 1 M Azeem Aslam, Islamabad 1 Seema Mumtaz, Karachi 1 Sabzghabaee, Iran M Sarwar, Karachi 3 Shahid Hameed, Lahore 4 M Waqar Rabbani, Multan 3 Ameer Malik, Bahawalpur 1 Shahid Mahmood Baig, 2 Anisuddin Bhatti, Karachi 2 M Zubair, Karachi 1 Faisalabad Anwar Naqvi, Karachi 1 M. Akbar Chaudhry, Lahore 5 Shahida Khawaja, Lahore 2 Aqeel Safdar, Islamabad 1 M. Aslam Maj. Gen., Islamabad 3 Shakeel Baig, Karachi 1 Arturo Langa, Scotland, UK 1 M. Zaman Shaikh, Karachi 2 Shamim Qureshi, Karachi 2 Arif-ur-Rehman, Karachi 5 Mahfooz-ur-Rehman, Lahore 3 Shams Nadeem Alam, Karachi 3 Ata Mahmood Poor, Iran 4 Mansoor Ahmed, Karachi 1 Shaukat Ali, Karachi 4 Azeem Aslam, Islamabad 1 Maqbool H. -

2020 Daily Prayer Calendar
2020 Daily Prayer Calendar for South Asia largest Unreached People Groups Western edition To order prayer resources or for inquiries, contact email: [email protected] 2020 Daily Prayer Calendar for South Asia largest LR-Unreached People Groups (people selection based on unreached status, size & photo availability) downloaded July 2019 from website: joshuaproject.net Bangladesh = country (PG photo) Explanation (country flag) = no PG photo avail. (+ 2020 dates) of Ansari = people name Frontier = 0.1% Christian or less daily 1,230,000 = population LR-UPG= Least-Reached, Unreached PG data: Bengali = main language (LR-UPG=less than 2% Evangelical) Islam = main religion (& less than 5% total Christian) Let's dream God's dreams & fulfill God's visions -- God dreams of all people groups knowing & loving Him! * * * Revelation 7:9, "After this I looked and there before me was a great multitude that no one could count, from every nation, tribe, people and language, standing before the throne and in front of the Lamb." January -- Daily Prayer Calendar for South Asia Largest Unreached People Groups Sunday Monday Tuesday Wednesday Thursday Friday Saturday Bangladesh Bangladesh Bangladesh Bangladesh 2020 = 1 2020 = 2 2020 = 3 2020 = 4 Ansari Bairagi, Hindu Bihari, Muslim Brahman, gen. 1,230,000 209,000 913,000 584,000 Bengali Bengali Urdu Bengali Islam Frontier Hinduism Frontier Islam Frontier Hinduism Frontier Bangladesh Bangladesh Bangladesh Bangladesh Bangladesh Bangladesh Bangladesh 2020 = 5 2020 = 6 2020 = 7 2020 = 8 2020 = 9 2020 = 10 2020 = 11 -
List of Unclaimed Shares and Dividend
ATTOCK REFINERY LIMITED LIST OF SHAREHOLDERS REGARDING UNCLAIMED DIVIDENDS / UNCLAIMED SHARES FOLIO NO / CDC SHARE NET DIVIDEND S/NO. NAME OF SHAREHOLDER / CERTIFICATE HOLDER ADDRESS ACCOUNT NO. CERTIFICATES AMOUNT 1 208020582 MUHAMMAD HAROON DASKBZ COLLEGE, KHAYABAN-E-RAHAT, PHASE-VI, D.H.A., KARACHI 450 2 208020632 MUHAMMAD SALEEM SHOP NO.22, RUBY CENTRE,BOULTON MARKETKARACHI 8 3 307000046 IGI FINEX SECURITIES LIMITED SUIT # 701-713, 7TH FLOOR, THE FORUM, G-20, BLOCK 9, KHAYABAN-E-JAMI, CLIFTON, KARACHI 15 4 307013023 REHMAT ALI HASNIE HOUSE # 96/2, STREET # 19, KHAYABAN-E-RAHAT, DHA-6, KARACHI. 15 5 307020846 FARRUKH ALI HOUSE # 246-A, STREET # 39, F-11/3, ISLAMABAD 67 6 307022966 SALAHUDDIN QURESHI HOUSE # 785, STREET # 11, SECTOR G-11/1, ISLAMABAD. 174 7 307025555 ALI IMRAN IQBAL MOTIWALA HOUSE NO. H-1, F-48-49, BLOCK - 4, CLIFTON, KARACHI. 2,550 8 307026496 MUHAMMAD QASIM C/O HABIB AUTOS, ADAM KHAN, PANHWAR ROAD, JACOBABAD. 2,085 9 307028922 NAEEM AHMED SIDDIQUI HOUSE # 429, STREET # 4, SECTOR # G-9/3, ISLAMABAD. 7 10 307032411 KHALID MEHMOOD HOUSE # 10 , STREET # 13 , SHAHEEN TOWN, POST OFFICE FIZAI, C/O MADINA GERNEL STORE, CHAKLALA, RAWALPINDI. 6,950 11 307034797 FAZAL AHMED HOUSE # A-121,BLOCK # 15,RAILWAY COLONY , F.B AREA, KARACHI 225 12 307037535 NASEEM AKHTAR AWAN HOUSE # 183/3 MUNIR ROAD , LAHORE CANTT LAHORE . 1,390 13 307039564 TEHSEEN UR REHMAN HOUSE # S-5, JAMI STAFE LANE # 2, DHA, KARACHI. 3,475 14 307041594 ATTIQ-UR-REHMAN C/O HAFIZ SHIFATULLAH,BADAR GENERALSTORE,SHAMA COLONY,BEGUM KOT,LAHORE 7 15 307042774 MUHAMMAD NASIR HUSSAIN SIDDIQUI HOUSE-A-659,BLOCK-H, NORTH NAZIMABAD, KARACHI.