SACN STATEMENT on IODINE and HEALTH February 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Super Green Superfoods
[Plant-Based Ingredients] Vol. 17 No. 12 December 2012 Super Green Superfoods By Celeste Sepessy, Associate Editor Once the secret of Birkenstock-wearing progressives, green foods are now filling the shopping carts of informed—if not guilty—conventional consumers. Nutrient-dense greens date back millions of years, and humans in the know have been eating them for centuries; green foods manufacturers commonly tout their ingredients as the energy food of ancient Mesoamericans, namely the Aztecs. The term "green foods" encompasses a range of raw materials including algae (chlorella, spirulina, etc.), grasses (alfalfa, barley grass, wheat grass, etc.) and common green vegetables (broccoli, spinach, etc.). Though each ingredient boasts its own benefits, they all pack a well-rounded nutritional punch not often found elsewhere. "Spirulina is nature's multivitamin," said John Blanco, president of AnMar International, noting the microalgae has 60-percent protein, unsaturated fatty acids and vitamin precursors, such as amino acids and proenzymes. "It's not a complete 100-percent balanced vitamin tablet, but it's pretty close." And this nutritional breakdown is similar across the green board, as the ingredients are densely filled with phytonutrients, antioxidants, vitamins, minerals and nucleic acid, among other nutrients. Consumers of all demographics are becoming more aware of the benefits of eating these green superfoods; Guinevere Lynn, director of business development at Sun Chlorella, pointed to the media for the industry's popularity surge. "Mass media has certainly played a major role in this 'green renaissance,' " she explained, citing Dr. Oz's help in particular. The television medical personality is a huge proponent of green foods, and Dr. -
FACT SHEET – Multivitamin Inclusion in SNAP
FACT SHEET – Multivitamin Inclusion in SNAP Low-income Americans do not obtain all the nutrients they need from food alone. • Data from the 2015-2020 Dietary Guidelines for Americans show that many Americans do not meet their requirements for several important nutrients. • Nutrition surveys consistently show that substantial numbers of Americans fail to obtain the recommended amounts of a variety of essential nutrients from diet alone. • Calcium, magnesium, and vitamins A, D, E, and C are some of the nutrients that are consumed below the recommended levels. Iron is also under-consumed by many women. • Calcium and vitamin D are considered “nutrients of public health concern” because low intakes are associated with particular health concerns. • Studies show that low-income and older Americans are more likely to have insufficient and nutritionally inadequate diets. Science underscores the role of a multivitamin for filling critical nutrient gaps. • Dietary supplements, like the multivitamin, provide shortfall nutrients and have been shown to help Americans fill nutrient gaps. • A multivitamin, in combination with a balanced diet, is a healthy choice and can play an important role in promoting good nutrition and well-being. • The U.S. Preventive Services Task Force (USPSTF) recommends that all women planning or capable of pregnancy take a daily supplement containing 400 to 800 micrograms of folic acid. • Several leading medical authorities recommend that all pregnant women take a daily supplement that contains 150 micrograms of iodine daily. • Data from the 2001-2008 National Health and Nutrition Examination Survey (NHANES) reveal nutrient shortfalls in children at 88% for vitamin D, 54% for calcium, and 41% for magnesium. -
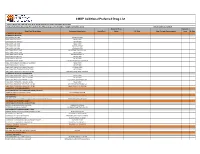
CMDP Additional Preferred Drug List
CMDP Additional Preferred Drug List • Generic Drugs Are Preferred Drugs Over Brand Name Drugs Unless Specified as Brand Only • Federally Reimbursable Drugs Not Listed On The AHCCCS Drug List Are Available Through Prior Authorization Effective Date: 11/2/2018 Preferred Drug Quantity Drug Class/Drug Name Reference Brand Name Brand Only Status PA Type Step Therapy Requirements Limit QL Days ALTERNATIVE MEDICINES ALTERNATIVE MEDICINE MELATONIN CAP 5 MG CVS MELATONIN MELATONIN CAP 10 MG MELATONIN MELATONIN TAB 300 MCG MELATONIN MELATONIN TAB 1 MG MELATONIN MELATONIN TAB 3 MG GNP MELATONIN MELATONIN TAB 5 MG CVS MELATONIN MELATONIN TAB ER 1 MG MELATONIN TIMED RELEASE MELATONIN TAB ER 5 MG MELATONIN MELATONIN TAB ER 10 MG MM MELATONIN TR MELATONIN SL TAB 3 MG MELATONIN MELATONIN SL TAB 5 MG MELATONIN MELATONIN SL TAB 10 MG CVS MELATONIN QUICK DISSOLVE MELATONIN LIQUID 1 MG/4ML (2.5 MG/10ML) MELATONIN MELATONIN LIQUID 1 MG/ML MELATONIN MELATONIN TABLET DISINTEGRATING 3 MG SV MELATONIN MELATONIN TABLET DISINTEGRATING 5 MG MELATONIN MELATONIN TABLET DISINTEGRATING 10 MG HM MELATONIN QUICK DISSOLVE ALTERNATIVE MEDICINE COMBINATIONS MELATONIN-PYRIDOXINE TABLETS 1-10 MG MELATONIN MELATONIN-PYRIDOXINE TABLETS 3-10 MG MELATONIN MELATONIN-PYRIDOXINE TABLETS 5-1 MG EQL MELATONIN/VITAMIN B-6 MELATONIN-PYRIDOXINE TABLETS 5-10 MG MELATONIN MELATONIN-PYRIDOXINE TABLETS ER 3-10 MG MELATONIN TR/VITAMIN B-6 MELATONIN-PYRIDOXINE TABLETS ER 5-10 MG MELATONIN TR/VITAMIN B6 ANALGESICS - ANTI-INFLAMMATORY NONSTEROIDAL ANTI-INFLAMMATORY AGENTS (NSAIDS) NAPROXEN SODIUM CAPSULES 220 MG EQL NAPROXEN SODIUM ANTHELMINTICS ANTHELMINTICS PYRANTEL PAMOATE SUSPENSION 144 MG/ML (50 MG/ML BASE EQUIV) REESES PINWORM MEDICINE ANTIDIARRHEAL/PROBIOTIC AGENTS ANTIDIARRHEAL/PROBIOTIC COMBINATIONS BACILLUS COAGULANS-INULIN CAPSULES PROBIOTIC FORMULA LACTOBACILLUS-INULIN CAPSULES CULTURELLE DIGESTIVE HEALTH ANTIDIARRHEAL/PROBIOTIC AGENTS - MISC. -

Multivitamin/Mineral Supplements Fact Sheet for Consumers
Multivitamin/mineral Supplements Fact Sheet for Consumers What are multivitamin/mineral (MVM) dietary supplements? Multivitamin/mineral (MVM) supplements contain a combination of vitamins and minerals, and sometimes other ingredients as well. They go by many names, includ- ing multis and multiples or simply vitamins. The vitamins and minerals in MVMs have unique roles in the body. For more information about each one, see our dietary supplement fact sheets. What kinds of MVM supplements are available? There are many types of MVMs in the marketplace. Manufacturers choose which vitamins, minerals, and other ingredients, as well as their amounts, to include in their products. Among the most common MVMs are basic, once-daily products containing all More than one-third of Americans or most vitamins and minerals, with the majority in amounts that are close to take MVMs. recommended amounts. Higher-potency MVMs often come in packs of two or more pills to take each day. Manufacturers promote other MVMs for special purposes, such as better performance or energy, weight control, or improved immunity. These products usually contain herbal and other ingredients (such as echinacea and glucosamine) in addition to vitamins and minerals. The recommended amounts of nutrients people should get vary by age and gender and are known as Recommended Dietary Allowances (RDAs) and Adequate Intakes (AIs). One value for each nutrient, known as the Daily Value (DV), is selected for the labels of dietary supplements and foods. A DV is often, but not always, similar to one’s RDA or AI for that nutrient. The label provides the %DV so that you can see how much (what percentage) a serving of the product contributes to reaching the DV. -

Dietary Supplement Laboratory Quality Assurance Program: Exercise M Final Report
NISTIR 8203 Dietary Supplement Laboratory Quality Assurance Program: Exercise M Final Report Melissa M. Phillips Catherine A. Rimmer Laura J. Wood Maria R. Ale Charles A. Barber Hannah Stindt Lee Yu This publication is available free of charge from: https://doi.org/10.6028/NIST.IR.8203 NISTIR 8203 Dietary Supplement Laboratory Quality Assurance Program: Exercise M Final Report Melissa M. Phillips Catherine A. Rimmer Laura J. Wood Maria R. Ale Charles A. Barber Hannah Stindt Lee Yu Chemical Sciences Division Material Measurement Laboratory This publication is available free of charge from: https://doi.org/10.6028/NIST.IR.8203 February 2018 U.S. Department of Commerce Wilbur L. Ross, Jr., Secretary National Institute of Standards and Technology Walter Copan, NIST Director and Under Secretary of Commerce for Standards and Technology ABSTRACT The NIST Dietary Supplement Laboratory Quality Assurance Program (DSQAP) was established in collaboration with the National Institutes of Health (NIH) Office of Dietary Supplements (ODS) in 2007 to enable members of the dietary supplements community to improve the accuracy of measurements for demonstration of compliance with various regulations including the dietary This publication is available free of charge from: http from: charge of free available is publication This supplement current Good Manufacturing Practices (cGMPs). Exercise M of this program offered the opportunity for laboratories to assess their in-house measurements of nutritional elements (potassium and zinc), contaminants (arsenic and lead), water-soluble vitamins (thiamine (B1) and riboflavin (B2)), fat-soluble vitamins (total vitamin K1, cis- and trans-vitamin K1), botanical marker compounds (curcuminoids, chondroitin sulfate), and identity (chondroitin) in foods and/or botanical dietary supplement ingredients and finished products. -

Multivitamins | Benefits and Risks |
UW MEDICINE | PATIENT EDUCATION | | Multivitamins | Benefits and risks | This handout explains the benefits and risks of taking multivitamins. It also includes the results of some scientific studies. Should I take a multivitamin? Taking a multivitamin can help some people. But, studies show that taking a multivitamin may be harmful for other people. Multivitamins are also linked with having a greater risk of cancer. The 1994 Dietary Supplement Health and Education Act (DSHEA) ruled that multivitamins and other dietary supplements no longer need to be approved by the Food and Drug Administration (FDA). This means that vitamins you find in the store or online have not been checked by the FDA for quality, strength, or purity. It is always best to meet your nutritional needs by eating a varied, plant- based diet with plenty of vitamin-rich fruits and vegetables. Who should take multivitamins? Taking a multivitamin may help some people. Those who benefit the most from taking a multivitamin are: • Pregnant women • People who eat less than 1,200 calories a day • Strict vegetarians or vegans • People with limited diets due to food preferences, allergies or intolerances, gastric bypass surgery, or chemotherapy What do scientific studies show? Results from scientific studies vary. Page 2 gives examples of some recent If possible, it is always best to meet studies. The source for each your body’s nutritional needs with study is included. plenty of vitamin-rich foods. _________________________________ ____________________________________________________________ Page 1 of 2 | Multivitamins Prostate Cancer Prevention Clinic/Men’s Health Center | Box 354785 1959 N.E. Pacific St., Seattle, WA 98195 | 206.598.6358 • Several studies have shown that vitamin D helps prevent cancer. -

Ratings of the Effectiveness of Nutraceuticals for Autism Spectrum Disorders: Results of a National Survey
Journal of Personalized Medicine Article Ratings of the Effectiveness of Nutraceuticals for Autism Spectrum Disorders: Results of a National Survey James B. Adams 1,* , Anisha Bhargava 2, Devon M. Coleman 1, Richard E. Frye 3 and Daniel A. Rossignol 4 1 School of Engineering of Matter, Transport, and Energy, Arizona State University, P.O. Box 876106, Tempe, AZ 85287, USA; [email protected] 2 Columbia Mailman School of Public Health, 722 W. 168th St., New York, NY 10032, USA; [email protected] 3 Section of Neurodevelopmental Disorders, Division of Neurology, Barrow Neurological Institute at Phoenix Children’s Hospital, 1919 E Thomas Rd., Phoenix, AZ 85016, USA; [email protected] 4 Rossignol Medical Center, 24541 Pacific Park Drive, Suite 210, Aliso Viejo, CA 92656, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-480-965-3316 Abstract: Autism spectrum disorder (ASD) often involves a wide range of co-occurring medical conditions (“comorbidities”) and biochemical abnormalities such as oxidative stress and mitochon- drial dysfunction. Nutritional supplements (“Nutraceuticals”) are often used to treat both core ASD symptoms and comorbidities, but some have not yet been formally evaluated in ASD. The potential biological mechanisms of nutraceuticals include correction of micronutrient deficiencies due to a poor diet and support for metabolic processes such as redox regulation, mitochondrial dysfunction and melatonin production. This paper reports on the results of the National Survey on Treatment Effectiveness for Autism, focusing on nutraceuticals. The Survey involved 1286 participants from across the United States. Participants rated the overall perceived benefits and adverse effects of each nutraceutical, and also indicated the specific symptoms changed and adverse effects. -

The Special Operations Forces Nutrition Guide
The Special Operations Forces Nutrition Guide Patricia A. Deuster, PhD, MPH, CNS Teresa Kemmer, PhD, RD Lori Tubbs, MS, RD Stacey Zeno, MS Christiane Minnick, M.Ac i Acknowledgements Many people have contributed to this revised guide, and it is dif- ficult to list all those who have made small contributions. However, we must acknowledge those who have made major contributions. First, we thank LtCol Charity Thomasos, RD, USAF for her comments and sugges- tions on multiple chapters and her efforts on chapters 11 and 12. We thank our primary points for contact at the SOF Commands who arranged and coordinated our site visits, to include LCDR David C. Krulak, MC from MARSOC, MAJ(P) Anthony Littrell, MC, USA from USASOC, LTC Robert Lutz, MC, USA from JSOC, MAJ Keith E. Schlechte, MC, USAF from AFSOC, and CDR Lanny Boswell, MSC, USN from NAVSOC. We offer a very special thanks to LCDR Jim Mucciarone, MC, UMO/DMO, Senior Medical Officer for Naval Special Warfare, who provided invaluable feedback on the chapters. We recognize MAJ Dirk Geers, Special Operations and Personnel Recovery Office in Belgium, who used the previous Navy SEAL Guide and posed many questions before the new guide was begun and provided excel- lent comments based on his use of the information for deployments. We also thank CAPT Roger Herbert, Commander of NSW Training who spent time discussing the importance of nutrition to BUD/S training. Ms. Jennifer Davis is recognized and thanked for her dedication to the Excel spreadsheets that were developed specifically for this effort—she did a wonderful job. -
Nutrients of Concern for Individuals Following a Plant-Based Diet Continuing Education Content Provided By
Special Continuing Education Supplement June 2014 The Magazine for Nutrition Professionals FREE CE COURSE Nutrients of Concern for Individuals Following a Plant-Based Diet Continuing education content provided by Includes recipes from Sweet and Spicy Vegetarian Chili page 10 www.bushbeansfoodservice.com CPE COURSE Defining Plant-Based Diets The Dietary Guidelines Advisory Committee says a plant- based diet emphasizes vegetables, cooked dry beans and peas, fruits, whole grains, nuts, and seeds.6 Vegans don’t eat animal products, including dairy and eggs. Vegetarians (also known as lacto-ovo vegetarians) don’t eat meat but do eat dairy and eggs; pescatarians (or pesco-vegetarians) eat fish but no other meats; and semivegetarians (or flexitarians) occasionally eat fish, poultry, or meat. Of course, many people call themselves vegetarians but follow eating patterns that diverge from these definitions. For example, some people may be nearly vegan, eating dairy and eggs only on rare occasions, and some may call themselves vegetarians but still eat small amounts of meat. Since there are many variations of a plant-based diet, it’s important for health professionals, including dietitians, to establish a person’s true eating pattern to accurately assess nutritional intake and status.7 Brief History of Plant-Based Eating While plant-based eating may appear to be a new trend, it actually dates back to ancient times. Claus Leitzmann, PhD, a retired professor from Justus Liebig Universitat in Germany, NUTRIENTS OF CONCERN spoke on the history of vegetarianism at the Sixth Interna- tional Congress on Vegetarian Nutrition in February 2013. He FOR INDIVIDUALS FOLLOWING reported that ancient cultures, including those in Egypt, China, A PLANT-BASED DIET India, Peru, and Mexico, ate a predominantly plant-based diet. -

The Efficacy of Spirulina in Comparison with Multivitamin Supplements Amongst Children Attending Ard El Insan Association Clinic in Gaza Strip
Al-Azhar University – Gaza Deanship of Postgraduate Studies & Scientific Research Faculty of Pharmacy Master Program of Clinical Nutrition The Efficacy of Spirulina in Comparison with Multivitamin Supplements amongst Children Attending Ard El Insan Association Clinic in Gaza Strip By Mahmoud A. El-Sheikh Ali Supervised by Dr. Suliman Eljabour Dr. Abed El-Raziq Salama Ass. Professor of Pharmaceutical Ass. Professor of Food Science and Technology and Medicinal Chemistry Faculty of Agriculture Faculty of Pharmacy Al-Azhar University - Gaza Al-Azhar University - Gaza A thesis Submitted in Partial Fulfillment of the Requirements for the Master Degree in Clinical Nutrition Gaza – Palestine 1435 / 2014 Dedication I would like to express my gratitude to my family, my father and my mother. Special and warm appreciation to my wife and my children Who supported me all the way. To everyone who contributed to completion of this study …… thank you. Mahmoud A. El-Sheikh Ali i Declaration I certify that this thesis is a result of my own research, except where otherwise acknowledged, and that this thesis (or any part of the same) has not been submitted for a higher degree to any other university or institution. Mahmoud A. El-Sheikh Ali Signed ………………. September 2014 ii Acknowledgement Above all, I want to thank profoundly and humbly the almighty God for giving me such a great strength, patience, courage and ability to complete this research, and peace and blessings of Allah be upon the noblest of all Prophets and messengers, our prophet Muhammad, all thanks for Allah who granted me the power and capability to complete this thesis. -

Omega-3 Supplements May Interact with Drugs That Affect Blood Clotting
U.S. Department of Health & Human Services National Institutes of Health Omega-3 Supplements © Zoonar/Thinkstock Omega-3 fatty acids (omega-3s) are a group of polyunsaturated fatty acids that are important for a number of functions in the body. Some types of omega-3s are found in foods such as fatty fish and shellfish. Another type is found in some vegetable oils. Omega-3s are also available as dietary supplements. This fact sheet provides basic information about omega-3s—with a focus on dietary supplements, summarizes scientific research on effectiveness and safety, and suggests sources for additional information. Key Facts — There has been a substantial amount of research on supplements of omega-3s, particularly the types of omega-3s found in seafood and fish oil, and heart disease. The findings of individual studies have been inconsistent. In 2012, two combined analyses of the results of these studies did not find convincing evidence that these omega-3s protect against heart disease. — There is some evidence that omega-3s of the types found in seafood and fish oil may be modestly helpful in relieving symptoms in rheumatoid arthritis. For most other conditions for which omega-3s have been studied, definitive conclusions cannot yet be reached, or studies have not shown omega-3s to be beneficial. — Omega-3 supplements may interact with drugs that affect blood clotting. — It is uncertain whether people with fish or shellfish allergies can safely consume fish oil supplements. — Fish liver oils (which are not the same as fish oils) contain vitamins A and D as well as omega-3 fatty acids; these vitamins can be toxic in high doses. -

Supplements for Vegans (Or Anyone)
Supplements for Vegans (or anyone) BARRIERS IN GETTING ENOUGH NUTRIENTS: VITAMIN B12: • Low nutrient levels in degraded soils due to With no natural plant sources, it’s important to be industrial agriculture with chemical fertilizer aware of the deficiency symptoms and to take a high and pesticides quality supplement of B12 regularly – either in your • Low nutrient levels in highly processed foods multivitamin or in addition. • Low nutrient intake because of calorie- Best taken in the morning. restriction Ultra B12 Liquid • Low absorption and utilization rates if our digestive systems are weak or slowing down as we age CALCIUM: Plant sources are a better choice than dairy, but ANIMAL PRODUCTS USED IN SUPPLEMENTS: most people don’t eat quite enough food to get the • Gelatin capsules (made of animal bone). full recommended intake for the day, so a low level Cellulose (vegetable fiber) is used for supplement or fortified non-dairy milk a good idea. vegetarian capsules. Best taken in the evening. • Magnesium stearate (can be made of animal Pure Vegan Calcium/Magnesium oils or vegetable oils). So look for the company to specify which they use. ESSENTIAL FATTY ACIDS: • Vitamin D3 (sourced from oil in sheep’s wool). D3 is listed as cholecalciferol. The vegan form There are plenty of plant sources of omega-3, is D2 (ergocalciferol). There are now vegan and algae-based DHA supplements if you want a sources of D3 from mushrooms, but you’d have concentrated source. to check. DEVA Vegan DHA • Omega-3 and DHA often come as fish oil, but there are sources using algae or flaxseed oil.