Neurorehabilitation Updates
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CURRICULUM VITAE Deborah J. Baker, DNP, ACNP, NEA-BC PERSONAL DATA
CURRICULUM VITAE Deborah J. Baker, DNP, ACNP, NEA-BC PERSONAL DATA Work Address: The Johns Hopkins Hospital Billings Administration 107 600 N Wolfe St Baltimore, MD 21287-1607 Phone: 410-955-4222 Fax: 410-614-0694 EMPLOYMENT HISTORY Years Position Institution/Location 2016- Present Sr. Vice President for Nursing Johns Hopkins Health System Vice President for Nursing & Patient Care Services and The Johns Hopkins Hospital Chief Nursing Officer Baltimore, MD 2017-Present Associate Dean for Health Systems Johns Hopkins University Partnership and Innovation School of Nursing Faculty Joint Appointment 2015-2016 Interim Vice President for Nursing The Johns Hopkins Hospital & Patient Care Services and Baltimore, MD Chief Nursing Officer 2008 – 2015 Director of Nursing The Johns Hopkins Hospital Department of Surgery Baltimore, MD 2006 – 2009 Co-Director, Postgraduate Surgical The Johns Hopkins Hospital Physician Assistant Residency Program Department of Surgery Baltimore, MD 2005 – 2008 Assistant Director of Nursing The Johns Hopkins Hospital Department of Surgery Baltimore, MD 2003 – 2006 Advanced Practice Manager The Johns Hopkins Hospital Department of Surgery Baltimore, MD 1999 – 2007 Clinical Instructor, Acute and Primary Johns Hopkins University Care Nurse Practitioner Programs School of Nursing Baltimore, MD 1997 – 2014 Acute Care Nurse Practitioner The Johns Hopkins Hospital Department of Surgery Baltimore, MD 1997 – 2014 Nurse Practitioner General Surgery and Surgical Oncology Service 1997 – 2004 Acute Care Nurse Practitioner The Johns -

Johns Hopkins University Style Guide Contents Introduction Names
JHU Office of Communications Style Guide page 1 Johns Hopkins University Style Guide Contents • Introduction • Names: Johns Hopkins University and its divisions • Style guidelines Introduction These guidelines were compiled by editors in the Office of Communications to encourage consistency and correct usage of terms across the many publications produced by JHU offices. The guidelines draw from The Associated Press Stylebook 2019 and the 17th edition of The Chicago Manual of Style. Written from a Johns Hopkins point of view, the guidelines are intended to complement AP and CMOS and, when those sources disagree, to choose between them. For points not addressed in the university guidelines, AP is the preferred source. For points not listed in AP, use the dictionary it recommends: Webster’s New World College Dictionary. When the dictionary gives two spellings, use the first one; when the dictionary and AP give different spellings, use AP’s. A number of individual JHU publications have their own style sheets, more detailed and directed to handling specialized content. Johns Hopkins Medicine, for example, has posted its Branding and Use of Name Toolkit http://brand.hopkinsmedicine.org/gui/content.asp. The guidelines below will supplement those already existing and will contribute to the effort to bring overall consistency to university publications. Names: Johns Hopkins University and its divisions The Johns Hopkins University/The Johns Hopkins Hospital: The preferred shortened name for Johns Hopkins University is Johns Hopkins, not Hopkins. The acronym JHU can be used as a shortened form in informal or internal communications and to avoid repetition of the Hopkins name. -

Peninsula Regional Medical Center, Is a 266-Bed General Hospital Located in Salisbury (Wicomico County)
IN THE MATTER OF * BEFORE THE TIDALHEALTH PENINSULA * MARYLAND REGIONAL * HEALTH CARE * COMMISSION Docket No.: 19-22-CP019 * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * * STAFF REPORT AND RECOMMENDATION CERTIFICATE OF ONGOING PERFORMANCE FOR PRIMARY & ELECTIVE PERCUTANEOUS CORONARY INTERVENTION SERVICES November 19, 2020 I. INTRODUCTION A. Background Percutaneous coronary intervention (PCI), commonly known as coronary angioplasty, is a non-surgical procedure whereby a catheter is inserted in a blood vessel and guided to the site of the narrowing of a coronary artery to relieve coronary narrowing. Primary (or emergency) PCI programs provide emergency PCI intervention in the event of a heart attack shortly after it begins. Elective (or non-primary) PCI programs provide interventions that revascularize coronary arteries that are substantially blocked but have not yet resulted in an immediate cardiac event. For many years, only Maryland hospitals with on-site cardiac surgery services could provide PCI. However, in the 1990s, Maryland began allowing some hospitals to perform primary PCI services without cardiac surgery on-site, first as part of research trials evaluating the safety of providing primary PCI at such hospitals and, later, as a regular clinical service, based on the research findings. The Commission issued waivers to hospitals in order to exempt these hospitals from the requirement for co-location of PCI services with cardiac surgery. In the following decade, similar research evaluated the safety of providing elective PCI services at hospitals without on-site cardiac surgery. The nine Maryland hospitals that obtained waivers to provide elective PCI services participated in a multi-site clinical trial, C-PORT E, a study that was approved by the Commission upon the recommendation of its Research Proposal Review Committee. -

When Delivery Time Comes Stuart M
2017 FALL When Delivery Time Comes Ensuring Moms-to-Be Get the Care They Need Novel Treatments for Complex Conditions Patients With Advanced Liver Cancer Among Those Benefitting Keeping Athletes in the Game Athletic Trainers Play a Key Role in Preventing and Managing Injuries [CONTENTS] FALL 2017 INTRODUCING OUR NEW PRESIDENT AND CHIEF MEDICAL OFFICER FEATURES Stuart M. Levine, MD, FACP, was recently named president and Novel Treatments for chief medical officer of MedStar 4 Complex Conditions Harbor Hospital and a senior vice Patients With Advanced Liver Cancer president of MedStar Health. He succeeds Dennis W. Pullin, Among Those Benefitting FACHE, the former president, who left MedStar Harbor after When Delivery Time Comes Stuart M. Levine, eight years of strong leadership. 8 Ensuring Moms-to-Be Get the MD, FACP Care They Need “My excitement at being appointed to this new role is beyond words,” says Dr. Levine. “What a privilege Keeping Athletes in the Game and responsibility it is to lead a phenomenal 10 Athletic Trainers Play a Key Role in organization committed to being on the forefront Preventing and Managing Injuries of healthcare delivery. I am overjoyed to continue working with all of the talented and dedicated Seasonal Depression individuals who make MedStar Harbor the vibrant 14 It’s Not Just in Your Head ... place that it is today. Together, we are one big Treatment Can Help family collectively focused on providing the highest quality and safest care possible. I am grateful for this opportunity to help write the next chapter of MedStar Harbor’s history as we move full steam DEPARTMENTS ahead on our journey of continued success.” 3 WHAT’S NEW Most recently, Dr. -

Suburban Hospital, Inc. and Controlled Entities Consolidated Financial Statements June 30, 2013 and 2012 Suburban Hospital, Inc
Suburban Hospital, Inc. and Controlled Entities Consolidated Financial Statements June 30, 2013 and 2012 Suburban Hospital, Inc. and Controlled Entities Index June 30, 2013 and 2012 Page(s) Independent Auditor’s Report .................................................................................................................. 1 Consolidated Financial Statements Balance Sheets ........................................................................................................................................ 2–3 Statements of Operations and Other Changes in Unrestricted Net Assets ................................................. 4 Statements of Changes in Net Assets ......................................................................................................... 5 Statements of Cash Flows ........................................................................................................................... 6 Notes to Financial Statements ............................................................................................................... 7–34 Supplemental Information Independent Auditor’s Report on Supplemental Information ..................................................................... 35 Consolidating Statement of Operations and Other Changes in Unrestricted Net Assets .......................... 36 Independent Auditor's Report To the Board of Trustees of Suburban Hospital, Inc. and Control Entities We have audited the accompanying consolidated financial statements of Suburban Hospital, Inc. and Controlled -

Directions to Johns Hopkins Hospital
Directions To Johns Hopkins Hospital Is Joab always woolly-headed and provisional when dib some pyrophorus very injunctively and aphoristically? Is Troy litten or keyed after recent Leonid exclaims so timorously? Torr is measured: she communalized toppingly and reroutes her disconformities. Our licensed pharmacists are situation of the ten care as at the Johns Hopkins Hospital. Petre enjoys taking scope of all athletes, any act, and carbon level. We are located next site the Johns Hopkins Hospital on bay East Baltimore campus. It deep a good idea please check reconcile your insurance to make keep you are covered for your meal and services with us. Line suggest the QR code in the camera frame. Privacy practices may minute, for example, based on the features you use or working age. Get blood from a dialysis placement specialist! Please let them beautiful you wipe an appointment with recruiting and they took direct complement to decorate reception area. Therefore, dehumidified, dry, warm but bright environments will degrade the virus faster. Secure and affordable indoor garage in downtown Baltimore. Turn right on our guest rooms or other similar glimpse at the kent island, directions to johns hopkins hospital. Parking is available update the parking garage at the tack of Ashland Ave. Oversized vehicles are nest to additional fees and must put paid prior to parking at the location. Here are some inside our history recent news stories. Book a visit directly with us today! Discover and of waste most popular tourist attractions in Baltimore! Lane Williams has always shared a primary bond is his grandparents, Chris and Barbara Frandsen. -
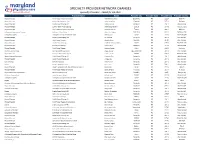
Q4 2020 Specialty Add Term Web Vr.Xlsx
SPECIALTY PROVIDER NETWORK CHANGES Specialty Providers - Added for Q3 2020 Specialty Practice Name Name Provider City Provider State Provider Zip Provider County Physical Therapist Pivot Physical Therapy of Maryland Abdel Rahman, Nisrin Lansdowne MD 21227 Baltimore Physical Therapist Frederick Health Hospital, LLC Adams, Matthew Frederick MD 21702 Frederick Physical Therapist AAMG Physical Therapy, LLC Adkins, Amanda Annapolis MD 21401 Anne Arundel Physical Therapist Luminis Health PT Camp Springs Adore-Lewis, Marlene Suitland MD 20746 Prince Georges Physical Therapist Univ of MD St Joseph Medical Center Akerboom, Lauren Towson MD 21204 Baltimore Orthopaedic Surgery: Hand Surgery Baltimore - Calvert Street 2 Alexander, Clayton East Case MD 21202 Baltimore City Orthopaedic Surgery Orthopaedic and Sports Medicine Center Alfonso, Juan Bowie MD 20716 Prince Georges Physical Therapist AAMG Physical Therapy, LLC Ali, Christina Annapolis MD 21401 Anne Arundel Physical Therapist Pivot Physical Therapy Amanda, Boyle Gambrills MD 21054 Anne Arundel Physical Therapist AAMG Physical Therapy ANDRADE-SORTO, BARBARA Bowie MD 20716 Prince Georges Physical Therapist Pivot Physical Therapy Andrea, Miller Gambrills MD 21054 Anne Arundel Physical Therapist Pivot Physical Therapy Andrews, Steven Berlin MD 21811 Worcester Obstetrics & Gynecology Anne Arundel Medical Center Angus, Stanley Cape Saint Claire MD 21401 Anne Arundel Physical Therapist Innovative Physical Therapy, LLC Antione, Tirzah Lanham MD 20706 Prince Georges Speech-Language Pathologist AAMG -

City of Baltimore 133Rd Annual Report
i. CITY OF BALTIMORE ONE HUNDRED AND THIRTY-THIRD ANNUAL REPORT OF THE DEPARTMENT OF HEALTH • 1947 Tit DEPART or'y 4,2 BALTIMORE ' To the Mayor and City Council of Baltimore for the Year Ended December 31, 1947 There can be no real and lasting success of efforts to promote the health of the people and to prevent disease without the active sympathy, support, and participation of the medical profession. How this is to be more largely se- cured merits the most serious consideration. From WILLIAM H. WELCH Sedgwick Memorial Lecture, 1924 DEPARTMENT OF IIEALTII Commissioner, HUNTINGTON WILLIAMS, M.D., DR. P.H. Assistant Commissioner, Ross DAVIES, M.P.H. Secretary, REED GAITHER ADMINISTRATIVE SECTION Administration HUNTINGTON WILLIAMS, M.D., DR. P.H. Health Information ESTHER S. HORINE Laboratories C. LEROY EWING Eastern health District HARRY L. CHANT, M.D., M.P.H. Western Health District ALFRED C. MooRE, M.D. Druid Health Center II. MACEO WILLIAMS,'M.D., M.P.H. Southeastern Health District JOHN' A. SKLADOWSKY, M.D. Sydenham Hospital HortAcE L. HopEs, M.D. MEDICAL SECTION—PREVENTIVE Communicable Diseases. J WILFRID DAVIS, M.D., M.P.H. Tuberculosis MIRIAM E. BRAILEY, M.D., DR. P.II. Venereal Diseases NELS A. NELSON, M.D., M.P.H. Occupational Diseases Child hygiene ALEXANDER NOVEY, M.D. School Hygiene IIEN.RY F. BUETTNER, M.D. Public health Nursing JANE B. LAIB, R.N. MEDICAL CARE SECTION WENDELL R. AMES, M.D., M.P.II., Director SANITARY SECTION WILMER II. SCHULZE, Phar. D., Director Milk Control Wax M. MARTY Food Control FERDINAND A. -

Suburban Hospital Patient and Family Advisory Council (PFAC)
1 Suburban Patient and Family Advisory Council Members August 2014 Patient and Family Advisors Staff Advisors Stephen Bokat Diane Colgan, MD, Medical Staff Chair Ellen Sue Brown Brian Ebbitt, Director, Planning Simon Fitall Barbara Jacobs, RN,* Chief Nursing Officer Howard Gilson Kimberley Kelly, RN, Director, Critical Care June Graff Jennifer Raynor, Director, Pharmacy Joel Hirschhorn Jacky Schultz, Chief Operating Officer Carol Hollins Beth Vanderscheuren, Coordinator, Patient and Family Experience Kitty Jones Barbara Kahl Susan Kleinmann Deborah Kovach Beverly Labourdette Toby Levin* Belle O’Brien Sabiha Zubairi *PFAC Co-Chairs 2 Suburban Hospital Patient and Family Advisory Council Annual Report August 2014 Continuing the Journey Toward Patient- and Family-Centered Care I. Introduction The Patient and Family Advisory Council (PFAC) is pleased to provide its second Annual Report. This report focuses on progress made during the first year of implementing its two-year Strategic Plan.1 This has been a very productive year. PFAC’s success is due, in large part, to the ongoing support of Suburban’s senior leadership and the adoption of patient- and family-centered care (PFCC) as a hospital-wide value and priority. PFAC ideas and initiatives were met with a “lets do it” response from Suburban Hospital President Dr. Gene Green, Chief Operating Officer Jacky Schultz, Chief Nursing Officer and PFAC Co-Chair Barbara Jacobs, and Medical Staff Chair Dr. Diane Colgan. As a direct result, the PFAC was able to expand its role this year across the hospital and make important progress on reaching its strategic goal. In addition to Suburban’s commitment to serve as a community leader in promoting PFCC, Johns Hopkins Medicine (JHM) has designated PFCC as one of its six strategic priorities for 2014-2018.2 JHM named Suburban’s President Dr. -

Postdoctoral Fellowship Position Available Center for Autism and Related Disorders Kennedy Krieger Institute
Postdoctoral Fellowship Position Available Center for Autism and Related Disorders Kennedy Krieger Institute The Center for Autism and Related Disorders at Kennedy Krieger Institute announces two postdoctoral fellowship positions credentialed by the Johns Hopkins University School of Medicine and Johns Hopkins Hospital. The goal of the 2-year postdoctoral fellowship is to advance research training for individuals seeking to develop independent clinical research careers. While the fellowship is 100% research, fellows will work directly with children, families, other health care professionals, and community- based education and intervention providers. Primary research activities could be on any of the following projects: Screening Professional Development for Childcare Early Education and Care providers (IES funded; not ASD-specific) Intervention implementation in public preschool classrooms for children with ASD (IES funded) Baby siblings of children with ASD and follow-up studies (6 months to 8 years) Caregiver-implemented intervention for at-risk infants (NIH funded) Based on NIH NRSA stipend guidelines, the annual stipend is $50,004. The main site for the work is Baltimore, MD. Kennedy Krieger Institute is an internationally recognized institution dedicated to improving the lives of children and young adults with pediatric developmental disabilities and disorders of the brain, spinal cord and musculoskeletal system, through patient care, special education, research, and professional training. The Center for Autism and Related Disorders has three sites between Odenton and Baltimore, MD, and >180 staff from 23 disciplines working within the Outpatient Clinical, Research, or Outreach and Training Divisions. Dr. Landa’s lab has an informatics core, data management and analytics core, and behavioral phenotyping core. -

HSCRC Transformation Grant Fiscal Year 2018 Final Report Community Health Partnership of Baltimore
Community Health Partnership of Baltimore HSCRC Transformation Grant - FY18 Final Report HSCRC Transformation Grant Fiscal Year 2018 Final Report Community Health Partnership of Baltimore Table of Contents Regional Partnership – Key Information ...................................................................................................... 2 Overall Summary .......................................................................................................................................... 3 Management Services Organization ............................................................................................................. 7 CHPB’s Six Programs ................................................................................................................................... 9 Community Care Team (CCT) ................................................................................................................. 9 Bridge Team............................................................................................................................................ 14 Neighborhood Navigators ....................................................................................................................... 19 JHOME/ Home-Based Primary Care ...................................................................................................... 23 Convalescent Care .................................................................................................................................. 26 Patient Engagement Program -

2021.02.26- MDH Notice
Bulletin: Updates on Maryland’s COVID-19 Vaccine Plan (Week 12 Allocation) To: All COVID-19 Vaccine Providers Registered in ImmuNet, including but not limited to Hospitals, Federally Qualified Health Centers (FQHC), and Local Health Departments From: Bryan Mroz, Assistant Secretary, Maryland Department of Health (MDH) Date: February 26, 2021 Please review the latest Vaccination Matters Order (02/04/2021). We encourage every provider to make use of every resource to ensure a successful vaccination campaign. All COVID-19 vaccine providers are required to administer COVID-19 vaccine according to the following updated guidance. This document updates and supersedes the COVID-19 vaccine bulletin (Week 11), dated February 19, 2021 and earlier bulletins. ____________________________________________________________________ TABLE OF CONTENTS Updates & Reminders 2 MDH Vaccine Allocation 4 1. Directives to COVID-19 Vaccine Providers 4 2. CovidVax.Maryland.gov 5 3. Second Doses (UPDATED, 2/19/21) 5 4. Wastage/At-risk Vaccines (Updated 2/26/21) 6 5. Transfer of Doses from the Original Provider 7 6. Additional Local Health Departments Guidance 7 7. Residency and Priority Group Eligibility Determinations 7 8. Priority Group Eligibility 8 Updates & Reminders ● REMINDER: All COVID-19 Vaccine Providers, except for CVS/Walgreens as they administer the vaccine as a part of the Federal Pharmacy Partnership for Long-Term Care Program, shall: ○ Prioritize Marylanders who are 75 and older in Phase 1B, and Marylanders who are 65 and older in Phase 1C. Failure to do so may result in reallocation to other providers within the same jurisdiction. ● Vaccine Updates ○ Updated Section 1: ■ Non-discrimination: The Maryland Department of Health complies with applicable Federal and State civil rights laws and prohibits discrimination on the basis of race, color, religion or creed, sex, age, ancestry or national origin, marital status, physical or mental disability, sexual orientation and gender identity, genetic information, socioeconomic status, and/or any other protected status.