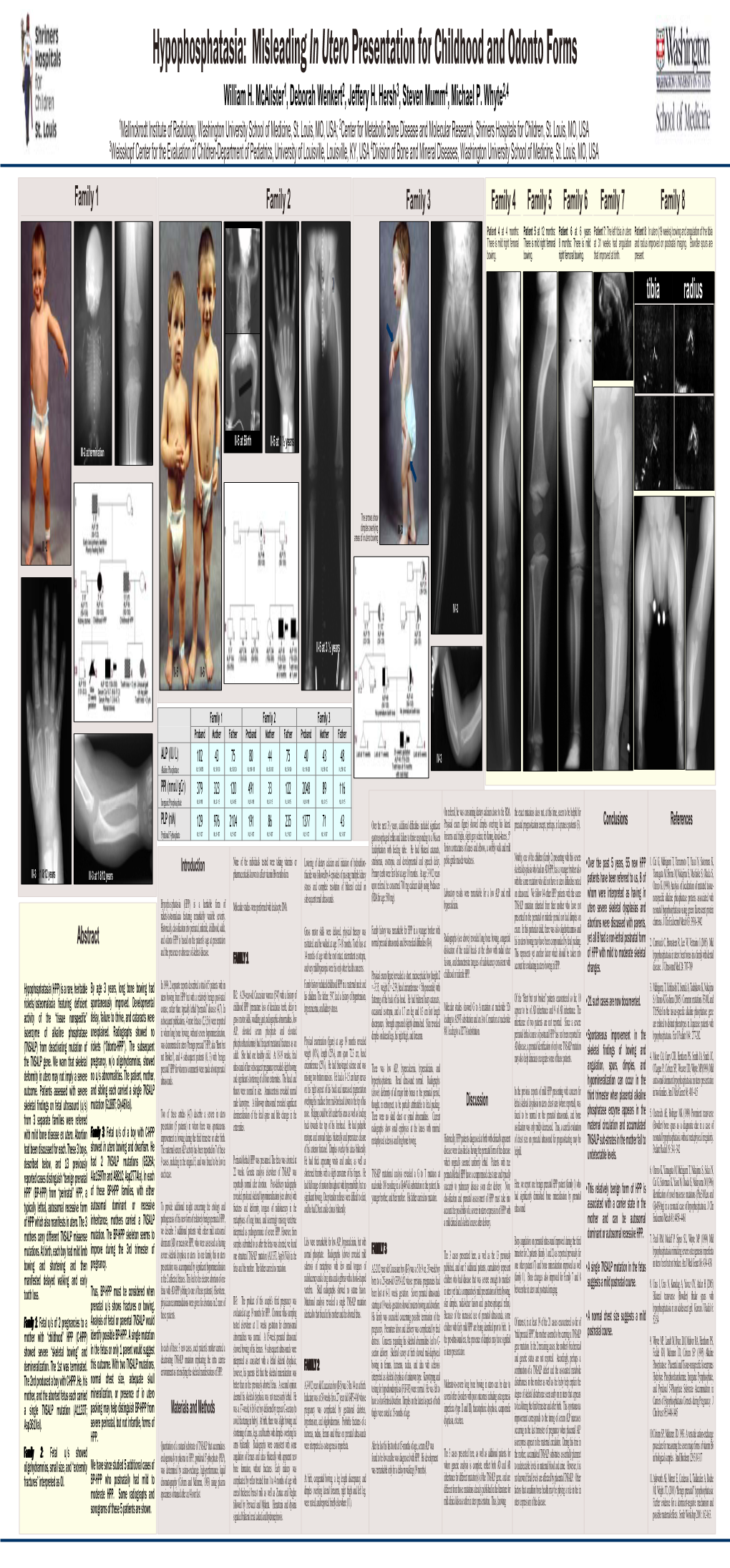
Hypophosphatasia: Misleading in Utero Presentation for Childhood and Odonto Forms William H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypophosphatasia Could Explain Some Atypical Femur Fractures
Hypophosphatasia Could Explain Some Atypical Femur Fractures What we know Hypophosphatasia (HPP) is a rare genetic disease that affects the development of bones and teeth in children (Whyte 1985). HPP is caused by the absence or reduced amount of an enzyme called tissue-nonspecific alkaline phosphatase (TAP), also called bone-specific alkaline phosphatase (BSAP). The absence of TAP raises the level of inorganic pyrophosphate (Pi), which prevents calcium and phosphate from creating strong, mineralized bone. Without TAP, bones can become weak. In its severe form, HPP is fatal and happens in 1/100,000 births. Because HPP is genetic, it can appear in adults as well. A recent study has identified a milder, more common form of HPP that occurs in 4 of 1000 adults (Dahir 2018). This form of HPP is usually seen in early middle aged adults who have low bone density and sometimes have stress fractures in the feet or thigh bone. Sometimes these patients lose their baby teeth early, but not always. HPP is diagnosed by measuring blood levels of TAP and vitamin B6. An elevated vitamin B6 level [serum pyridoxal 5-phosphate (PLP)] (Whyte 1985) in a patient with a TAP level ≤40 or in the low end of normal can be diagnosed with HPP. Almost half of the adult patients with HPP in the large study had TAP >40, but in the lower end of the normal range (Dahir 2018). The connection between hypophosphatasia and osteoporosis Some people who have stress fractures get a bone density test and are treated with an osteoporosis medicine if their bone density results are low. -

A Novel Germline Mutation of ADA2 Gene In
International Journal of Molecular Sciences Case Report A Novel Germline Mutation of ADA2 Gene in Two “Discordant” Homozygous Female Twins Affected by Adenosine Deaminase 2 Deficiency: Description of the Bone-Related Phenotype Silvia Vai 1,†, Erika Marin 1,† , Roberta Cosso 2 , Francesco Saettini 3, Sonia Bonanomi 3, Alessandro Cattoni 3, Iacopo Chiodini 1,4 , Luca Persani 1,4 and Alberto Falchetti 1,2,* 1 Department of Endocrine and Metabolic Diseases, IRCCS, Istituto Auxologico Italiano, 20145 Milan, Italy; [email protected] (S.V.); [email protected] (E.M.); [email protected] (I.C.); [email protected] (L.P.) 2 IRCCS, Istituto Auxologico Italiano, San Giuseppe Hospital, 28824 Verbania, Italy; [email protected] 3 Department of Pediatrics, Università degli Studi di Milano-Bicocca, Fondazione MBBM, San Gerardo Hospital, 20100 Monza, Italy; [email protected] (F.S.); [email protected] (S.B.); [email protected] (A.C.) 4 Department of Medical Biotechnologies and Translational Medicine, University of Milan, 20122 Milan, Italy * Correspondence: [email protected] † These authors equally contributed to this paper. Abstract: Adenosine Deaminase 2 Deficiency (DADA2) syndrome is a rare monogenic disorder preva- lently linked to recessive inherited loss of function mutations in the ADA2/CECR1 gene. It consists Citation: Vai, S.; Marin, E.; Cosso, R.; of an immune systemic disease including autoinflammatory vasculopathies, with a frequent onset Saettini, F.; Bonanomi, S.; Cattoni, A.; at -

Establishment of a Dental Effects of Hypophosphatasia Registry Thesis
Establishment of a Dental Effects of Hypophosphatasia Registry Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Jennifer Laura Winslow, DMD Graduate Program in Dentistry The Ohio State University 2018 Thesis Committee Ann Griffen, DDS, MS, Advisor Sasigarn Bowden, MD Brian Foster, PhD Copyrighted by Jennifer Laura Winslow, D.M.D. 2018 Abstract Purpose: Hypophosphatasia (HPP) is a metabolic disease that affects development of mineralized tissues including the dentition. Early loss of primary teeth is a nearly universal finding, and although problems in the permanent dentition have been reported, findings have not been described in detail. In addition, enzyme replacement therapy is now available, but very little is known about its effects on the dentition. HPP is rare and few dental providers see many cases, so a registry is needed to collect an adequate sample to represent the range of manifestations and the dental effects of enzyme replacement therapy. Devising a way to recruit patients nationally while still meeting the IRB requirements for human subjects research presented multiple challenges. Methods: A way to recruit patients nationally while still meeting the local IRB requirements for human subjects research was devised in collaboration with our Office of Human Research. The solution included pathways for obtaining consent and transferring protected information, and required that the clinician providing the clinical data refer the patient to the study and interact with study personnel only after the patient has given permission. Data forms and a custom database application were developed. Results: The registry is established and has been successfully piloted with 2 participants, and we are now initiating wider recruitment. -

Metabolic Bone Disease 5
g Metabolic Bone Disease 5 Introduction, 272 History and examination, 275 Osteoporosis, 283 STRUCTURE AND FUNCTION, 272 Investigation, 276 Paget’s disease of bone, 288 Structure of bone, 272 Management, 279 Hyperparathyroidism, 290 Function of bone, 272 DISEASES AND THEIR MANAGEMENT, 280 Hypercalcaemia of malignancy, 293 APPROACH TO THE PATIENT, 275 Rickets and osteomalacia, 280 Hypocalcaemia, 295 Introduction Calcium- and phosphate-containing crystals: set in a structure• similar to hydroxyapatite and deposited in holes Metabolic bone diseases are a heterogeneous group of between adjacent collagen fibrils, which provide rigidity. disorders characterized by abnormalities in calcium At least 11 non-collagenous matrix proteins (e.g. osteo- metabolism and/or bone cell physiology. They lead to an calcin,• osteonectin): these form the ground substance altered serum calcium concentration and/or skeletal fail- and include glycoproteins and proteoglycans. Their exact ure. The most common type of metabolic bone disease in function is not yet defined, but they are thought to be developed countries is osteoporosis. Because osteoporosis involved in calcification. is essentially a disease of the elderly, the prevalence of this condition is increasing as the average age of people Cellular constituents in developed countries rises. Osteoporotic fractures may lead to loss of independence in the elderly and is imposing Mesenchymal-derived osteoblast lineage: consist of an ever-increasing social and economic burden on society. osteoblasts,• osteocytes and bone-lining cells. Osteoblasts Other pathological processes that affect the skeleton, some synthesize organic matrix in the production of new bone. of which are also relatively common, are summarized in Osteoclasts: derived from haemopoietic precursors, Table 3.20 (see Chapter 4). -

Overuse Injuries in Sport: a Comprehensive Overview R
Aicale et al. Journal of Orthopaedic Surgery and Research (2018) 13:309 https://doi.org/10.1186/s13018-018-1017-5 REVIEW Open Access Overuse injuries in sport: a comprehensive overview R. Aicale1*, D. Tarantino1 and N. Maffulli1,2 Abstract Background: The absence of a single, identifiable traumatic cause has been traditionally used as a definition for a causative factor of overuse injury. Excessive loading, insufficient recovery, and underpreparedness can increase injury risk by exposing athletes to relatively large changes in load. The musculoskeletal system, if subjected to excessive stress, can suffer from various types of overuse injuries which may affect the bone, muscles, tendons, and ligaments. Methods: We performed a search (up to March 2018) in the PubMed and Scopus electronic databases to identify the available scientific articles about the pathophysiology and the incidence of overuse sport injuries. For the purposes of our review, we used several combinations of the following keywords: overuse, injury, tendon, tendinopathy, stress fracture, stress reaction, and juvenile osteochondritis dissecans. Results: Overuse tendinopathy induces in the tendon pain and swelling with associated decreased tolerance to exercise and various types of tendon degeneration. Poor training technique and a variety of risk factors may predispose athletes to stress reactions that may be interpreted as possible precursors of stress fractures. A frequent cause of pain in adolescents is juvenile osteochondritis dissecans (JOCD), which is characterized by delamination and localized necrosis of the subchondral bone, with or without the involvement of articular cartilage. The purpose of this compressive review is to give an overview of overuse injuries in sport by describing the theoretical foundations of these conditions that may predispose to the development of tendinopathy, stress fractures, stress reactions, and juvenile osteochondritis dissecans and the implication that these pathologies may have in their management. -

Vitamin D and Bone Health
1150 17th Street NW Suite 850 Washington, D.C. 200361 Bone Basics 1 (800) 231-4222 TEL ©National Osteoporosis Foundation 2013 1 (202) 223-2237 FAX www.nof.org Vitamin D and Bone Health Vitamin D plays an important role in protecting your bones. It may also help prevent other conditions including certain cancers. Your body requires vitamin D to absorb calcium. Children need vitamin D to build strong bones, and adults need it to keep bones strong and healthy. When people do not get enough vitamin D, they can lose bone. Studies show that people with low levels of vitamin D have lower bone density or bone mass. They are also more likely to break bones when they are older. Severe vitamin D deficiency is rare in the United States. It can cause a disease known as osteomalacia where the bones become soft. In children, this is known as rickets. These are both different conditions from osteoporosis. NOF Recommendations for Vitamin D The National Osteoporosis Foundation (NOF) recommends that adults under age 50 get 400-800 International Units (IU) of vitamin D every day, and that adults age 50 and older get 800-1,000 IU of vitamin D every day. Some people need more vitamin D. There are two types of vitamin D supplements. They are vitamin D2 and vitamin D3. Previous research suggested that vitamin D3 was a better choice than vitamin D2. However, more recent studies show that vitamin D3 and vitamin D2 are fairly equal for bone health. Vitamin D3 is also called cholecalciferol. Vitamin D2 is also called ergocalciferol. -

Osseous Manifestations of Primary Hyperparathyroidism: Imaging Findings
Hindawi International Journal of Endocrinology Volume 2020, Article ID 3146535, 10 pages https://doi.org/10.1155/2020/3146535 Review Article Osseous Manifestations of Primary Hyperparathyroidism: Imaging Findings Jackson Bennett ,1 James W. Suliburk ,2 and Fanny E. Moro´n 3 1School of Medicine, Baylor College of Medicine, Houston, TX, USA 2Department of Surgery, Baylor College of Medicine, Houston, TX, USA 3Department of Radiology, Baylor College of Medicine, Houston, TX, USA Correspondence should be addressed to Fanny E. Mor´on; [email protected] Received 13 September 2019; Revised 10 December 2019; Accepted 8 January 2020; Published 21 February 2020 Academic Editor: Giorgio Borretta Copyright © 2020 Jackson Bennett et al. -is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Primary hyperparathyroidism is a systemic endocrine disease that has significant effects on bone remodeling through the action of parathyroid hormone on the musculoskeletal system. -ese findings are important as they can aid in distinguishing primary hyperparathyroidism from other forms of metabolic bone diseases and inform physicians regarding disease severity and complications. -is pictorial essay compiles bone-imaging features with the aim of improving the diagnosis of skeletal in- volvement of primary hyperthyroidism. 1. Introduction the symptomatic classical variant in some individuals [2, 4]. Other HPT disease subtypes include secondary and tertiary Hyperparathyroidism (HPT) is an endocrine disorder de- disease, which are primarily seen in patients with chronic fined by a state of inappropriately increased levels of renal disease and posttransplant patients [7]. -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -

Fracture Healing Complications in Patients Presenting with High-Energy Trauma Fractures and Bone Health Intervention Debra L
Scientific Poster #116 Polytrauma OTA 2014 Fracture Healing Complications in Patients Presenting with High-Energy Trauma Fractures and Bone Health Intervention Debra L. Sietsema, PhD1,2; Michael D. Koets, BS3; Clifford B. Jones, MD1,2; 1Orthopaedic Associates of Michigan, Grand Rapids, Michigan, USA; 2Michigan State University, Grand Rapids, Michigan, USA; 3Wayne State University School of Medicine, Detroit, Michigan, USA Purpose: Approximately 5%-10% of fractures will have healing complications of nonunion or malunion. Altered bone metabolism is one of many contributing factors to abnormal bone healing. Trauma patients may have many of the risk factors for osteoporosis which when combined with a high-impact injury can lead to poor fracture healing. The purpose of this study was to determine fracture healing complications following high-energy trauma in those who have had bone health follow-up. Methods: From 2011 through 2012, 522 consecutive adults with high-energy trauma frac- tures received treatment in a Level I trauma center, were seen in an outpatient clinic for bone health, and retrospectively evaluated. 96 patients were excluded due to insufficient chart data, resulting in 426 patients in the study. Patients had a full workup consisting of mechanism of traumatic fracture(s), radiologic determination of healing, health and medi- cation history, physical examination, bone health laboratory values drawn inpatient, and dual x-ray absorptiometry (DXA) outpatient when physically feasible. Vitamin D 50,000 IU was given following trauma presentation prior to initial laboratory draw and continued maintenance dose was dependent on laboratory results. Individualized bone health life- style behavioral counseling, treatment and prescription were provided as indicated. -

Nephrology II BONE METABOLISM and DISEASE in CHRONIC KIDNEY DISEASE
Nephrology II BONE METABOLISM AND DISEASE IN CHRONIC KIDNEY DISEASE Sarah R. Tomasello, Pharm.D., BCPS Reviewed by Joanna Q. Hudson, Pharm.D., BCPS; and Lisa C. Hutchison, Pharm.D., MPH, BCPS aluminum toxicity. Adynamic bone disease is referred to as Learning Objectives low turnover disease with normal mineralization. This disorder may be caused by excessive suppression of PTH 1. Analyze the alterations in phosphorus, calcium, vitamin through the use of vitamin D agents, calcimimetics, or D, and parathyroid hormone regulation that occur in phosphate binders. In addition to bone effects, alterations in patients with chronic kidney disease (CKD). calcium, phosphorus, vitamin D and PTH cause other 2. Classify the type of bone disease that occurs in patients deleterious consequences in patients with CKD. Of these, with CKD based on the evaluation of biochemical extra-skeletal calcification and increased left ventricular markers. mass have been documented and directly correlated to an 3. Construct a therapeutic plan individualized for the stage increase in cardiovascular morbidity and mortality. The goal of CKD to monitor bone metabolism and the effects of of treatment in patients with CKD and abnormalities of bone treatment. metabolism is to normalize mineral metabolism, prevent 4. Assess the role of various treatment options such as bone disease, and prevent extraskeletal manifestations of the phosphorus restriction, phosphate binders, calcium altered biochemical processes. supplements, vitamin D agents, and calcimimetics In 2003, a non-profit international organization, Kidney based on the pathophysiology of the disease state. Disease: Improving Global Outcomes, was created. Their 5. Devise a therapeutic plan for a specific patient with mission is to improve care and outcomes for patients with alterations of phosphorus, calcium, vitamin D, and CKD worldwide by promoting, coordinating, collaborating, intact parathyroid hormone concentrations. -

Crystal Deposition in Hypophosphatasia: a Reappraisal
Ann Rheum Dis: first published as 10.1136/ard.48.7.571 on 1 July 1989. Downloaded from Annals of the Rheumatic Diseases 1989; 48: 571-576 Crystal deposition in hypophosphatasia: a reappraisal ALEXIS J CHUCK,' MARTIN G PATTRICK,' EDITH HAMILTON,' ROBIN WILSON,2 AND MICHAEL DOHERTY' From the Departments of 'Rheumatology and 2Radiology, City Hospital, Nottingham SUMMARY Six subjects (three female, three male; age range 38-85 years) with adult onset hypophosphatasia are described. Three presented atypically with calcific periarthritis (due to apatite) in the absence of osteopenia; two had classical presentation with osteopenic fracture; and one was the asymptomatic father of one of the patients with calcific periarthritis. All three subjects over age 70 had isolated polyarticular chondrocalcinosis due to calcium pyrophosphate dihydrate crystal deposition; four of the six had spinal hyperostosis, extensive in two (Forestier's disease). The apparent paradoxical association of hypophosphatasia with calcific periarthritis and spinal hyperostosis is discussed in relation to the known effects of inorganic pyrophosphate on apatite crystal nucleation and growth. Hypophosphatasia is a rare inherited disorder char- PPi ionic product, predisposing to enhanced CPPD acterised by low serum levels of alkaline phos- crystal deposition in cartilage. copyright. phatase, raised urinary phosphoethanolamine Paradoxical presentation with calcific peri- excretion, and increased serum and urinary con- arthritis-that is, excess apatite, in three adults with centrations -

Osteoporosis/Bone Health in Adults As a National Public Health Priority
Position Statement Osteoporosis/Bone Health in Adults as a National Public Health Priority This Position Statement was developed as an educational tool based on the opinion of the authors. It is not a product of a systematic review. Readers are encouraged to consider the information presented and reach their own conclusions. Osteoporosis is a widespread metabolic bone disease characterized by decreased bone mass and poor bone quality. It leads to an increased frequency of fractures of the hip, spine, and wrist. Osteoporosis is a global public health problem currently affecting more than 200 million people worldwide. In the United States alone, 10 million people have osteoporosis, and 18 million more are at risk of developing the disease. Another 34 million Americans are at risk of osteopenia, or low bone mass, which can lead to fractures and other complications. Low bone mass is a growing global health burden, and likely reflects only a small part of the true burden of osteoporosis, given that bone mineral density (BMD) does not indicate other important components of bone strength. Fragility fractures have a morbidity and mortality related to them that may be avoided more effectively if information is provided in clinical and public health prevention and management programs.14 Eighty percent of people who suffer osteoporosis are females.1 Although more commonly seen in females, osteoporosis in males remains underdiagnosed and underreported.8 The lifetime risk for fracture may be rising in certain populations, specifically Hispanic females. According to the 2004 Surgeon General's Report on Bone Health and Osteoporosis, the prevalence of osteoporosis in Hispanic females is similar to that found in Caucasian females.