Movantik) Reference Number: CP.PMN.171 Effective Date: 12.01.18 Last Review Date: 11.20 Line of Business: Medicaid Revision Log
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Naloxegol (Movantik) Reference Number: ERX.NSMN.02 Effective Date: 07/16 Last Review Date: 03/16
Clinical Policy: naloxegol (Movantik) Reference Number: ERX.NSMN.02 Effective Date: 07/16 Last Review Date: 03/16 Clinical policies are intended to be reflective of current scientific research and clinical thinking. This policy is current at the time of approval, may be updated and therefore is subject to change. This Clinical Policy is not intended to dictate to providers how to practice medicine, nor does it constitute a contract or guarantee regarding payment or results. Providers are expected to exercise professional medical judgment in providing the most appropriate care, and are solely responsible for the medical advice and treatment of members. This policy is the property of Envolve Pharmacy Solutions. Unauthorized copying, use, and distribution of this Policy or any information contained herein is strictly prohibited. By accessing this policy, you agree to be bound by the foregoing terms and conditions, in addition to the Site Use Agreement for Health Plans associated with Envolve Pharmacy Solutions. Description The intent of the criteria is to ensure that patients follow selection elements established by Envolve Pharmacy Solutions for the use of naloxegol (MovantikTM). Policy/Criteria It is the policy of health plans affiliated with Envolve Pharmacy Solutions that naloxegol (Movantik) is medically necessary for members meeting the following criteria: Initial Approval Criteria: I. Opioid-Induced Constipation (OIC) (must meet all) A. Age is ≥ 18 years old; B. Diagnosis of opioid-induced constipation; C. Member has used an opioid analgesic ≥ 4 weeks; D. Member is not being treated for cancer pain; E. Member has failed ≥ 2 non-bulk forming laxatives (see Table A) from different classes while on opioid therapy, unless contraindicated; F. -

204760Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204760Orig1s000 OTHER REVIEW(S) MEMORANDUM DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH DATE: September 16, 2014 FROM: Julie Beitz, MD SUBJECT: Approval Action TO: NDA 204760 Movantik (naloxegol) tablets AstraZeneca Pharmaceuticals LP Summary Naloxegol is an antagonist of opioid binding at the muͲopioid receptor. When administered at the recommended dose levels, naloxegol functions as a peripherallyͲacting opioid receptor antagonist in tissues such as the gastrointestinal tract, thereby decreasing the constipating effects of opioids. Naloxegol is a PEGylated derivative of naloxone and a new molecular entity. Pegylation confers the following properties: naloxegol has reduced passive permeability across membranes compared to naloxone; naloxegol is a PͲglycoprotein (PͲgp) efflux transporter substrate; and naloxegol is orally bioavailable. The reduced passive permeability and PͲgp efflux transporter properties limit CNS entry of naloxegol compared to naloxone. This memo documents my concurrence with the Division of Gastroenterology and Inborn Errors Product’s recommendation for approval of NDA 204760 for Movantik (naloxegol) tablets for the treatment of opioidͲinduced constipation (OIC) in adult patients with chronic nonͲcancer pain. Discussions regarding product labeling, and postmarketing study requirements and commitments have been satisfactorily completed. There are no inspectional issues that preclude approval. Dosing The recommended dose of Movantik (naloxegol) tablets is 25 mg taken once daily in the morning on an empty stomach. Patients who do not tolerate this dose, may reduce the dose to 12.5 mg once daily. Maintenance laxatives should be discontinued prior to initiation of therapy with Movantik. -

Design and Synthesis of Cyclic Analogs of the Kappa Opioid Receptor Antagonist Arodyn
Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn By © 2018 Solomon Aguta Gisemba Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Dr. Michael Rafferty Dr. Teruna Siahaan Dr. Thomas Tolbert Date Defended: 18 April 2018 The dissertation committee for Solomon Aguta Gisemba certifies that this is the approved version of the following dissertation: Design and synthesis of cyclic analogs of the kappa opioid receptor antagonist arodyn Chair: Dr. Blake Peterson Co-Chair: Dr. Jane Aldrich Date Approved: 10 June 2018 ii Abstract Opioid receptors are important therapeutic targets for mood disorders and pain. Kappa opioid receptor (KOR) antagonists have recently shown potential for treating drug addiction and 1,2,3 4 8 depression. Arodyn (Ac[Phe ,Arg ,D-Ala ]Dyn A(1-11)-NH2), an acetylated dynorphin A (Dyn A) analog, has demonstrated potent and selective KOR antagonism, but can be rapidly metabolized by proteases. Cyclization of arodyn could enhance metabolic stability and potentially stabilize the bioactive conformation to give potent and selective analogs. Accordingly, novel cyclization strategies utilizing ring closing metathesis (RCM) were pursued. However, side reactions involving olefin isomerization of O-allyl groups limited the scope of the RCM reactions, and their use to explore structure-activity relationships of aromatic residues. Here we developed synthetic methodology in a model dipeptide study to facilitate RCM involving Tyr(All) residues. Optimized conditions that included microwave heating and the use of isomerization suppressants were applied to the synthesis of cyclic arodyn analogs. -

Moventig, INN-Naloxegol
Package leaflet: Information for the patient Moventig 12.5 mg film-coated tablets Moventig 25 mg film-coated tablets naloxegol Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor, pharmacist or nurse. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Moventig is and what it is used for 2. What you need to know before you take Moventig 3. How to take Moventig 4. Possible side effects 5. How to store Moventig 6. Contents of the pack and other information 1. What Moventig is and what it is used for Moventig contains the active substance naloxegol. It is a medicine used in adults to treat constipation specifically caused by pain medicines, called opioids, (e.g. morphine, oxycodone, fentanyl, tramadol, codeine) taken on a regular basis. It is used when laxatives have not provided acceptable relief of constipation. Constipation related to opioids can result in symptoms such as: • stomach pain • rectal straining (having to push very hard to move the stool out of the rectum, which can also cause pain in the anus during pushing) • hard stools (stools which are hard “like a rock”) • incomplete emptying of the rectum (after having a bowel movement, the feeling as if a stool is still in the rectum which needs to come out) In patients taking opioids with constipation, who have tried at least one laxative and had incomplete relief of constipation, Moventig has been shown in clinical trials to increase the number of bowel movements and improve symptoms of constipation caused by opioids. -
Methylnaltrexone Nonf
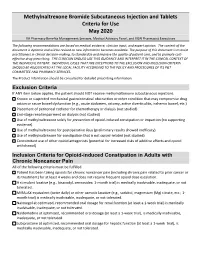
Methylnaltrexone Bromide Subcutaneous Injection and Tablets Criteria for Use May 2020 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The following recommendations are based on medical evidence, clinician input, and expert opinion. The content of the document is dynamic and will be revised as new information becomes available. The purpose of this document is to assist practitioners in clinical decision-making, to standardize and improve the quality of patient care, and to promote cost- effective drug prescribing. THE CLINICIAN SHOULD USE THIS GUIDANCE AND INTERPRET IT IN THE CLINICAL CONTEXT OF THE INDIVIDUAL PATIENT. INDIVIDUAL CASES THAT ARE EXCEPTIONS TO THE EXCLUSION AND INCLUSION CRITERIA SHOULD BE ADJUDICATED AT THE LOCAL FACILITY ACCORDING TO THE POLICY AND PROCEDURES OF ITS P&T COMMITTEE AND PHARMACY SERVICES. The Product Information should be consulted for detailed prescribing information. Exclusion Criteria If ANY item below applies, the patient should NOT receive methylnaltrexone subcutaneous injections. Known or suspected mechanical gastrointestinal obstruction or other condition that may compromise drug action or cause bowel dysfunction (e.g., acute abdomen, ostomy, active diverticulitis, ischemic bowel, etc.) Placement of peritoneal catheter for chemotherapy or dialysis (not studied) End-stage renal impairment on dialysis (not studied) Use of methylnaltrexone solely for prevention of opioid-induced constipation or impaction (no supporting evidence). Use of methylnaltrexone for postoperative ileus (preliminary results showed inefficacy). Use of methylnaltrexone for constipation that is not opioid-related (not studied) Concomitant use of other opioid antagonists (potential for increased risks of additive effects and opioid withdrawal) Inclusion Criteria for Opioid-induced Constipation in Adults with Chronic Noncancer Pain All of the following criteria must be fulfilled. -

Prescriber Update Vo.39 No.2. June 2018
Prescriber Update Vol. 39 No. 2 June 2018 www.medsafe.govt.nz ISSN 1172-5648 (print) ISSN 1179-075X (online) Contents Spotlight on Codeine 18 Making Medicines Safer: New e-Learning Module on Reporting Adverse Reactions Launched 19 Tenofovir Disoproxil – a Salty Tale 20 Medicines Interacting with Methadone 20 Hyoscine Butylbromide Injection and Cardiovascular Adverse Reactions 22 Using New Zealand Data to Review the Risk of Venous Thromboembolism with Combined Oral Contraceptives 23 Hypocalcaemia – a Risk with Zoledronic Acid 24 Pharmacogenomics – Helps Reduce Rash Decisions 25 MARC’s Remarks: March 2018 Meeting 27 Gathering Knowledge from Adverse Reaction Reports: June 2018 28 Medicines Monitoring: Dabigatran and gout or gout-like symptoms 29 Recent Approvals of Medicines Containing a New Active Ingredient 29 The Medsafe Files – Episode Six: Global Pharmacovigilance 29 Correction: Adverse Reaction Reporting in New Zealand – 2017 30 Medicine Classification Update – November 2017 31 Quarterly Summary of Recent Safety Communications 31 Report Adverse Drug Reactions 31 Subscribe to Prescriber Update 32 Spotlight on Codeine Key Messages phenotypes varies between populations. The relative frequencies of these phenotypes in the z The following patients should not use New Zealand population are not known. codeine as the risks of harm outweigh Poor metabolisers are unable to convert codeine any benefit: to morphine and receive little if any, analgesic – children aged under 12 years benefit. Extensive metabolisers convert 5–15% – adolescents aged under 18 years: for of codeine to morphine via the CYP2D6 enzyme. pain following surgery to remove In these patients, a 30 mg dose of codeine tonsils or adenoids, for symptomatic phosphate would yield approximately 1.5 mg to relief of cough, or in patients whose 4.5 mg of morphine. -

Oncology & Haematology
Oncology & Haematology Specialist Formulary List – NON-CHEMOTHERAPY DRUGS **Other indications for particular drugs may be included on completion of further specialist lists** For information on use of unlicensed medicines or medicines used 'off-label' - click here The following medicines are approved for prescribing by or on the recommendation of a prescribing oncology or haematology specialist (including non-medical prescribers where appropriate): In the event of a broken link please forward details to [email protected] Please include the location and full title of the link MEDICINE SUMMARY OF RESTRICTED INDICATION CATEGORY PROTOCOL Aprepitant capsules Adjunct to dexamethasone and a 5HT3-receptor antagonist NOSCAN (North of Scotland Cancer in preventing nausea and vomiting associated with cisplatin Network) Antiemetic Protocol pending. containing chemotherapy regimes. Granisetron tablets, injection Chemotherapy-induced nausea and vomiting (2nd line). Prophylaxis of Chemotherapy Induced Usually given pre-chemotherapy. Nausea and Vomiting follow MASCC guidelines Levomepromazine tablets, injection Chemotherapy-induced nausea and vomiting (3rd line). www.mascc.org 6mg tablets available. Tablets may be halved. Usual dose 3mg or 6mg twice daily. Lorazepam tablets, injection Anticipatory nausea and vomiting. 0.5mg to 1mg the night before and morning of chemotherapy. Palonosetron Injection Chemotherapy-induced nausea and vomiting. Given as a single dose IV pre-chemotherapy Granisetron transdermal patch Prevention of nausea and vomiting -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

208854Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208854Orig1s000 SUMMARY REVIEW OND=Office of New Drugs OPQ=Office of Pharmaceutical Quality OPDP=Office of Prescription Drug Promotion OSI=Office of Scientific Investigations CDTL=Cross-Discipline Team Leader COA=Clinical Outcome Assessment CSS=Controlled Substance Staff DAAAP= Division of Anesthesia, Analgesia, and Addiction Products OSE= Office of Surveillance and Epidemiology DEPI= Division of Epidemiology DMEPA=Division of Medication Error Prevention and Analysis DPMH = Division of Pediatric and Maternal Health MHT=Maternal Health Team Quality Review Team DISCIPLINE REVIEWER BRANCH/DIVISION Drug Substance Joseph Leginus CDER/OPQ/ONDP/ DNDAPI/NDBII Drug Product Sarah Ibrahim CDER/OPQ/ONDP/ DNDPII/NDPBV Process Zhao Wang CDER/OPQ/OPF/ DPAI/PABI Microbiology Zhao Wang CDER/OPQ/OPF/ DPAI/PABI Facility Donald Lech CDER/OPQ/OPF/DIA/IABIII Biopharmaceutics Peng Duan CDER/OPQ/ONDP/ DB/BBII Regulatory Business Cheronda Cherry-France CDER/OND/ODEIII/ DGIEP Process Manager Application Technical Lead Hitesh Shroff CDER/OPQ/ONDP/ DNDPII/NDPBV Laboratory (OTR) N/A N/A ORA Lead Paul Perdue Jr. ORA/OO/OMPTO/ DMPTPO/MDTP Environmental Analysis James Laurenson CDER/OPQ/ONDP (EA) 2 Reference ID: 4073992 1. Benefit-Risk Assessment I concur with the reviewers’ conclusions that the benefit/risk of naldemedine is favorable in the population for which this product will be approved and that the risks can be managed with labeling. The applicant proposed the following indication for naldemedine, an orally administered peripheral mu opioid receptor antagonist: Symproic is indicated for the treatment of opioid-induced constipation (OIC) in adult patients with chronic non-cancer pain. -

Moventig, INN-Naloxegol
25 September 2014 EMA/CHMP/738815/2014 Committee for Medicinal Products for Human Use (CHMP) Assessment report Moventig International non-proprietary name: naloxegol Procedure No. EMEA/H/C/002810/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5520 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2014. Reproduction is authorised provided the source is acknowledged. Administrative information Name of the medicinal product: Moventig Applicant: AstraZeneca AB SE-151 85 Södertälje Sweden Active substance: naloxegol oxalate International Nonproprietary Name/Common naloxegol Name: Pharmaco-therapeutic group Drugs for constipation (ATC Code): (A06AH03) Therapeutic indication(s): Moventig is indicated for the treatment of opioid-induced constipation (OIC) in adult patients who have had an inadequate response to laxative(s). Pharmaceutical form: Film-coated tablet Strengths: 12.5 mg and 25 mg Route of administration: Oral use Packaging: Blister 12.5 mg: Package sizes: 30 (3x10) tablets, 90 (9x10) tablets and 90 x 1 tablets (unit dose) 25mg: 10 (1x10) tablets, 30 (3x10) tablets, 90 (9x10) tablets and 90 x 1 tablets (unit dose) Assessment report EMA/CHMP/738815/2014 Page 2/120 Table of contents 1. Background information on the procedure .............................................. 9 1.1. Submission of the dossier ...................................................................................... 9 1.2. Manufacturers .................................................................................................... 10 1.3. Steps taken for the assessment of the product ....................................................... 10 2. Scientific discussion .............................................................................. 12 2.1. -

MOVANTIK Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION • Concomitant use with strong CYP3A4 inhibitors (e.g., clarithromycin, These highlights do not include all the information needed to use ketoconazole) (4, 7.1) MOVANTIK safely and effectively. See full prescribing information for • Known serious or severe hypersensitivity reaction to MOVANTIK or MOVANTIK. any of its excipients (4) MOVANTIK® (naloxegol) tablets, for oral use ----------------------- WARNINGS AND PRECAUTIONS --------------------- Initial U.S. Approval: 2014 • Opioid withdrawal: Consider the overall risk benefit in patients with disruptions to the blood-brain barrier. Monitor for symptoms of opioid withdrawal (5.1) --------------------------RECENT MAJOR CHANGES ------------------------ Indications and Usage (1) 08/2017 • Severe abdominal pain and/or diarrhea: Monitor for the development of symptoms after initiating treatment with MOVANTIK and discontinue if --------------------------- INDICATIONS AND USAGE ------------------------- severe symptoms develop. Consider restarting MOVANTIK at 12.5 mg MOVANTIK is an opioid antagonist indicated for the treatment of opioid- once daily if appropriate (5.2) induced constipation (OIC) in adult patients with chronic non-cancer pain, • Gastrointestinal perforation: Consider the overall risk benefit in patients including patients with chronic pain related to prior cancer or its treatment with known or suspected lesions of the GI tract. Monitor for severe, who do not require frequent (e.g., weekly) opioid dosage escalation (1) persistent or worsening -

OUH Formulary Approved for Use in Breast Surgery
Oxford University Hospitals NHS Foundation Trust Formulary FORMULARY (Y): the medicine can be used as per its licence. RESTRICTED FORMULARY (R): the medicine can be used as per the agreed restriction. NON-FORMULARY (NF): the medicine is not on the formulary and should not be used unless exceptional approval has been obtained from MMTC. UNLICENSED MEDICINE – RESTRICTED FORMULARY (UNR): the medicine is unlicensed and can be used as per the agreed restriction. SPECIAL MEDICINE – RESTRICTED FORMULARY (SR): the medicine is a “special” (unlicensed) and can be used as per the agreed restriction. EXTEMPORANEOUS PREPARATION – RESTRICTED FORMULARY (EXTR): the extemporaneous preparation (unlicensed) can be prepared and used as per the agreed restriction. UNLICENSED MEDICINE – NON-FORMULARY (UNNF): the medicine is unlicensed and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. SPECIAL MEDICINE – NON-FORMULARY (SNF): the medicine is a “special” (unlicensed) and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. EXTEMPORANEOUS PREPARATION – NON-FORMULARY (EXTNF): the extemporaneous preparation (unlicensed) cannot be prepared and used unless exceptional approval has been obtained from MMTC. CLINICAL TRIALS (C): the medicine is clinical trial material and is not for clinical use. NICE TECHNOLOGY APPRAISAL (NICETA): the medicine has received a positive appraisal from NICE. It will be available on the formulary from the day the Technology Appraisal is published. Prescribers who wish to treat patients who meet NICE criteria, will have access to these medicines from this date. However, these medicines will not be part of routine practice until a NICE TA Implementation Plan has been presented and approved by MMTC (when the drug will be given a Restricted formulary status).