MLN Connects for Thursday, October 17, 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Dance Division Calendar 17-18
Early Dance Division 2017-2018 Session 1 September 9 – November 3 Monday Classes Tuesday Classes September 11 Class September 12 Class September 18 Class September 19 Class September 25 Class September 26 Class October 2 Class October 3 Class October 9 Class October 10 Class October 16 Class October 17 Class October 23 Class October 24 Class October 30 Last Class October 31 Last Class Wednesday Classes Thursday Classes September 13 Class September 14 Class September 20 Class September 21* Class September 27 Class September 28 Class October 4 Class October 5 Class October 11 Class October 12 Class October 18 Class October 19 Class October 25 Class October 26 Class November 1 Last Class November 2 Last Class Saturday Classes Sunday Classes September 9 Class September 10 Class September 16 Class September 17 Class September 23 Class September 24 Class September 30* Class October 1 Class October 7 Class October 8 Class October 14 Class October 15 Class October 21 Class October 22 Class October 28 Last Class October 29 Last Class *Absences due to the holiday will be granted an additional make-up class. Early Dance Division 2017-2018 Session 2 November 4 – January 22 Monday Classes Tuesday Classes November 6 Class November 7 Class November 13 Class November 14 Class November 20 No Class November 21 No Class November 27 Class November 28 Class December 4 Class December 5 Class December 11 Class December 12 Class December 18 Class December 19 Class December 25 No Class December 26 No Class January 1 No Class January 2 No Class January 8 Class -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -
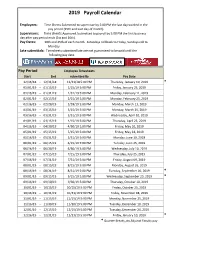
2019 Payroll Calendar
2019 Payroll Calendar Employees: Time Sheets Submitted to supervisor by 5:00 PM the last day worked in the pay period (15th and Last day of month). Supervisors: Time sheets Approved /submitted to payroll by 5:00 PM the first business day after pay period ends (1st and 16th). Pay Dates: 10th and 25th of each month. Saturdays roll back to Friday, Sundays roll to Monday. Late submittals: Timesheets submitted late are not guaranteed to be paid until the following pay date. Pay Period Employee Timesheets Start End submitted By Pay Date 12/16/18 - 12/31/18 12/31/18 5:00 PM Thursday, January 10, 2019 * 01/01/19 - 01/15/19 1/15/19 5:00 PM Friday, January 25, 2019 01/16/19 - 01/31/19 1/31/19 5:00 PM Monday, February 11, 2019 02/01/19 - 02/15/19 2/15/19 5:00 PM Monday, February 25, 2019 02/16/19 - 02/28/19 2/28/19 5:00 PM Monday, March 11, 2019 03/01/19 - 03/15/19 3/15/19 5:00 PM Monday, March 25, 2019 03/16/19 - 03/31/19 3/31/19 5:00 PM Wednesday, April 10, 2019 04/01/19 - 04/15/19 4/15/19 5:00 PM Thursday, April 25, 2019 04/16/19 - 04/30/19 4/30/19 5:00 PM Friday, May 10, 2019 05/01/19 - 05/15/19 5/15/19 5:00 PM Friday, May 24, 2019 05/16/19 - 05/31/19 5/31/19 5:00 PM Monday, June 10, 2019 06/01/19 - 06/15/19 6/15/19 5:00 PM Tuesday, June 25, 2019 06/16/19 - 06/30/19 6/30/19 5:00 PM Wednesday, July 10, 2019 07/01/19 - 07/15/19 7/15/19 5:00 PM Thursday, July 25, 2019 07/16/19 - 07/31/19 7/31/19 5:00 PM Friday, August 09, 2019 08/01/19 - 08/15/19 8/15/19 5:00 PM Monday, August 26, 2019 08/16/19 - 08/31/19 8/31/19 5:00 PM Tuesday, September 10, -

Salary Payroll Schedule - 2021 Fiscal Pay Salary Overtime &Retro Leave Semester Pay Period HR Transaction Deadline Payday Days Year Number Entry (PHAHOUR) Periods
Salary Payroll Schedule - 2021 Fiscal Pay Salary Overtime &Retro Leave Semester Pay Period HR Transaction deadline Payday Days Year Number Entry (PHAHOUR) Periods December 25 – January 9 1 Monday, January 4, 2021 Wednesday, January 6, 2021 Friday, January 15, 2021 11 12 January 10 – January 24 2 Tuesday, January 19, 2021 Thursday, January 21, 2021 Monday, February 1, 2021 10 1 January 25 – February 9 3 Tuesday, February 2, 2021 Thursday, February 4, 2021 Tuesday, February 16, 2021 12 February 10 – February 24 4 Tuesday, February 16, 2021 Thursday, February 18, 2021 Monday, March 1, 2021 11 Spring Semester 2 Classes Begin February 25 – March 9 5 Wednesday, March 3, 2021 Friday, March 5, 2021 Tuesday, March 16, 2021 9 1/19/21 Exams End 5/13/21 21 March 10 – March 24 6 Thursday, March 18, 2021 Monday, March 22, 2021 Wednesday, March 31, 2021 11 3 March 25 – April 9 7 Monday, April 5, 2021 Wednesday, April 7, 2021 Friday, April 16, 2021 12 April 10 – April 24 8 Monday, April 19, 2021 Wednesday, April 21, 2021 Friday, April 30, 2021 10 4 April 25 – May 9 9 Monday, May 3, 2021 Wednesday, May 5, 2021 Friday, May 14, 2021 10 May 10 – May 24 10 Tuesday, May 18, 2021 Thursday, May 20, 2021 Tuesday, June 1, 2021 11 Summer I 5 Classes Begin May 25 – June 9 11 Thursday, June 3, 2021 Monday, June 7, 2021 Wednesday, June 16, 2021 12 5/24/21 (Paid 7/1/21) June 10 – June 24 12 Friday, June 18, 2021 Tuesday, June 22, 2021 Thursday, July 1, 2021 11 6 June 25 – July 9 13 Friday, July 2, 2021 Wednesday, July 7, 2021 Friday, July 16, 2021 11 Summer II Classes -

2021 Daily 10 October
October 2021 Daily Lectionary These Scripture readings are from the two-year daily lectionary of the Presbyterian Book of Common Worship (Westminster John Knox Press, 2018). The readings from the three-year Revised Common Lectionary for Sundays and Festivals are not included in this document. Friday, October 1 Thursday, October 7 Wednesday, October 13 Morning: Pss. 84; 148 Morning: Pss. 97; 147:12–20 Morning: Pss. 15; 147:1–11 Evening: Pss. 25; 40 Evening: Pss. 16; 62 Evening: Pss. 48; 4 2 Kings 19:1–20 2 Kings 23:4–25 Jer. 37:3–21 1 Cor. 9:16–27 1 Cor. 12:1–11 1 Cor. 14:13–25 Matt. 8:1–17 Matt. 9:18–26 Matt. 10:24–33 Saturday, October 2 Friday, October 8 Thursday, October 14 Morning: Pss. 63; 149 Morning: Pss. 51; 148 Morning: Pss. 36; 147:12–20 Evening: Pss. 125; 90 Evening: Pss. 142; 65 Evening: Pss. 80; 27 2 Kings 19:21–36 2 Kings 23:36–24:17 Jer. 38:1–13 1 Cor. 10:1–13 1 Cor. 12:12–26 1 Cor. 14:26–33a Matt. 8:18–27 Matt. 9:27–34 (33b–36) 37–40 Matt. 10:34–42 Sunday, October 3 Saturday, October 9 Morning: Pss. 103; 150 Morning: Pss. 104; 149 Friday, October 15 Evening: Pss. 117; 139 Evening: Pss. 138; 98 Morning: Pss. 130; 148 2 Kings 20:1–21 Jer. 35:1–19 Evening: Pss. 32; 139 Acts 12:1–17 1 Cor. 12:27–13:3 Jer. 38:14–28 Luke 7:11–17 Matt. -
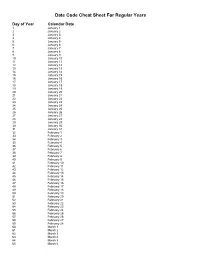
Julian Date Cheat Sheet for Regular Years
Date Code Cheat Sheet For Regular Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 March 1 61 March 2 62 March 3 63 March 4 64 March 5 65 March 6 66 March 7 67 March 8 68 March 9 69 March 10 70 March 11 71 March 12 72 March 13 73 March 14 74 March 15 75 March 16 76 March 17 77 March 18 78 March 19 79 March 20 80 March 21 81 March 22 82 March 23 83 March 24 84 March 25 85 March 26 86 March 27 87 March 28 88 March 29 89 March 30 90 March 31 91 April 1 92 April 2 93 April 3 94 April 4 95 April 5 96 April 6 97 April 7 98 April 8 99 April 9 100 April 10 101 April 11 102 April 12 103 April 13 104 April 14 105 April 15 106 April 16 107 April 17 108 April 18 109 April 19 110 April 20 111 April 21 112 April 22 113 April 23 114 April 24 115 April -

Pay Date Calendar
Pay Date Information Select the pay period start date that coincides with your first day of employment. Pay Period Pay Period Begins (Sunday) Pay Period Ends (Saturday) Official Pay Date (Thursday)* 1 January 10, 2016 January 23, 2016 February 4, 2016 2 January 24, 2016 February 6, 2016 February 18, 2016 3 February 7, 2016 February 20, 2016 March 3, 2016 4 February 21, 2016 March 5, 2016 March 17, 2016 5 March 6, 2016 March 19, 2016 March 31, 2016 6 March 20, 2016 April 2, 2016 April 14, 2016 7 April 3, 2016 April 16, 2016 April 28, 2016 8 April 17, 2016 April 30, 2016 May 12, 2016 9 May 1, 2016 May 14, 2016 May 26, 2016 10 May 15, 2016 May 28, 2016 June 9, 2016 11 May 29, 2016 June 11, 2016 June 23, 2016 12 June 12, 2016 June 25, 2016 July 7, 2016 13 June 26, 2016 July 9, 2016 July 21, 2016 14 July 10, 2016 July 23, 2016 August 4, 2016 15 July 24, 2016 August 6, 2016 August 18, 2016 16 August 7, 2016 August 20, 2016 September 1, 2016 17 August 21, 2016 September 3, 2016 September 15, 2016 18 September 4, 2016 September 17, 2016 September 29, 2016 19 September 18, 2016 October 1, 2016 October 13, 2016 20 October 2, 2016 October 15, 2016 October 27, 2016 21 October 16, 2016 October 29, 2016 November 10, 2016 22 October 30, 2016 November 12, 2016 November 24, 2016 23 November 13, 2016 November 26, 2016 December 8, 2016 24 November 27, 2016 December 10, 2016 December 22, 2016 25 December 11, 2016 December 24, 2016 January 5, 2017 26 December 25, 2016 January 7, 2017 January 19, 2017 1 January 8, 2017 January 21, 2017 February 2, 2017 2 January -

2021 Calendar Campaign
One Tail at a Time 2021 Calendar Pets Date Status Date Status Date Status Date Status Date Status Date Status Date Status Date Status Friday, January 1 Not Available Saturday, February 20 Not Available Sunday, April 11 Available Monday, May 31 Not Available Tuesday, July 20 Available Wednesday, September 8 Not Available Thursday, October 28 Available Thursday, December 16 Available Saturday, January 2 Available Sunday, February 21 Available Monday, April 12 Not Available Tuesday, June 1 Available Wednesday, July 21 Not Available Thursday, September 9 Available Friday, October 29 Available Friday, December 17 Available Sunday, January 3 Available Monday, February 22 Available Tuesday, April 13 Available Wednesday, June 2 Available Thursday, July 22 Not Available Friday, September 10 Available Saturday, October 30 Available Saturday, December 18 Not Available Monday, January 4 Available Tuesday, February 23 Available Wednesday, April 14 Available Thursday, June 3 Available Friday, July 23 Available Saturday, September 11 Available Sunday, October 31 Not Available Sunday, December 19 Available Tuesday, January 5 Available Wednesday, February 24 Available Thursday, April 15 Not Available Friday, June 4 Available Saturday, July 24 Available Sunday, September 12 Available Monday, November 1 Available Monday, December 20 Available Wednesday, January 6 Available Thursday, February 25 Available Friday, April 16 Not Available Saturday, June 5 Available Sunday, July 25 Available Monday, September 13 Available Tuesday, November 2 Available Tuesday, -

Due Date Chart 201803281304173331.Xlsx
Special Event Permit Application Due Date Chart for Events from January 1, 2019 - June 30, 2020 If due date lands on a Saturday or Sunday, the due date is moved to the next business day Event Date 30 Calendar days 90 Calendar Days Tuesday, January 01, 2019 Sunday, December 02, 2018 Wednesday, October 03, 2018 Wednesday, January 02, 2019 Monday, December 03, 2018 Thursday, October 04, 2018 Thursday, January 03, 2019 Tuesday, December 04, 2018 Friday, October 05, 2018 Friday, January 04, 2019 Wednesday, December 05, 2018 Saturday, October 06, 2018 Saturday, January 05, 2019 Thursday, December 06, 2018 Sunday, October 07, 2018 Sunday, January 06, 2019 Friday, December 07, 2018 Monday, October 08, 2018 Monday, January 07, 2019 Saturday, December 08, 2018 Tuesday, October 09, 2018 Tuesday, January 08, 2019 Sunday, December 09, 2018 Wednesday, October 10, 2018 Wednesday, January 09, 2019 Monday, December 10, 2018 Thursday, October 11, 2018 Thursday, January 10, 2019 Tuesday, December 11, 2018 Friday, October 12, 2018 Friday, January 11, 2019 Wednesday, December 12, 2018 Saturday, October 13, 2018 Saturday, January 12, 2019 Thursday, December 13, 2018 Sunday, October 14, 2018 Sunday, January 13, 2019 Friday, December 14, 2018 Monday, October 15, 2018 Monday, January 14, 2019 Saturday, December 15, 2018 Tuesday, October 16, 2018 2019 Tuesday, January 15, 2019 Sunday, December 16, 2018 Wednesday, October 17, 2018 Wednesday, January 16, 2019 Monday, December 17, 2018 Thursday, October 18, 2018 Thursday, January 17, 2019 Tuesday, December 18, 2018 -

2021 Park Hours
Holiday World & Splashin' Safari 2021 Operating Calendar May, 2021 Holiday World Hours Splashin' Safari Hours Special Events Saturday, May 1 Holiday World & Splashin' Safari are closed Sunday, May 2 Holiday World & Splashin' Safari are closed Monday, May 3 Holiday World & Splashin' Safari are closed Tuesday, May 4 Holiday World & Splashin' Safari are closed Wednesday, May 5 Holiday World & Splashin' Safari are closed Thursday, May 6 Holiday World & Splashin' Safari are closed Friday, May 7 Holiday World & Splashin' Safari are closed Saturday, May 8 Platinum Season Pass Preview Day: Holiday World is open from 10 AM until 6 PM Splashin' Safari is Closed Platinum Season Passholder Party Sunday, May 9 Passholder Preview Day: Holiday World is open from 10 AM until 6 PM Splashin' Safari is Closed Monday, May 10 Holiday World & Splashin' Safari are closed Tuesday, May 11 Holiday World & Splashin' Safari are closed Wednesday, May 12 Holiday World & Splashin' Safari are closed Thursday, May 13 Holiday World & Splashin' Safari are closed Friday, May 14 Holiday World & Splashin' Safari are closed for a private outing Saturday, May 15 Holiday World is open from 10 AM until 4 PM Splashin' Safari is Closed Sunday, May 16 Holiday World is open from 10 AM until 4 PM Splashin' Safari is Closed Monday, May 17 Holiday World & Splashin' Safari are closed Tuesday, May 18 Holiday World & Splashin' Safari are closed Wednesday, May 19 Holiday World & Splashin' Safari are closed Thursday, May 20 Holiday World & Splashin' Safari are closed Friday, May 21 Holiday -

October 10, 1962 Speech by Senator Keating, "Cuba"
Digital Archive digitalarchive.wilsoncenter.org International History Declassified October 10, 1962 Speech by Senator Keating, "Cuba" Citation: “Speech by Senator Keating, "Cuba",” October 10, 1962, History and Public Policy Program Digital Archive, 87th Congress, 2nd session, Congressional Record 108, part 17 (October 10, 1962), 22957. https://digitalarchive.wilsoncenter.org/document/134657 Summary: Keating alleges that there are six IRBM bases being constructed by the Soviet Union in Cuba. Original Language: English Contents: English Transcription Scan of Original Document Mr. KEATING. Mr. President, yesterday I spoke on the subject of Cuba. At that time I did not have fully confirmed the matter to which I shall address myself now. I now have it fully confirmed. As a result, I call upon the appropriate Government officials to confirm or to deny reports of intermediate range missile bases in Cuba. Construction has begun on at least a half dozen launching sites for intermediate range tactical missiles. Intelligence authorities must have advised the President and top Government officials of this fact, and they must now have been told that ground-to-ground missiles can be operational from the island of Cuba within 6 months. My own sources on the Cuban situation, which have been 100 percent reliable, have substantiated this report completely. When are the American people going to be given all of the facts about the military buildup in Cuba? Yesterday I pointed out, for either the 19th or 20th time, that we are not getting the whole story on Cuba. I referred to the recent testimony by Under Secretary of State George Ball before the House Select Committee on Export Control. -

Vol. 84 Thursday, No. 201 October 17, 2019 Pages 55489–55858
Vol. 84 Thursday, No. 201 October 17, 2019 Pages 55489–55858 OFFICE OF THE FEDERAL REGISTER VerDate Sep 11 2014 20:51 Oct 16, 2019 Jkt 250001 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\17OCWS.LOC 17OCWS II Federal Register / Vol. 84, No. 201 / Thursday, October 17, 2019 The FEDERAL REGISTER (ISSN 0097–6326) is published daily, SUBSCRIPTIONS AND COPIES Monday through Friday, except official holidays, by the Office PUBLIC of the Federal Register, National Archives and Records Administration, under the Federal Register Act (44 U.S.C. Ch. 15) Subscriptions: and the regulations of the Administrative Committee of the Federal Paper or fiche 202–512–1800 Register (1 CFR Ch. I). The Superintendent of Documents, U.S. Assistance with public subscriptions 202–512–1806 Government Publishing Office, is the exclusive distributor of the official edition. Periodicals postage is paid at Washington, DC. General online information 202–512–1530; 1–888–293–6498 Single copies/back copies: The FEDERAL REGISTER provides a uniform system for making available to the public regulations and legal notices issued by Paper or fiche 202–512–1800 Federal agencies. These include Presidential proclamations and Assistance with public single copies 1–866–512–1800 Executive Orders, Federal agency documents having general (Toll-Free) applicability and legal effect, documents required to be published FEDERAL AGENCIES by act of Congress, and other Federal agency documents of public Subscriptions: interest. Assistance with Federal agency subscriptions: Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless the Email [email protected] issuing agency requests earlier filing.