Community Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ormond Scenic Loop & Trail
Ormond Scenic Loop & Trail Corridor Management Plan / Designation Application for the County of Volusia, Florida Submitted to Florida Department of Transportation May 2007 i Ormond Scenic Loop & Trail Corridor Management Plan Produced by the Ormond Scenic Loop & Trail Corridor Advocacy Group with assistance from GAI Consultants, Inc. MAY 2007 The Ormond Scenic Loop & Trail acknowledges the following organizations for their assistance and support throughout the development of this project: Florida Department of Transportation, District 5 County of Volusia City of Ormond Beach Heritage Crossroads: Miles of History Corridor Advocacy Group A1A Scenic & Historic Coastal Byway Florida Department of Environmental Protection Daytona Beach Community College Florida Power & Light Photographs by Skip Lowery, Rob Bird, Laura Bamberger, J. Walker Fischer, Leslie Whittaker, Richard Gardner, Scott Veix, Lou Kellenberger, Anne Barca, Charles Littlewood, the Ormond Beach Historical Trust, and the Florida Department of Environmental Protection GAI Consultants, Inc. 618 East South Street Orlando, Florida 32804 (p) 407.423.8398 (f) 407.843.1070 www.gaiconsultants.com Ormond Scenic Loop & Trail – Corridor Management Plan ii Secretary Signage Page As Secretary of the Florida Department of Transportation, the signature below indicates the approval and endorsement of this Corridor Management Plan and this corridor for designation as a Florida Scenic Highway. FDOT approval of this management plan represents our agreement to serve in a partnership with -

What Families in Transition Need to Know About Public Education PETAL
Resources for Families National Resources Volusia/Flagler County Coalition for the National Association for the Education of Homeless Homeless Children and Youth P.O. Box 444, DeLand, Florida (866) 862-2562 or www.naehcy.org (386) 279-0029 National Center for Homeless Education Florida Coalition for the Homeless (800) 308-2145 or www.serve.org/nche What Families (727) 809-1980 or www.fchonline.org National Law Center in Transition on Homelessness & Poverty HUM Center (202) 638-2535 or www.nlchp.org Need to Know 340 North Street, Daytona Beach, Florida (386) 252-9400 National Coalition for the Homeless (202) 462-4822 or about Volusia County Human Services www.nationalhomeless.org Daytona Beach – (386) 254-4675 Public Education DeLand – (386) 736-5956 New Smyrna Beach – (386) 423-3309 For more information contact: Orange City – (386) 775-5204 District Homeless Education Liaison PETAL Department of Students Services: United Way of Volusia-Flagler Counties, Inc. Jennifer Watley (386) 734-7190 x-20856 First Call for Help – 211 Halifax Area – (386) 255-6475 Southeast Area – (386) 427-5223 Florida Department of Education Westside Area – (386) 734-7190 People Experiencing Transition and Loss Homeless Education Program (850) 245-0505 Florida Department of Children The School Board of Volusia County, FL and Families Volusia County Schools www.dcf.state.fl.us/homelessness DeLand Administrative Complex Student Services & Government Affairs 1-800-962-2873 200 North Clara Avenue Department DeLand, Florida 32721 VCan 2020 People Experiencing Transition & Loss www.vcan2020.org Funding provided by McKinney-Vento of Housing (386) 999-1888 Homeless Education Assistance Act (PETAL) Program Printed June 2020 McKinney-Vento Homeless Your Children’s Rights When You Move Education Act Local school districts must ensure that homeless The federally funded McKinney-Vento Homeless Becoming homeless is highly disruptive to children and youth have equal access to a free, Education Assistance Act established educational students in many ways. -

Andrea Messina Executive Director Florida School Boards Association 203 South Monroe Street Tallahassee, Florida 32301
Andrea Messina Executive Director Florida School Boards Association 203 South Monroe Street Tallahassee, Florida 32301 Dear Ms. Messina, Please accept this letter as an application for the interim superintendent position for Volusia County Schools, Volusia County, Florida. Attached is my resume. The resume indicates my 36 years of experience for Volusia County Schools, including classroom teaching (10 years), successful school based administration (8 years) and district administrative (15 years) leadership roles. It would be an honor and privilege to serve Volusia County Schools as interim superintendent. References are available upon request. Sincerely, Timothy J. Huth TIMOTHY J. HUTH 32 MEADOW RIDGE VIEW ORMOND BEACH, FLORIDA, 32174 H-386-672-7602 C-386-214-9193 [email protected] EDUCATION: • Educational Specialist – Nova Southeastern University (Administration and Supervision). 1985 • Master of Education – University of Cincinnati, 1979 • Bachelors of Science – University of Cincinnati, 1974 • Graduate Course work – University of Florida, University of Central Florida, 2002 EMPLOYMENT HISTORY: 2010 - Present Substitute -Volusia County School Board 2010 - Present Education Consultant 1997-2010 Deputy Superintendent of Schools, Volusia County Public Schools, Deland, Florida 1995-1997 Area Superintendent of Schools, Volusia County Public Schools, Deland, Florida 1990-1995 Principal, Mainland High School, Daytona Beach, Fl. 1988-1990 Principal, Holly Hill Jr. High/Middle School, Holly Hill, Fl. 1987-1989 Assistant Principal, Holly Hill Jr. -
Memorial Service Program
A Memorial Service Honoring Those Who Left Us In The Year 2018 Florida Council of Chapters 2019 Convention hosted byTampa Chapter June 22, 2019 “On behalf of a Grateful Nation” God of the Ages God of the ages, whose almighty hand leads forth in beauty all the starry band of shining worlds in splendor through the skies, our grateful songs before thy throne arise. Thy love divine hath led us in the past; in this free land with thee our lot is cast; be thou our ruler, guardian, guide, and stay, thy Word our law, thy paths our chosen way. Refresh thy people on their toilsome way; lead us from night to never-ending day; fill all our lives with love and grace divine, and glory, laud, and praise be ever thine. Abide with Me Abide with me; fast falls the eventide; the darkness deepens; Lord, with me abide. When other helpers fail and comforts flee, Help of the helpless, O abide with me. I need thy presence every passing hour. What but thy grace can foil the temper’s power? Who like thyself, my guide and stay can be? Through cloud and sunshine, Lord, abide with me. I fear no foe, with thee at hand to bless; Ills have no weight, and tears no bitterness. Where is death’s sting? Where, grave, thy victory? I triumph still, is thou abide with me. Florida Council of Chapters Memorial Service Safety Harbor Resort and Spa 22 June 2019 PRELUDE Ginger Heath, Pianist Past President, Tampa Chapter MOWC CALL TO WORSHIP AND INVOCATION Chaplain (COL) Bernard H. -
January 2009 Inc
Volume XXXIII • Issue 1 • January, 2009 4931 South Peninsula Drive • Ponce Inlet, Florida 32127 www.ponceinlet.org • www.poncelighthousestore.org (386) 761-1821 • [email protected] © Copyright 2008 Ponce de Leon Inlet Lighthouse Preservation Association. All rights reserved. From the 2 Executive Director Events 3 Calendar Regional History 4 Maritime Commerce on the Halifax Feature Article The 6 Coasting Captain Education 8 News Lighthouses of the World Île Vierge Lighthouse Objects of the Quarter 9 Post Lantern Crossword Puzzle 10 Volunteer News Gift Shop 12 Features The Quarterly Newsletter of the Ponce de Leon Inlet LighthousePonce de Leon Preservation Inlet Light Station Association, • January 2009 Inc. From the Executive Director appy New Year, I hope this reaches all our Additional upgrades and enhancements to The Ponce de Leon Inlet Lighthouse Hmembers in good health and spirit. our onsite exhibits, community outreach programs, Preservation Association is dedicated to In keeping with an annual newsletter cover and online educational resources continue. The the preservation and dissemination of the theme started last year in celebration of our 120th Association is currently in the process of developing maritime and social history of the Ponce anniversary, this year’s newsletter covers will feature a new Science of Light educational program and de Leon Inlet Light Station. recent aerial photographs of the historic Ponce Inlet exhibit. Scheduled for completion during the 2009- Light Station. Each quarterly publication, beginning 2010 fiscal-year, this exciting program will feature 2008 Board of Trustees with last October’s issue, provides one quadrant an interactive DVD with accompanying models Robyn Hurd of stunning pictures of the tower, grounds, and and hands-on activities. -

Golden Sands
By KATHRYN ABBEY HANNA Florida, LAnd of Change (1941) Jlorida~s A one-volume history of Florida from its discovery to the present. /" GOLDEN SANDS By ALFRED JACKSON HANNA By Flight into Oblivion (1938) ALFRED JACKSON HANNA A narrative of the last days and flight of the Confederate Cabinet. \\ The St. Johns, with James Branch Cabell, in the and Rivers of America Series (1943) KATHRYN ABBEY HANNA 1 The story of the St. Johns River of Florida. A Prince in Their Midst: The Adventurous Life of Achille Murat on the American Frontier (1946) A biography of Prince Murat, nephew of Napoleon. By KATHRYN ABBEY HANNA and A.l.FJ.um JACKSON HANNA LAke Okeechobee, in the American Lakes Series (1948) A history of the large inland area of South Florida encircling Lake Okeechobee. MAPS AND DECORATIONS Florida's Golden Sands (1950) BY DON J. EMERY The Florida East Coast: its unfoldment as a region. THE BOBBS-MERRILL COMPANY, INC. Publishers NEW YORK INDIANAPOLIS f ~ SO I?O Florida's Golden Sands This was true of the Benets of St. Augustine. Pedro Benet, known as King Benet because of his political power, kept a small grocery store and grogshop. To anyone opposing him was always given the warn ing, "take care of Pedro Benet." It was said of him that he bequeathed to his descendants "a fine tradition of integrity, enterprise and achievement." One of his sons, Stephen Vincent, had the distinction of being the first appointee from Florida to West Point. He contin ued in the United States Army after Florida seceded and attained the rank of brigadier general. -
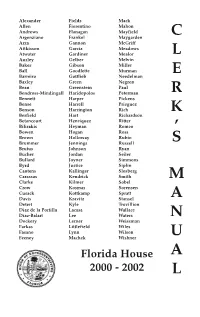
C L E R K ' S M a N U
Alexander Fields Mack Allen Fiorentino Mahon Andrews Flanagan Mayfield Argenziano Frankel Maygarden C Arza Gannon McGriff Attkisson Garcia Meadows Atwater Gardiner Mealor L Ausley Gelber Melvin Baker Gibson Miller Ball Goodlette Murman E Barreiro Gottlieb Needelman Baxley Green Negron Bean Greenstein Paul Bendross-Mindingall Haridopolos Peterman R Bennett Harper Pickens Bense Harrell Prieguez Benson Harrington Rich K Berfield Hart Richardson Betancourt Henriquez Ritter Bilirakis Heyman Romeo Bowen Hogan Ross ’ Brown Holloway Rubio Brummer Jennings Russell S Brutus Johnson Ryan Bucher Jordan Seiler Bullard Joyner Simmons Byrd Justice Siplin Cantens Kallinger Slosberg Carassas Kendrick Smith M Clarke Kilmer Sobel Crow Kosmas Sorensen Cusack Kottkamp Spratt Davis Kravitz Stansel A Detert Kyle Trovillion Diaz de la Portilla Lacasa Wallace Diaz-Balart Lee Waters N Dockery Lerner Weissman Farkas Littlefield Wiles Fasano Lynn Wilson Feeney Machek Wishner U Florida House A 2000 - 2002 L The Clerk's Manual 2000-2002 Compiled for use by The House of Representatives of the State of Florida John B. Phelps, Clerk of the House March 2001 Contents The House of Representatives House Directory....1 Members, by Districts....8 House Districts, by Counties....15 Councils and Committees....17 Members, Biographies....28 Other House Officers....186 Members, Length of Service....189 The Senate Senate Directory....194 Senators, by Districts....197 Senate Districts, by Counties....200 Committees....202 Senators, Biographies....209 Other Senate Officers....282 Senators, Seniority....284 Capitol Press Corps....286 The House of Representatives Tom Feeney, Speaker Sandra L. "Sandy" Murman, Speaker pro tempore Mike Fasano, Majority Leader Lois J. Frankel, Democratic Leader Doug Wiles, Democratic Leader pro tempore John B. -

Volusia County by the Numbers
Hugs are the best medicine. #family #feelingwhole TABLE OF CONTENTS 2019 Executive Committee . 3 2019 Board of Directors . 4 Mission Statement / Vision Statement / Core Values . 5 Important Chamber Events / Programs . 6 Important Numbers . 8 City Profiles Daytona Beach . 10 SERVING MEMBERS SINCE 1919 Daytona Beach Shores / Holly Hill . 11 DAYTONA REGIONAL CHAMBER OF COMMERCE Ormond Beach / Ponce Inlet . 12 126 East Orange Avenue Port Orange / South Daytona . 13 Daytona Beach, FL 32114 386 .255 .0981 • Fax 386 .258 .5104 DeBary / DeLand . 14 DaytonaChamber .com Deltona / Edgewater . 15 CHAMBER PROFESSIONAL TEAM Lake Helen / New Smyrna Beach . .16 Nancy Keefer, CCE Oak Hill / Orange City . 17 President & CEO • 386 .523 .3670 Pierson . 18 Janet Kersey, CDME, CFEE Executive Vice President & COO • 386 .523 .3676 Volusia County Map . 18 Jim Cameron Trustee Member Profiles . 20 Senior VP Government Relations • 386 .523 .3673 Daytona Beach History . 33 Jami Gallegos Membership Director • 386 .523 .3680 Education . 34 Ken Phelps Higher Education . 35 Events Director • 386 .523 .3675 Healthcare . 37 Nichole Sprague Business Manager • 386 .523 .3677 Arts & Culture . 38 Jennifer Pipes Sports . 40 Administrative Assistant & Database Specialist • 386 .523 .3678 Recreation . 41 Cathy Benedict Entertainment / Restaurant / Shopping . 42 Administrative Specialist • 386 .255 .7174 Special Events . 44 Tiffany Moen Receptionist • 386 .255 .0981 Economic Development . 45 Bob Elkin What’s New in 2019 . 46 CFO Consultant • 386 .212 .4515 Chamber Affiliates . 47 CHAMBER AFFILIATES Volusia County by the Numbers . 48 Volusia County Association of Responsible Development (VCARD) Top Employers . 49 Kerry Symolon Karl, Executive Director Buyer’s Guide Category Directory . 50 Volusia Young Professionals Group (VYPG) Vinod Sagrani, Chair Buyer’s Guide Membership Directory . -

Halifax Area Advertising Authority - Executive Update
Halifax Area Advertising Authority - Executive Update December 2019 New Stats . Bed Tax collections (CDT) increased 4.08% , at $460,905 in November 2019, compared to $442,856 in November 2018 . Average Daily Rate increased 5.2% at $110.28 in November 2019, compared to $104.85 in November 2018 . Occupancy remained about the same at 53% in November 2019, compared to 53% in November 2018 Administration . Attended weekly Rotary Club meetings . Visited various accommodations partners . Conducted interviews for the finance/HR position . Met with potential new attraction partners . Participated in a CVB Human Resources Committee meeting . Held a CVB Leadership Team meeting . Discussed CVB office space with Chamber representatives . Participated in the Bike Week Task Force meeting . Participated in STR and AirDNA report training . Met with SE and West Volusia CVBs, and Team Volusia . Met with Adara re: additional marketing opportunities . Attended the Challenge Daytona Triathlon competitors’ meeting and toured the facility . Met with The Shores and joined staff for a CVB reception . Held a conference call with the Welcome to Rockville team . Joined CVB staff in a meeting with Speedway and The Daytona sales staff . Participated in tourism interviews on WSBB-AM and WELE-AM radio . Joined CVB staff for the annual Holiday Potluck gathering . Worked with staff on the Partner Survey and an Employee Satisfaction Survey projects Finance & Human Resources Human Resources . Processed biweekly payrolls . Reviewed payroll and benefits Finance . Continued to review cash flow projections and bank accounts on a daily basis . Performed all accounts payable functions . Updated CDT grid, graphs and factors . Processed financial transactions for October and November 2019 financials . -

1 TOMOKA HISTORICAL TRAIL (From Interstate 95 Exit 278, Drive
TOMOKA HISTORICAL TRAIL (From Interstate 95 Exit 278, drive east, southeast and south on Old Dixie Hwy. to park at the south end of Ormond Tomb Park. Walk northwest 300 feet.) 1 West side of Old Dixie Hwy., between Walter Boardman Ln. and 0.0 Bulow Creek James Ormond Tomb Park Capt. James Ormond of Scotland received a grant for a plantation near here in 1804, which he named Damietta. He was killed by a runaway slave in 1817 and was buried at Nordman's Point. James Ormond II moved here with his wife and four children in 1824. The settlers were on friendly terms and knew Indian chiefs King Philip, Billy Bowlegs, and Coacoochee. Ormond died in 1829 and was buried on the plantation. The family moved to Charleston, South Carolina in 1832. Damietta became the property of Samuel H. Williams, who turned it into his Orange Grove Plantation. Two-thirds of it was sold by the tax collector for his failure to pay state and county taxes for 1849. Inscribed on the grave of James Ormond II is "An Honest Man". The tomb was badly damaged by vandals but was restored and maintained by Maud Van Woy. The nine-acre site was donated to the Park Service in 1945. (Walk northeast to Old Dixie Hwy. and north 700 feet, then east on the park entrance road to the large oak tree.) 2 Bulow Creek State Park, east of Old Dixie Hwy. 0.4 Ormond-Fairchild Oak This tree is said to be over 2,000 years old and is one of the largest in the county. -

03-1 03 1017 Center for Business Excellence Board Membership
03-1 03 1017 Center for Business Excellence board membership appointment. 03-1 03-2 03 1017 Center for Business Excellence board membership appointment. 03-2 03-3 03 1017 Center for Business Excellence board membership appointment. 03-3 03-4 03 1017 Center for Business Excellence board membership appointment. 03-4 03-5 03 1017 Center for Business Excellence board membership appointment. 03-5 03-6 03 1017 Center for Business Excellence board membership appointment. 03-6 03-7 03 1017 Center for Business Excellence board membership appointment. 03-7 03-8 03 1017 Center for Business Excellence board membership appointment. 03-8 03-9 03 1017 Center for Business Excellence board membership appointment. 03-9 03-10 03 1017 Center for Business Excellence board membership appointment. 03-10 03-11 03 1017 Center for Business Excellence board membership appointment. 03-11 03-12 03 1017 Center for Business Excellence board membership appointment. 03-12 03-13 03 1017 Center for Business Excellence board membership appointment. 03-13 03-14 03 1017 Center for Business Excellence board membership appointment. 03-14 03-15 03 1017 Center for Business Excellence board membership appointment. 03-15 03-16 03 1017 Center for Business Excellence board membership appointment. 03-16 03-17 03 1017 Center for Business Excellence board membership appointment. 03-17 03-18 03 1017 Center for Business Excellence board membership appointment. 03-18 03-19 03 1017 Center for Business Excellence board membership appointment. 03-19 03-20 03 1017 Center for Business Excellence board membership appointment. 03-20 03 1017 Center for Business Excellence board membership appointment. -

Tourism Events
MThe missioni ofs thse Hialoifax n Area Advertising Authority and the Daytona Beach Area Convention & Visitors Bureau is to contribute to and enhance the overall economic prosperity of the Halifax Area Taxing District and all of Volusia County through successful promotion of the area as a preferred tourism destination. Contents: Letter from President ....................1 The Budget ....................................5 Meetings & Conventions ........10-14 Travel Industry Sales ..............21-22 Meet Our Boards ..........................2 Consumer Marketing ................6-7 Tourism Events ............................15 Niche Markets ............................23 Tourism By The Numbers ..............3 Fulfillment ......................................8 Communications ....................16-18 Hospitality Services ....................24 Strategic Plan ................................4 Research ......................................9 Technology Services ..............19-20 DBACVB Info ..............................25 Letter From President/CEO The Daytona Beach Area Convention & Visitors Bureau (DBACVB) is pleased to present to you our 2010-11 Destination Marketing Plan. This brand new, easy to use format is designed to provide a complete overview of how we market and sell the Daytona Beach area to vacationers and meeting planners as a favorable destination. This plan is developed each year under the guidance and oversight of the Halifax Area Advertising Authority (HAAA). The majority of the authority’s 11 members represent area lodging facilities. The remainder represent a variety of tourism-related businesses from throughout the Halifax Taxing District. Members must be businesses in good standing and possess a high record of success in the area of tourism marketing application and principals. Appointed by the Volusia County Council, the members oversee the disbursements of the Convention Development Tax through the services of the DBACVB and the implementation of this annual destination marketing plan.