Recent Development of Rapid Antimicrobial Susceptibility Testing Methods Through Metabolic Profiling of Bacteria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Histopathology and Laboratory Features of Sexually Transmitted Diseases
Histopath & Labs for STIs Endo, Energy and Repro 2017-2018 HISTOPATHOLOGY AND LABORATORY FEATURES OF SEXUALLY TRANSMITTED DISEASES Dominck Cavuoti, D.O. Phone: 469-419-3412 Email: [email protected] LEARNING OBJECTIVES: • Identify the etiologic agents causing pelvic inflammatory disease and the pathologic changes they produce. • Discuss the characteristic clinical and pathologic findings caused by herpes simplex virus (HSV) infections: a. fever blisters b. genital herpes simplex virus infection c. disseminated neonatal HSV • Describe the pathologic changes produced by Treponema pallidum. • Describe the clinical features and pathologic changes produced by Chlamydia trachomatisand Neisseria gonorrhoeae • Describe the clinical and laboratory features of vaginal infections including: Trichomonas, Candida, and bacterial vaginosis. • Describe the clinical and laboratory features of ectoparasite infections PURPOSE OF THE LECTURE: 1. To describe the various agents of sexually transmitted diseases and their disease manifestations 2. To describe the pathologic features associated with STDs 3. To introduce some of the laboratory aspects of STDs TERMS INTRODUCED IN LECTURE: Condyloma lata Disseminated gonococcal infection Gummatous syphilis Lymphogranuloma venereum Pelvic inflammatory disease Rapid Plasma Reagin (RPR) Salpingitis Syphilis/endarteritis obliterans Venereal Disease Research Laboratory (VDRL) Treponema pallidum particle agglutination (TPPA) Histopath & Labs for STIs Endo, Energy and Repro 2017-2018 MAJOR CONCEPTS EMPHASIZED IN LECTURE I. Syphilis (Will be covered by Dr. Norgard in later lecture). II. Gonorrhea A. Causative agent: Neisseria gonorrhoeae, a Gram negative diplococcus. Humans are the only natural reservoir. Infection is acquired via direct contact with the mucosa of an infected person. The incubation period averages 2-5 days with a range of 1-14 days. -

Francisella Tularensis 6/06 Tularemia Is a Commonly Acquired Laboratory Colony Morphology Infection; All Work on Suspect F
Francisella tularensis 6/06 Tularemia is a commonly acquired laboratory Colony Morphology infection; all work on suspect F. tularensis cultures .Aerobic, fastidious, requires cysteine for growth should be performed at minimum under BSL2 .Grows poorly on Blood Agar (BA) conditions with BSL3 practices. .Chocolate Agar (CA): tiny, grey-white, opaque A colonies, 1-2 mm ≥48hr B .Cysteine Heart Agar (CHA): greenish-blue colonies, 2-4 mm ≥48h .Colonies are butyrous and smooth Gram Stain .Tiny, 0.2–0.7 μm pleomorphic, poorly stained gram-negative coccobacilli .Mostly single cells Growth on BA (A) 48 h, (B) 72 h Biochemical/Test Reactions .Oxidase: Negative A B .Catalase: Weak positive .Urease: Negative Additional Information .Can be misidentified as: Haemophilus influenzae, Actinobacillus spp. by automated ID systems .Infective Dose: 10 colony forming units Biosafety Level 3 agent (once Francisella tularensis is . Growth on CA (A) 48 h, (B) 72 h suspected, work should only be done in a certified Class II Biosafety Cabinet) .Transmission: Inhalation, insect bite, contact with tissues or bodily fluids of infected animals .Contagious: No Acceptable Specimen Types .Tissue biopsy .Whole blood: 5-10 ml blood in EDTA, and/or Inoculated blood culture bottle Swab of lesion in transport media . Gram stain Sentinel Laboratory Rule-Out of Francisella tularensis Oxidase Little to no growth on BA >48 h Small, grey-white opaque colonies on CA after ≥48 h at 35/37ºC Positive Weak Negative Positive Catalase Tiny, pleomorphic, faintly stained, gram-negative coccobacilli (red, round, and random) Perform all additional work in a certified Class II Positive Biosafety Cabinet Weak Negative Positive *Oxidase: Negative Urease *Catalase: Weak positive *Urease: Negative *Oxidase, Catalase, and Urease: Appearances of test results are not agent-specific. -

Biofire Blood Culture Identification System (BCID) Fact Sheet
BioFire Blood Culture Identification System (BCID) Fact Sheet What is BioFire BioFire BCID is a multiplex polymerase chain reaction (PCR) test designed to BCID? identify 24 different microorganism targets and three antibiotic resistance genes from positive blood culture bottles. What is the purpose The purpose of BCID is to rapidly identify common microorganisms and of BCID? antibiotic resistance genes from positive blood cultures so that antimicrobial therapy can be quickly optimized by the physician and the antibiotic stewardship pharmacist. It is anticipated that this will result in improved patient outcomes, decreased length of stay, improved antibiotic stewardship, and decreased costs. When will BCID be BCID is performed on all initially positive blood cultures after the gram stain is routinely performed and reported. performed? When will BCID not For blood cultures on the same patient that subsequently become positive with be routinely a microorganism showing the same morphology as the initial positive blood performed? culture, BCID will not be performed. BCID will not be performed on positive blood cultures with gram positive bacilli unless Listeria is suspected. BCID will not be performed on blood culture bottles > 8 hours after becoming positive. BCID will not be performed between 10PM-7AM on weekdays and 2PM-7AM on weekends. BCID will not be performed for clinics that have specifically opted out of testing. How soon will BCID After the blood culture becomes positive and the gram stain is performed and results be available? reported, the bottle will be sent to the core Microbiology lab by routine courier. BCID testing will then be performed. It is anticipated that total turnaround time will generally be 2-3 hours after the gram stain is reported. -

Interpreting and Acting on Positive Blood Cultures Trevor Van Schooneveld, MD 1/18/18 Objectives
Stewardship Interventions: Interpreting and Acting on Positive Blood Cultures Trevor Van Schooneveld, MD 1/18/18 Objectives • Interpret the results of blood cultures including gram stains and rapid pathogen diagnostic tests • Make recommendations regarding antimicrobial therapy based on interpretation of blood culture data Early Initiation of Active Therapy is Essential Predicted hospital mortality and 95% CIs for time to first antibiotic administration Surviving Sepsis Guidelines (N=28,150 severe sepsis, septic shock patients) • Administer IV antimicrobials within one hour of presentation (strong) • Initiate empiric, broad-spectrum therapy with one or more agents to cover all likely pathogens (strong) Ferrer R, et al. Crit Care Med. 2014;42:1749-55. Rhodes A, et al. Crit Care Med. 2017;45:486-552. De-escalation Also is Important Surviving Sepsis Guidelines • Narrow empiric antibiotics once pathogen identified and/or clinical improvement De-escalation Benefit • De-escalation in severe sepsis, septic shock (N=712) • Mortality OR 0.54 (95% CI 0.33-0.89, P=.016) • De-escalation in community-onset gram-negative bacteremia (N=189) • Mortality OR 0.37 (0.14-0.96, P=.04) Garnarcho-Montero J, et al. Intensive Care Med. 2014;40:32-40. Lee C, et al. Diag Micro Infect Dis. 2015;82:158-64. Issues with Treatment of Sepsis/Bacteremia Under-treatment • May die (mortality) • May not get better as quickly (LOS, cost) • May develop complications (LOS, cost) Overtreatment • May develop toxicities (cost, LOS) • May develop C. difficile (cost, LOS, readmission) -

BLOOD CULTURE MEDIA Principle: Specimen: Reagent Preparation Storage: Procedure
BLOOD CULTURE MEDIA For In-Vitro and professional use only Store at (2° to 8°C) Blood cultures are used to detect the presence of bacteria or fungi in the blood, to identify the type present, and to guide treatment. Testing is used to identify a blood infection (septicemia) that can lead to sepsis, a serious and life-threatening complication. Individuals with a suspected blood infection are often treated in intensive care units, so testing is often done in a hospital setting. A bacterial infection in the blood called bacteremia. It can be serious because the blood can spread the bacteria to any part of the body. Blood infections most often occur with other serious infections such as those affecting the lungs, kidneys, bowel, gallbladder, or heart valves. Blood infections may also develop when the immune system is weak in infants and older adults, from disease (such as cancer or AIDS) or from medicines (such as corticosteroids or chemotherapy) that change the ability of your body to fight infections (immunity). Principle: The vials containing 25 ml or 50 ml of brain heart infusion, yeast extract, SPS and other stabilizers. The Media is used for yeast, aerobic and anaerobic organisms in blood. The principle of the this test is that each type of organisms need a certain time to grow and multiply. Specimen: Blood. Reagent preparation The vials are ready to use. Storage: Store reagent from (2 - 8 oC). Procedure: 1. Bottles of Brain Heart Infusion which are not used the same day as sterilized should be placed in a boiling water bath for several minutes to remove absorbed oxygen , and cooled rapidly without shaking , just before use. -
Gram Stain Workshop for the Laboratory Generalist
Gram Stain Workshop for the Laboratory Generalist Karen Stiles, SM(ASCP)CM State Training Coordinator Assistant Chemical Terrorism Coordinator Nebraska Public Health Laboratory 402-559-3590 [email protected] 1 GRAM STAIN OBJECTIVES: Upon completion, the participant will be able to: 1. Explain the principle of the Gram stain procedure, including what elements can affect staining results 2. Correlate the most common pathogens with positive Gram stains from blood cultures and direct specimen sterile body fluid smears 3. Perform and interpret Grams stains 2 Purpose of Gram Stain Classify bacteria based on form, size, cellular morphology, Gram reaction Assess quality of specimen Identify specific infectious agent from morphology and Gram reaction Correlation with culture growth Correlation with culture-independent methodologist Guide presumptive antibiotic therapy 3 Principle of Gram Stain Cell wall composition Gram positive – think peptidoglycan layer with teichoic acid Gram negative – high in lipid content Basic premise Crystal Violet – all cells take up primary stain Gram’s iodine – mordant to form complex Decolorizer – mixture of acetone and alcohol Dehydrate lipids in Gram negative cell walls, wash out complex Gram positive cells resistant, retain stain complex Safranin - counterstain 4 Gram negative cells take up counterstain Preparation of Samples Specimen Type Preparation CSF/sterile body fluids Cyto/Centrifuge Blood Culture Broth Drop to slide Tissue Touch prep Tissue homogenate Drop to slide Swabbed material Roll -

Blood Culture Sampling Policy for Adult and Paediatric Patients
Blood Culture Sampling Policy for Adult and Version: 7.0 Paediatric Patients Date Issued: 25 July 2018 Review Date: 30 May 2021 Document Type: Policy Contents Page Paragraph Executive Summary / Policy Statement / Flowchart 2 1 Scope and Purpose 2 2 Definitions 2 3 Indications for taking a blood culture and procedure 4 4 Roles and Responsibilities 7 5 Related Trust Policies 8 6 Implementation (including training and dissemination) 8 7 Process for Monitoring Compliance/Effectiveness of 9 this Policy 8 Arrangements for Review of this Policy 9 9 References 9 Appendices Page Appendix A List of equipment needed for peripheral blood culture 10 sampling Appendix B ANTT clinical guideline for Blood Culture Sampling 10 Appendix C ANTT clinical guideline for Blood Culture Sampling 10 from a CVC Device without a Transducer Appendix D ANTT clinical guideline for Blood Culture Sampling 10 from a CVC Device with a Transducer Appendix E Paediatric ANTT guideline for Blood Culture Sampling 10 from a CVC device Document Status This is a controlled document. Whilst this document may be printed, the electronic version posted on the intranet is the controlled copy. Any printed copies of this document are not controlled. As a controlled document, this document should not be saved onto local or network drives but should always be accessed from the intranet. Page 1 of 11 Executive Summary Blood cultures are used to detect the cause of a bloodstream infection. The result provides a guide to the appropriate treatment of the patient. False positives may occur if micro- organisms from a site outside of the bloodstream are introduced into the sample of blood obtained for culture which can then result in inappropriate antibiotic therapy and a waste of healthcare resources. -

Blood Culture
CHI Health Laboratory 4955 F Street Omaha, NE 68117 Phone: 402-717-5227 Fax: 402-717-5252 BLOOD CULTURE Determine the type of culture bottles to utilize, as indicated per physician's order. If necessary, discuss timing of cultures, sites, need for any special instructions with the physician. Alegent Creighton Laboratory Blood Culture tube guide Optimal Age Group Bottle Distribution Difficult draw Volume Infant (Neonate -1 Bactec® Peds Plus 1-3 ml All into Peds bottle N/A yr old Child (1-5 yrs) Bactec® Peds Plus 1-5 ml All into Peds bottle N/A Bactec® Aerobic 8 ml into Aerobic bottle, the Child (6-8 yrs), < 8 ml, entire specimen and Anaerobic 10 ml remaining into the under 80 lbs in Aerobic Bottle bottles Anaerobic bottle 8 ml into Aerobic Adults > 8 yrs old Bactec® Aerobic bottle, the remaining 10 ml Aerobic bottle and children > 80 and Anaerobic 20 ml into Anaerobic bottle 10 ml Anaerobic bottle lbs bottles <8 ml entire specimen into Aerobic bottle Bactec® Myco/F All ages 3-5 ml All into Fungal bottle 3 ml minimum bottle BLOOD CULTURE BOTTLE STORAGE REQUIREMENTS: The Bactec blood culture bottles are ready for use as received and require no reconstitution or dilution. Store vials upright, in a cool, dry place (2-25°C), out of direct light. SPECIMEN COLLECTION: 1. Types of Blood Cultures available a. Routine blood culture b. Fungus blood culture c. Acid Fast blood culture d. CMV blood culture 2. Number and Timing - Most cases of bacteremia are detected by using 2 sets of blood cultures, collected separately. -

(BCID) Results Are “Not Detected”
Interpretation of Positive Blood Cultures When PCR Blood Culture Identification (BCID) Results are “Not Detected” Nebraska Medicine currently uses a multi-plex PCR-based blood culture identification (BCID) system that is able to identify 19 potential pathogens growing in blood culture. BCID generally detects over 90% of the most common causative agents in bloodstream infections; however, when microbes not included on the panel are present in a blood culture, it returns a result of “Not Detected.” This document aims to provide guidance in these scenarios supported by data collected at Nebraska Medicine from January 2018 to August 2019. Table 1: Recommendations for treatment of patients with blood cultures growing organisms not detected on BCID Gram Stain/Preliminary Likely Organism (% total BCID negative)* Recommended Treatment Culture Result Gram-positive: Aerobe Micrococcus sp. (18.1%) (most can also grow in Coagulase-negative Staphylococcus (9.3%) None anaerobic bottles) Diphtheroids (7%) None Peptostreptococcus sp. (4.4%) If therapy is desired: Anaerobe bottle only Lactobacillus sp. (2.6%) Metronidazole 500 mg PO q8h Clostridium sp. (2.6%) OR Penicillin G 4 million units IV q4h Gram-negative: Aerobe Acinetobacter sp. (1.8%) (most can also grow in Stenotrophomonas maltophilia (1.6%) Levofloxacin 750 mg IV/PO q24h anaerobic bottles) Pseudomonas fluorescens-putida group (1%) Bacteroides fragilis group (9.3%) Anaerobe bottle only Metronidazole 500 mg IV/PO q8h Fusobacterium sp. (4.7%) *A full list of isolated organisms can be found below in Table 2 Orange text = Cocci, Blue text = Bacilli (rods) Gram-Positives When BCID results as “Not Detected” but there is microbial growth, the organism is most frequently gram-positive (71%). -
ANTT Guidelines
www.antt .org ANTT Guidelines The ANTT Clinical Guideline for Blood Culture Collection Rationale and supporting evidence 1 ANTT: Blood Culture Collection v2.0 2013 The Association for Safe Aseptic Practice www.antt.org © 2013 Aseptic Non Touch Technique (ANTT)® This document is a publication of The-ASAP and all rights of copyright, intellectual property and Trademark are reserved. ANTT is protected to prevent dilution and misrepresentation of the practice framework so as to avoid ANTT becoming another unhelpful generic term for aseptic technique that is variably interpreted. For guidance see [email protected]. This document may however, be freely reviewed, copied and translated, in part, or in whole, for LOCAL, SINGLE ORGANIZATION educational use. It must not be published via the www/internet or its content used for production and publication of dedicated ANTT e-learning resources. ANTT is not for sale or for use in conjunction with commercial purposes. The-ASAP provide a number of free core ANTT resources to help disseminate and train healthcare staff. The- ASAP requests that the balance it determines between free dissemination and protection of the standard is respected in the interests of patient safety. Disclaimer: The-ASAP provides the ANTT Clinical Practice Framework and ANTT Clinical Guidelines to healthcare organizations in good faith in a collaboration to promote effective aseptic technique. It is the responsibility of healthcare organizations to implement ANTT effectively. No guarantee or responsibility for the application or outcome of clinical practice can be, or is, assumed or accepted by The-ASAP/ANTT. Published by The Association for Safe Aseptic Practice (ASAP) ANTT: Blood Culture Collection v2.0 2013 The Association for Safe Aseptic Practice www.antt.org 2 Glossary Please note: Historically, the terms below have been defined variously and often ambiguously in the medical literature. -

A Complicated Course of Acute Viral Induced Pharyngitis, Icteric Hepatitis, Acalculous Cholecystitis, and Skin Rash
Hindawi Publishing Corporation Case Reports in Medicine Volume 2016, Article ID 6796094, 5 pages http://dx.doi.org/10.1155/2016/6796094 Case Report A Complicated Course of Acute Viral Induced Pharyngitis, Icteric Hepatitis, Acalculous Cholecystitis, and Skin Rash Fereshte Sheybani,1 HamidReza Naderi,1 Seddigheh Sadat Erfani,1 and Masoumeh Gharib2 1 Department of Infectious Diseases, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran 2Department of Pathology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran Correspondence should be addressed to Masoumeh Gharib; [email protected] Received 17 July 2016; Revised 17 September 2016; Accepted 5 October 2016 Academic Editor: Walter Zidek Copyright © 2016 Fereshte Sheybani et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. This case reveals the complexities and challenges in the diagnosis of acute Epstein-Barr virus (EBV) infection, indicating the potential relationship between EBV infection and severe icteric hepatitis, acalculous cholecystitis, and lymphocytic vasculitis. We suggest including EBV infectious mononucleosis in the list of differential diagnoses when any of these clinical syndromes (ora combination thereof) occurs without apparent cause, especially in the presence of lymphocytosis. To our knowledge, this is the first report to suggest the possible role of EBV in the pathogenesis of cutaneous lymphocytic vasculitis. Also it is possible that EBV infection triggered the flare-up of the underlying rheumatologic disease. Therefore, it could be assumed that a part of the clinical syndrome (e.g., dermatologic manifestations) might be related to the flare-up of the underlying rheumatologic disease. -
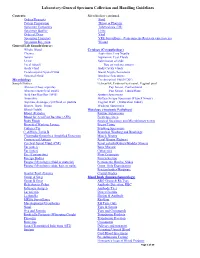
Laboratory-General Specimen Collection and Handling Guidelines
Laboratory-General Specimen Collection and Handling Guidelines Contents: Microbiology continued. Orders/Requests Stool Patient Preparation Throat or Pharynx Specimen Containers Tuberculosis (TB) Specimen Quality Urine Order of Draw Viral Specimen Transport VRE Surveillance (Vancomycin- Resistant entercoccus) Specimen Rejection Wound General Lab Sample/Source: Whole Blood Cytology (Cytopathology) Plasma Aspiration, Fine Needle Serum Aspiration, Cyst Fluids Urine Submission of slide Fecal (Stool) Tips on making smears Body Fluid Body Cavity Fluids Cerebrospinal Spinal Fluid Breast Nipple Secretions Synovial Fluid Brushing Specimens Microbiology Cerebrospinal Fluid (CSF) Sample/Source: Ectocervix, Endocervical canal, Vaginal pool Abscess (Deep aspirate) Pap Smear, Conventional Abscess (superficial swab) Pap Smear, Liquid Base Acid Fast Bacillus (AFB) Sputum Specimens Anaerobic Surface Scrape Specimen (Tzanck Smear) Aspirate, drainage, cyst fluid, or pustule Vaginal Wall (Maturation Index) Biopsy, Bone, Tissue Washing Specimens Blood (Adult) Histology (Anatomic Pathology) Blood )Pediatric Routine Submission Blood for Acid Fast Bacillus (AFB) Fresh Specimen Body Fluids Surgical Specimen and Microbiology test(s) Bronchial Washing Lavage Breast Tissue Catheter Tip Brushing Specimens C. difficile Toxin B Bronchial Washing and Brushings Chlamydia/Gonorrhea Amplified Detection Muscle Biopsy Crytococcal Antigen Renal Biopsy (Kidney) Cerebral Spinal Fluid (CSF) Renal calculi (Kidney/Bladder Stones) Ear (outer) Bone Marrow Ear (inner) Cytogenics Eye