Studies of New Sympathomimetic Beta-Receptor Stimulating Drugs in Asthmatic Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MDPV Bath Salts Test
One Step Methylenedioxypyrovalerone Drug of Abuse Test MATERIALS Analytical Sensitivity The cut-off concentration of the One Step Methylenedioxypyrovalerone Drug of Abuse Test is determined to be 1,000ng/mL. (Dip Card) Materials Provided: Test was run in 30 replicates with negative urine and standard control at ±25% cut-off and ±50% cut-off concentration levels. Test results ● Dip cards are summarized below. For Forensic Use Only ● Desiccants ● Package insert Test Result INTENDED USE Percent of Cut-off n Materials Required But Not Provided: Methylenedioxypyrovalerone Concentration in ng/mL The One Step Methylenedioxypyrovalerone Drug of Abuse Test is a lateral flow chromatographic immunoassay for the ● Specimen collection container Negative Positive qualitative detection of Methylenedioxypyrovalerone (MDPV) in human urine specimen at the cut-off level of 1,000ng/mL. This ● Disposable gloves 0% Cut-off assay is intended for forensic use only. ● Timer 30 30 0 This assay provides only a preliminary qualitative test result. A more specific confirmatory reference method, such as Liquid (No Drug Present) chromatogra -50% Cut-off phy tandem mass spectrometry (LC/MS/MS) or gas chromatography/mass spectrometry (GC/MS) must be use in INSTRUCTIONS FOR USE] 30 30 0 order to obtain a confirmed analytical result. (500ng/mL) 1) Remove the dip card from the foil pouch. -25% Cut-off 30 30 0 BACKGROUND 2) Remove the cap from the dip card. Label the device with patient or control identifications. (750ng/mL) 3) Immerse the absorbent tip into the urine sample for 5 seconds. Urine sample should not touch the plastic device. Cut-off ‘Bath salts’, a form of designer drugs, also promoted as ‘plant food’ or ‘research chemicals’, is sold mainly in head shops, on 4) Replace the cap over the absorbent tip and lay the dip card on a clean, flat, and non-absorptive surface. -

PRODUCT MONOGRAPH ORCIPRENALINE Orciprenaline Sulphate Syrup House Standard 2 Mg/Ml Β2-Adrenergic Stimulant Bronchodilator AA P
PRODUCT MONOGRAPH ORCIPRENALINE Orciprenaline Sulphate Syrup House Standard 2 mg/mL 2-Adrenergic Stimulant Bronchodilator AA PHARMA INC. DATE OF PREPARATION: 1165 Creditstone Road, Unit #1 April 10, 2014 Vaughan, Ontario L4K 4N7 Control Number: 172362 1 PRODUCT MONOGRAPH ORCIPRENALINE Orciprenaline Sulfate Syrup House Standard 2 mg/mL THERAPEUTIC CLASSIFICATION 2–Adrenergic Stimulant Bronchodilator ACTIONS AND CLINICAL PHARMACOLOGY Orciprenaline sulphate is a bronchodilating agent. The bronchospasm associated with various pulmonary diseases - chronic bronchitis, pulmonary emphysema, bronchial asthma, silicosis, tuberculosis, sarcoidosis and carcinoma of the lung, has been successfully reversed by therapy with orciprenaline sulphate. Orciprenaline sulphate has the following major characteristics: 1) Pharmacologically, the action of orciprenaline sulphate is one of beta stimulation. Receptor sites in the bronchi and bronchioles are more sensitive to the drug than those in the heart and blood vessels, so that the ratio of bronchodilating to cardiovascular effects is favourable. Consequently, it is usually possible clinically to produce good bronchodilation at dosage levels which are unlikely to cause cardiovascular side effects. 2 2) The efficacy of the bronchodilator after both oral and inhalation administration has been demonstrated by pulmonary function studies (spirometry, and by measurement of airways resistance by body plethysmography). 3) Rapid onset of action follows administration of orciprenaline sulphate inhalants, and the effect is usually noted immediately. Following oral administration, the effect is usually noted within 30 minutes. 4) The peak effect of bronchodilator activity following orciprenaline sulphate generally occurs within 60 to 90 minutes, and this activity lasts for 3 to 6 hours. 5) Orciprenaline sulphate taken orally potentiates the action of a bronchodilator inhalant administered 90 minutes later, whereas no additive effect occurs when the drugs are given in reverse order. -
Temporary Class Drug Order Report: 5-6APB and Nbome Compounds
ACMD Advisory Council on the Misuse of Drugs Chair: Professor Les Iversen Secretary: Rachel Fowler 3rd Floor (SW), Seacole Building 2 Marsham Street London SW1P 4DF Tel: 020 7035 0555 [email protected] Home Secretary Rt Hon. Theresa May MP Home Office 2 Marsham Street London SW1P 4DF 29 May 2013 Dear Home Secretary, I am writing to formally request that you consider laying a temporary class drug order (TCDO) pursuant to section 2A of the Misuse of Drugs Act 1971 on the following two groups of novel psychoactive substances (NPS). We consider the laying of TCDOs is appropriate as a pre-emptive measure in advance of the summer music festival season. Both classes of drugs have been associated with serious harm and drug-related deaths. ‘Benzofury’ compounds 5- and 6-APB and related substances are phenethylamine-type materials, related to ecstasy (MDMA). There have been several deaths and hospitalisations in the UK associated with these NPS, although poly-substance use often complicates the case. Research indicates that there is a potential risk of cardiac toxicity associated with the long-term use of 5- and 6-APB. Anecdotal user reports suggest that the consumption of these substances can cause insomnia, increased heart rate and anxiety, with some users reporting MDMA like symptoms. The related compound 5-IT has been subject to an EMCDDA-Europol joint report and an EMCDDA risk assessment exercise. [www.emcdda.europa.eu/publications/joint-reports/5- IT] 1 The substances recommended for control are: 5- and 6-APB: (1-(benzofuran-5-yl)-propan-2-amine and 1-(benzofuran-6-yl)-propan- 2-amine) and their N-methyl derivatives. -

The Place of Physical Exercise and Bronchodilator Drugs in the Assessment of the Asthmatic Child
Arch Dis Child: first published as 10.1136/adc.38.202.539 on 1 December 1963. Downloaded from Arch. Dis. Childh., 1963, 38, 539. THE PLACE OF PHYSICAL EXERCISE AND BRONCHODILATOR DRUGS IN THE ASSESSMENT OF THE ASTHMATIC CHILD BY R. S. JONES, M. J. WHARTON and M. H. BUSTON From Alder Hey Children's Hospital and the Department of Child Health, University ofLiverpool (RECEIVED FOR PUBLICATION MAY 9, 1963) Among the many factors that affect ventilatory exercise. Isoprenaline sulphate I % (Burroughs Wellcome function in the asthmatic subject, physical exercise preparation) was given as an aerosol using a Wright and bronchodilator drugs are two of the more inhaler and an air flow rate of 8-9 litres per minute important. It has been shown that physical exercise (Wright, 1958). The aerosol was fed into a face mask has two distinct and opposite effects on ventilatory held close to the face. The substance was inhaled for one minute and for two subsequent half-minute periods function depending upon the duration and level of during a total time of five minutes. Solutions of exercise (Jones, Buston and Wharton, 1962). adrenaline and noradrenaline were made up from the Providing the level is adequate, exercise lasting less solid substances (Burroughs Wellcome preparations) in than two minutes increases the forced expiratory strengths of 1% with added sodium metabisulphite. volume in one second (F.E.V.), whereas exercise These preparations were used fresh and were inhaled by copyright. lasting eight to 10 minutes produces a fall of F.E.V. in the same way as isoprenaline. -

Regulations 2021
STATUTORY INSTRUMENTS. S.I. No. 121 of 2021 ________________ MISUSE OF DRUGS (AMENDMENT) REGULATIONS 2021 2 [121] S.I. No. 121 of 2021 MISUSE OF DRUGS (AMENDMENT) REGULATIONS 2021 I, STEPHEN DONNELLY, Minister for Health, in exercise of the powers conferred on me by sections 4, 5 (amended by section 3 of the Misuse of Drugs (Amendment) Act 2016 (No. 9 of 2016)), 18 and 38 of the Misuse of Drugs Act 1977 (No. 12 of 1977) and section 5 of the Misuse of Drugs Act 1984 (No. 18 of 1984), hereby make the following regulations: 1. These Regulations may be cited as the Misuse of Drugs (Amendment) Regulations 2021. 2. The Misuse of Drugs Regulations 2017 (S.I. No. 173 of 2017) are amended by the substitution of the following Schedule for Schedule 1: Notice of the making of this Statutory Instrument was published in “Iris Oifigiúil” of 23rd March, 2021. [121] 3 “Schedule 1 1. The following substance and products, namely- (a) N-(Adamantan-1-yl)-1-(5-fluoropentyl)-1H-indazole-3-carboxamide (otherwise known as Clockwork Orange, 5F AKB48) N-[(2S)-1-Amino-3,3-dimethyl-1-oxobutan-2yl]-1-(cyclohexylmethyl)-1H- indazole-3-carboxamide (otherwise known as ADB-CHMINACA) N-(1-Amino-3,3-dimethyl-1-oxobutan-2yl)-1-(4-fluorobenzyl)-1H-indazole- 3-carboxamide (otherwise known as ADB-FUBINACA) N-[(2S)-1-Amino-3-methyl-1-oxobutan-2-yl]-1-(cyclohexylmethyl)-1H- indazole-3-carboxamide (otherwise known as AB-CHMINACA) N-[(2S)-1-Amino-3-methyl-1-oxobutan-2yl]-1-pentyl-1H-indazole-3- carboxamide (otherwise known as AB-PINACA) 5-(2-Aminopropyl)indole (otherwise known -
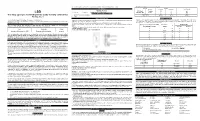
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

Thermogenic Drugs for the Treatment of Obesity: Sympathetic Stimulants in Animal Models
Downloaded from https://doi.org/10.1079/BJN19840087 British Journal of Nutrition (1984), 52, 179-196 179 https://www.cambridge.org/core Thermogenic drugs for the treatment of obesity: sympathetic stimulants in animal models BY A. G. DULL00 AND D. S. MILLER* Department of Nutrition, Queen Elizabeth College, University of London, Campden Hill Road, London W8 7AH . IP address: (Received 5 September 1983 - Accepted 3 March 1984) 1. Thirty-three drugs known to stimulate the sympathetic nervous system have been screened for thermogenic 170.106.40.219 properties. The results presented are for seven of them. 2. The drugs were tested in five animal models of obesity (genetic (mice and rats), hypothalamic (mice) and dietary (mice and rats)) as well asin leanmice. Energy-balance studies wereundertaken using thecomparative-carcass technique as well as by measurement of daily oxygen consumption. 3. All seven drugs in obese animals tended to reduce body-weight and fat without loss of body protein: they , on acted by increasing metabolic rate without increasing food intake. They were much less effective in lean animals. 28 Sep 2021 at 20:28:29 These findings lend support to the concept that obesity is due to a diminished activity of the sympathetic nervous system. 4. Differences in the effectiveness of the drugs are discussed in relation to differences between the animal models of obesity. Ephedrine and tranylcypromine were found to be the most effective drugs in this series of experiments and a prima facie case is made for human clinical trials. The methodology for screening thermogenic drugs for the treatment of obesity has been , subject to the Cambridge Core terms of use, available at outlined by Massoudi et al. -

One Step Multi-Drug Screen Test Cup Package Insert
Fentanyl (FEN) Fentanyl 300 the treatment of seizure disorders and alcohol withdrawal. Risk of physical dependence increases if One Step Multi-Drug Screen Test Cup Benzodiazepines are taken regularly (e.g., daily) for more than a few months, especially at higher Fentanyl (FEN) Fentanyl 200 than normal doses. Stopping abruptly can bring on such symptoms as trouble sleeping, Package Insert Fentanyl (FEN) Fentanyl 100 gastrointestinal upset, feeling unwell, loss of appetite, sweating, trembling, weakness, anxiety and changes in perception. Only trace amounts (less than 1%) of most Benzodiazepines are excreted Cotinine (COT) Cotinine 200 Package insert for testing of any combination of the following drugs: Methamphetamine, unaltered in the urine; most of the concentration in urine is conjugated drug. The detection period Amphetamine, Cocaine, Morphine, Ecstasy, EDDP (Methadone Metabolites), Tricyclic 6-Monoacetylmorphine (6-MAM) 6-Monoacetylmorphine 10 for the Benzodiazepines in the urine is 3-7 days. Antidepressants, Oxycodone, Barbiturates, Buprenorphine, Phencyclidine, K2 (Synthetic Methaqualone (MQL) Methaqualone 300 Cannabinoid), Ketamine, Methaqualone, Methadone, Fentanyl, Tramadol, Ethyl Glucuronide, OXYCODONE (OXY) Cotinine, 6-Monoacetylmorphine, Methylenedioxypyrovalerone, Lysergic acid diethylamide, Ketamine (KET) Ketamine 1,000 Oxycodone, [4,5-epoxy-14-hydroxy-3-methoxy-17-methyl-morphinan-6-one, Marijuana and Benzodiazepines. Ketamine (KET) Ketamine 100 dihydrohydroxycodeinone] is a semi-synthetic opioid agonist derived from thebaine, -

ORAL SYMPATHOMIMETIC AMINES in TREATMENT of ASTHMA *Indirect M.B.C.=F.E.V.0.7, X
14, 1963 INFECTION DUE TO MYCOBACTERIUM AVIUM BLUTisH 1506 DEC. ~~~~~~~~~~~~~~~~~~~~MEDICALJOURNAL We are indebted to many physicians for access to clinical Furniss, A. L., Collins, C. H., and Marks, J. (1961). Mth. Bull. in to Dr. R. G. Prosser Evans and Dr. Minist. Hlth Lab. Serv., 20, 126. histories and particular Griffith, A. S. (1938). Proc. roy. Soc. Med., 31, 1208. G. T. Morris for help with Case 1. Professor J. Gough. Dr. Griffith, A. H., Marks, J., and Richards, M. (1963). Tubercle R. M. E. Seal, and Dr. C. W. Jobling kindly provided patho- (Lond.), 44, 135. logical reports and Mr. C. Lediard gave us considerable Hart, P. D'Arcy, Miller, C. L., Sutherland, I., and Lesslie, 1. W. (1962). Ibid., 43. 268. technical assistance. Karlson, A. G., Andersen, H. A., and Needham, G. M. (1955). Dis. REFERENCES Chest, 28, 451. Bradbury, F. C. S., and Young, J. A. (1946). Lancet, 1, 89. Marks, J., and Richards, M. (1962). Mth. Bull. Minist. Hith Lab. Feldman, W. H (1938). Avian Tuberculosis Infections. Bailliere, Serv., 21, 200. Tindall and Cox, London. Nassal, J. (1961). Dtsch. med. Wschr., 86, 1855. Flynn, M. P. (1962). Tubercle (Lond.), 43, 64. Runyon, E. H. (1959). Med. Clin. N. Amer., 43, 273. ORAL SYMPATHOMIMETIC AMINES IN TREATMENT OF ASTHMA BY M. C. S. KENNEDY, B.A., M.R.C.S., L.R.C.P. S. L. 0. JACKSON, M.D., M.R.C.P. Department of Respiratory Physiology, City General Hospital, Stoke-on-Trent Since the work of Barger and Dale (1910) adrenaline has inhalation, and by subcutaneous injection have been been one of the most effective remedies in certain forms confirmed (Kennedy, 1963). -

A Pharmacological. Study of the Ephedrine Isomers
This dissertation has been 64—1295 microfilmed exactly as received PATIL, Popat Narayan, 1934- A PHARMACOLOGICAL. STUDY OF THE EPHEDRINE ISOMERS. The Ohio State Universityt Ph,Dt, 1963 Pharmacology University Microfilms, Inc., Ann Arbor, Michigan A PHARMACOLOGICAL STUDY OF THE HPHEDRIHE ISOMERS DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Popat Narayan Patil, B. Sc. in Phara., M. Sc. xxxxx The Ohio S tate University 1963 Approved by Adi College of Pharmacy ACKNOWLEDGMENTS The author would Ilka to acknowledge the efforte of Drs. Arthur Tye and Jules B. LaPidus for their valuable advice and Inspiration. The suggestions of Drs* Harold H. Wolf and John W. Nelson are also acknowledged. Special thanks to Mr* Balkrishna Modi for preparing the isomers and Mr. Dalai for the statistical analysis of the data* ii TABLE OF CONTENTS ACKNOWLEDGMENTS .................................................................................. LIST OF TABLES.................................................................................. LIST OF ILLUSTRATIONS ...................................................................... LIST OF ABBREVIATIONS ...................................................................... CHAPTER I. INTRODUCTION AND LITEiiATURS REVIEW G e n e r a l ......................................... .................................... Literature on Optical Isom ers ................................. II. MATERIALS AND METHODS Acute -

Para-Methoxymethylamphetamine (PMMA) Critical Review Report Agenda Item 5.6
para-Methoxymethylamphetamine (PMMA) Critical Review Report Agenda item 5.6 Expert Committee on Drug Dependence Thirty-seventh Meeting Geneva, 16-20 November 2015 37th ECDD (2015) Agenda item 5.6 PMMA Page 2 of 27 37th ECDD (2015) Agenda item 5.6 PMMA Contents Acknowledgements .......................................................................................................................... 5 Summary .......................................................................................................................................... 6 1. Substance identification ................................................................................................................ 7 A. International Nonproprietary Name (INN) .................................................................................... 7 B. Chemical Abstract Service (CAS) Registry Number ...................................................................... 7 C. Other Names .................................................................................................................................. 7 D. Trade Names .................................................................................................................................. 7 E. Street Names .................................................................................................................................. 7 F. Physical properties ........................................................................................................................ 7 G. WHO Review History