Runx Expression in Normal and Osteoarthritic Cartilage: Possible Functions of Runx Proteins in Chondrocytes: a Dissertation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human TNNI1 Antibody Catalog Number: ATGA0558
Human TNNI1 antibody Catalog Number: ATGA0558 PRODUCT INPORMATION Catalog number ATGA0558 Clone No. AT36E7 Product type Monoclonal antibody UnitProt No. P19237 NCBI Accession No. NP_003272 Alternative Names Troponin I slow skeletal muscle, Troponin I, slow skeletal muscle, DKFZp451O223, SSTNI, TNN1 Additional Information This product was produced from tissue culture supe PRODUCT SPECIFICATION Antibody Host Mouse Reacts With Human Concentration 1mg/ml (determined by BCA assay) Formulation Liquid in. Phosphate-Buffered Saline (pH 7.4) with 0.02% Sodium Azide, 10% glycerol Immunogen Recombinant human TNNI1 (1-187aa) purified from E. coli Isotype IgG2b kappa Purification Note By protein-A affinity chromatography Application ELISA,WB Usage The antibody has been tested by ELISA and Western blot analysis to assure specificity and reactivity. Since application varies, however, each investigation should be titrated by the reagent to obtain optimal results. 1 Human TNNI1 antibody Catalog Number: ATGA0558 Storage Can be stored at +2C to +8C for 1 week. For long term storage, aliquot and store at -20C to -80C. Avoid repeated freezing and thawing cycles. BACKGROUND Description Troponin I, slow skeletal muscle, also known as TNNI1, belongs to the troponin I family. The troponin I subfamily contains three genes: TNNI-skeletal-fast-twitch, TNNI-skeletal-slow-twitch, and TNNI-cardiac. The TNNI-fast and TNNI-slow genes are expressed in fast-twitch and slow-twitch skeletal muscle fibers, respectively, while the TNNI- cardiac gene is expressed exclusively in cardiac muscle tissue. TNNI1 is the inhibitory subunit; blocking actin- myosin interactions and thereby mediating striated muscle relaxation. General References Hunkeler NM, Kullman J, Murphy AM (1991). -

Identification of the Binding Partners for Hspb2 and Cryab Reveals
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2013-12-12 Identification of the Binding arP tners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non- Redundant Roles for Small Heat Shock Proteins Kelsey Murphey Langston Brigham Young University - Provo Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Microbiology Commons BYU ScholarsArchive Citation Langston, Kelsey Murphey, "Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins" (2013). Theses and Dissertations. 3822. https://scholarsarchive.byu.edu/etd/3822 This Thesis is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston A thesis submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Master of Science Julianne H. Grose, Chair William R. McCleary Brian Poole Department of Microbiology and Molecular Biology Brigham Young University December 2013 Copyright © 2013 Kelsey Langston All Rights Reserved ABSTRACT Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactors and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston Department of Microbiology and Molecular Biology, BYU Master of Science Small Heat Shock Proteins (sHSP) are molecular chaperones that play protective roles in cell survival and have been shown to possess chaperone activity. -

Supplementary Table 3 Complete List of RNA-Sequencing Analysis of Gene Expression Changed by ≥ Tenfold Between Xenograft and Cells Cultured in 10%O2
Supplementary Table 3 Complete list of RNA-Sequencing analysis of gene expression changed by ≥ tenfold between xenograft and cells cultured in 10%O2 Expr Log2 Ratio Symbol Entrez Gene Name (culture/xenograft) -7.182 PGM5 phosphoglucomutase 5 -6.883 GPBAR1 G protein-coupled bile acid receptor 1 -6.683 CPVL carboxypeptidase, vitellogenic like -6.398 MTMR9LP myotubularin related protein 9-like, pseudogene -6.131 SCN7A sodium voltage-gated channel alpha subunit 7 -6.115 POPDC2 popeye domain containing 2 -6.014 LGI1 leucine rich glioma inactivated 1 -5.86 SCN1A sodium voltage-gated channel alpha subunit 1 -5.713 C6 complement C6 -5.365 ANGPTL1 angiopoietin like 1 -5.327 TNN tenascin N -5.228 DHRS2 dehydrogenase/reductase 2 leucine rich repeat and fibronectin type III domain -5.115 LRFN2 containing 2 -5.076 FOXO6 forkhead box O6 -5.035 ETNPPL ethanolamine-phosphate phospho-lyase -4.993 MYO15A myosin XVA -4.972 IGF1 insulin like growth factor 1 -4.956 DLG2 discs large MAGUK scaffold protein 2 -4.86 SCML4 sex comb on midleg like 4 (Drosophila) Src homology 2 domain containing transforming -4.816 SHD protein D -4.764 PLP1 proteolipid protein 1 -4.764 TSPAN32 tetraspanin 32 -4.713 N4BP3 NEDD4 binding protein 3 -4.705 MYOC myocilin -4.646 CLEC3B C-type lectin domain family 3 member B -4.646 C7 complement C7 -4.62 TGM2 transglutaminase 2 -4.562 COL9A1 collagen type IX alpha 1 chain -4.55 SOSTDC1 sclerostin domain containing 1 -4.55 OGN osteoglycin -4.505 DAPL1 death associated protein like 1 -4.491 C10orf105 chromosome 10 open reading frame 105 -4.491 -

Supplementary Material Figures
1 Supplementary Material 2 3 Figures: 4 Suppl. Figure 1: Network analysis organs without serum. 5 In a GeneMANIA® network analysis each circle represents a gene. The input proteins/genes are 6 depicted as striped circles of the same size, while the monochromatic circles, whose size is proportional 7 to the number of interactions according to the software, can be considered as “relevant” related genes 8 found by GeneMANIA® searching in many large, publicly available biological datasets (including protein- 9 protein, protein-DNA and genetic interactions, pathways, reactions, gene and protein expression data, 10 protein domains and phenotypic screening profiles). Lines linking different circles can be distinguished 11 from their colour, mainly: violent represents co-expression (when expression levels are similar across 12 conditions in a gene expression study); light orange represents predicted functional relationships 13 between genes; light blue represents co-localization (when genes are expressed in the same tissue, or 14 proteins found in the same location); light yellow represents shared protein domains (when two gene 15 products have the same protein domain). 1 1 Tables: 2 Suppl. Table 1: Fifty-one functions filtered by absolute number (cut-off ≥7) from the original 159 deriving 3 from GeneMania® network analysis of the whole dataset without the serum proteins. Column 1 shows 4 the functions names. Columns 2 and 3 show respectively the number of annotated genes in the 5 displayed network and the number of genes with that annotation -

Troponin Variants in Congenital Myopathies: How They Affect Skeletal Muscle Mechanics
International Journal of Molecular Sciences Review Troponin Variants in Congenital Myopathies: How They Affect Skeletal Muscle Mechanics Martijn van de Locht , Tamara C. Borsboom, Josine M. Winter and Coen A. C. Ottenheijm * Department of Physiology, Amsterdam Cardiovascular Sciences, Amsterdam UMC, Location VUmc, 1081 HZ Amsterdam, The Netherlands; [email protected] (M.v.d.L.); [email protected] (T.C.B.); [email protected] (J.M.W.) * Correspondence: [email protected]; Tel.: +31-(0)-20-444-8123 Abstract: The troponin complex is a key regulator of muscle contraction. Multiple variants in skeletal troponin encoding genes result in congenital myopathies. TNNC2 has been implicated in a novel congenital myopathy, TNNI2 and TNNT3 in distal arthrogryposis (DA), and TNNT1 and TNNT3 in nemaline myopathy (NEM). Variants in skeletal troponin encoding genes compromise sarcomere function, e.g., by altering the Ca2+ sensitivity of force or by inducing atrophy. Several potential therapeutic strategies are available to counter the effects of variants, such as troponin activators, introduction of wild-type protein through AAV gene therapy, and myosin modulation to improve muscle contraction. The mechanisms underlying the pathophysiological effects of the variants in skeletal troponin encoding genes are incompletely understood. Furthermore, limited knowledge is available on the structure of skeletal troponin. This review focusses on the physiology of slow and fast skeletal troponin and the pathophysiology of reported variants in skeletal troponin encoding genes. A better understanding of the pathophysiological effects of these variants, together with enhanced knowledge regarding the structure of slow and fast skeletal troponin, will direct the development of Citation: van de Locht, M.; treatment strategies. -

Sarcomeres Regulate Murine Cardiomyocyte Maturation Through MRTF-SRF Signaling
Sarcomeres regulate murine cardiomyocyte maturation through MRTF-SRF signaling Yuxuan Guoa,1,2,3, Yangpo Caoa,1, Blake D. Jardina,1, Isha Sethia,b, Qing Maa, Behzad Moghadaszadehc, Emily C. Troianoc, Neil Mazumdara, Michael A. Trembleya, Eric M. Smalld, Guo-Cheng Yuanb, Alan H. Beggsc, and William T. Pua,e,2 aDepartment of Cardiology, Boston Children’s Hospital, Boston, MA 02115; bDepartment of Biostatistics and Computational Biology, Dana-Farber Cancer Institute, Boston, MA 02215; cDivision of Genetics and Genomics, The Manton Center for Orphan Disease Research, Boston Children’s Hospital and Harvard Medical School, Boston, MA 02115; dAab Cardiovascular Research Institute, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, NY 14642; and eHarvard Stem Cell Institute, Harvard University, Cambridge, MA 02138 Edited by Janet Rossant, The Gairdner Foundation, Toronto, ON, Canada, and approved November 24, 2020 (received for review May 6, 2020) The paucity of knowledge about cardiomyocyte maturation is a Mechanisms that orchestrate ultrastructural and transcrip- major bottleneck in cardiac regenerative medicine. In develop- tional changes in cardiomyocyte maturation are beginning to ment, cardiomyocyte maturation is characterized by orchestrated emerge. Serum response factor (SRF) is a transcription factor that structural, transcriptional, and functional specializations that occur is essential for cardiomyocyte maturation (3). SRF directly acti- mainly at the perinatal stage. Sarcomeres are the key cytoskeletal vates key genes regulating sarcomere assembly, electrophysiology, structures that regulate the ultrastructural maturation of other and mitochondrial metabolism. This transcriptional regulation organelles, but whether sarcomeres modulate the signal trans- subsequently drives the proper morphogenesis of mature ultra- duction pathways that are essential for cardiomyocyte maturation structural features of myofibrils, T-tubules, and mitochondria. -
S1 Table Protein
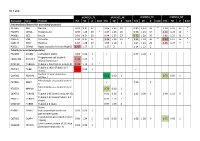
S1 Table dFSHD12_TE dFSHD12_NE aFSHD51_TE aFSHD51_NE Accession Gene Protein H/L SD # bold H/L SD # bold H/L SD # bold H/L SD # bold Intermediate filament (or associated proteins) P17661 DES Desmin 0.91 N.D. 37 1.06 1.35 19 0.89 1,13 33 * 1.20 1.21 17 * P02545 LMNA Prelamin-A/C 0.90 1.25 30 * 1.07 1.26 20 0.96 1.23 34 1.21 1.24 19 * P48681 NES Nestin 0.91 N.D. 60 0.94 1.25 27 0.72 1.20 50 * 0.89 1.27 31 * P08670 VIM Vimentin 1.04 N.D. 35 1.24 1.24 14 * 1.21 1.18 36 * 1.39 1.17 16 * Q15149 PLEC Plectin-1 1.10 1.28 19 1.05 1.10 3 1.07 1.23 26 1.25 1.27 7 * P02511 CRYAB Alpha-crystallin B chain (HspB5) 1.47 1.17 2 1.17 2 1.14 1.12 2 Tubulin (or associated proteins) P62158 CALM1 Calmodulin (CaM) 0.83 0.00 1 0.93 0.00 1 Programmed cell death 6- Q8WUM4 PDCD6IP 1.34 0.00 1 interacting protein Q71U36 TUBA1A Tubulin α-1A chain (α-tubulin 3) 1.44 1.12 3 * Tubulin β chain (Tubulin β-5 P07437 TUBB 1.52 0.00 1 chain) Nuclear mitotic apparatus Q14980 NUMA1 0.68 0.00 1 0.75 0.00 1 protein 1 Microtubule-associated protein P27816 MAP4 1.10 1 4 Microtubule-associated protein P78559 MAP1A 0.76 0.00 1 1A Q6PEY2 TUBA3E Tubulin α-3E chain (α-tubulin 3E) 0.91 0.00 1 1.12 0.00 1 0.98 1.12 3 Tubulin β-2C chain (Tubulin β-2 P68371 TUBB2C 0.93 1.13 7 chain) Q3ZCM7 TUBB8 Tubulin β-8 chain 0.97 1.09 4 Serine P34897 SHMT2 hydroxymethyltransferase 0.93 0.00 1 (serine methylase) Cytoskeleton-associated protein Q07065 CKAP4 0.98 1.24 5 0.96 0.00 1 1.08 1.28 6 0.75 0.00 1 4 (p63) Centrosomal protein of 135 kDa Q66GS9 CEP135 0.84 0.00 1 (Centrosomal protein 4) Pre-B cell leukemia transcription Q96AQ6 PBXIP1 0.74 0.00 1 0.80 1 factor-interacting protein 1 T-complex protein 1 subunit P17897 TCP1 0.84 0.00 1 alpha (CCT-alpha) Cytoplasmic dynein Q13409 DYNC1I2 1.01 0.00 1 intermediate chain 2 (DH IC-2) Dynein heavy chain 3 (Dnahc3- Q8TD57 DNAH3 b) Microtubule-actin cross- linking Q9UPN3 MACF1 factor 1 (Trabeculin-alpha) Actin (or associated including myofibril-associated porteins) P60709 ACTB Actin, cytoplasmic 1 (β-actin) 1.11 N.D. -

Supplementary Materials a Comprehensive Analysis of Gene Expression Changes in a High Replicate and Open-Source Dataset of Diff
Supplementary Materials A comprehensive analysis of gene expression changes in a high replicate and open-source dataset of differentiating hiPSC-derived cardiomyocytes Tanya Grancharova1,2, Kaytlyn A. Gerbin1,2, Alexander B. Rosenberg3,4, Charles M. Roco3,4,5, Joy Arakaki2, Colette DeLizzo2, Stephanie Q. Dinh2, Rory Donovan-Maiye2, Mathew Hirano3, Angelique Nelson2, Joyce Tang2, Julie A. Theriot2,6, Calysta Yan2, Vilas Menon7, Sean P. Palecek8, Georg Seelig3,9, Ruwanthi N. Gunawardane2* 1Authors contributed equally 2Allen Institute for Cell Science, Seattle, WA 3Department of Electrical & Computer Engineering, University of Washington, Seattle, WA 4Parse Biosciences, Seattle, WA 5Department of Bioengineering, University of Washington, Seattle, WA 6Department of Biology and Howard Hughes Medical Institute, University of Washington, Seattle, WA 7Department of Neurology, Columbia University Irving Medical Center, New York, NY 8 Department of Chemical and Biological Engineering, University of Wisconsin - Madison, Madison, WI 9Paul G. Allen School of Computer Science & Engineering, University of Washington, Seattle, WA * corresponding author, [email protected] Supplementary Figure S1 A Protocol 1 Protocol 2 D0 (undifferentiated) D12 D24 D90 D14 D26 WTC-11 TOMM20 TNNI1 WTC-11 TOMM20 TNNI1 WTC-11 TOMM20 TNNI1 WTC-11 TOMM20 TNNI1 WTC-11 TOMM20 TNNI1 WTC-11 TOMM20 TNNI1 Diff Exp1 1 1 1 1 Diff Exp2 1 1 1 1 1 1 Diff Exp3 1 1 1 1 1 1 1 1 Diff Exp4 2 1 2 1 2 1 2 1 Diff Exp5 1 2 1 1 1 2 1 2 1 3 1 2 Diff Exp6 2 1 Diff Exp7 2 Undiff 1 1 Protocol -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Bovine Cardiac Troponin I Gene (TNNI3) As a Candidate Gene for Bovine Dilated Cardiomyopathy
University of Pennsylvania ScholarlyCommons Departmental Papers (Vet) School of Veterinary Medicine 2009 Bovine Cardiac Troponin I Gene (TNNI3) as a Candidate Gene for Bovine Dilated Cardiomyopathy Marta Owczarek-Lipska Gaudenz Dolf Karina E. Guziewicz University of Pennsylvania Tosso Leeb Claude Shelling See next page for additional authors Follow this and additional works at: https://repository.upenn.edu/vet_papers Part of the Large or Food Animal and Equine Medicine Commons Recommended Citation Owczarek-Lipska, M., Dolf, G., Guziewicz, K. E., Leeb, T., Shelling, C., Posthaus, H., & Braunschweig, M. H. (2009). Bovine Cardiac Troponin I Gene (TNNI3) as a Candidate Gene for Bovine Dilated Cardiomyopathy. Archiv Tierzucht (Archives Animal Breeding), 52 (2), 113-123. Retrieved from https://repository.upenn.edu/vet_papers/28 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/vet_papers/28 For more information, please contact [email protected]. Bovine Cardiac Troponin I Gene (TNNI3) as a Candidate Gene for Bovine Dilated Cardiomyopathy Abstract The cardiac troponin complex, which is an important component of the contractile apparatus, is composed of the three subunits troponin I (TnI), troponin C (TnC) and troponin T (TnT). Troponin I is the inhibitory subunit and consists of three isoforms encoded by TNNI1, TNNI2 and TNNI3 genes, respectively. Due to the different types of cardiomyopathies caused by mutations in the TNNI3 gene and its fluorescence in situ hybridization (FISH) mapping on bovine chromosome 18q26, which was shown to be linked to the recessively inherited bovine dilated cardiomyopathy (BDCMP), bovine TNNI3 was considered as candidate gene for BDCMP. Real-time polymerase chain reaction (PCR) TNNI3 expression analysis resulted in a significant difference between BDCMP affected and unaffected animals when normalized to ACTB gene expression, but there was no significant difference in expression when normalized to GAPDH. -

Are These Cardiomyocytes? Protocol Development Reveals Impact of Sample Preparation on the Accuracy of Identifying Cardiomyocytes by Flow Cytometry
bioRxiv preprint doi: https://doi.org/10.1101/388926; this version posted August 9, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Resource Are these cardiomyocytes? Protocol development reveals impact of sample preparation on the accuracy of identifying cardiomyocytes by flow cytometry Matthew Waas1, Ranjuna Weerasekera1, Erin M. Kropp1, Marisol Romero-Tejeda2,3, Ellen Poon4, Kenneth R. Boheler4,5,6, Paul W. Burridge2,3, Rebekah L. Gundry1,7 1Department of Biochemistry, Medical College of Wisconsin, Milwaukee, WI 53226, USA 2Department of Pharmacology, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA 3Center for Pharmacogenomics, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA 4School of Biomedical Sciences, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, China. 5Division of Cardiology, Johns Hopkins University School of Medicine, Baltimore, MD 21205, USA. 6Department of Biomedical Engineering, The Johns Hopkins University, Baltimore, MD 21205, USA. 7Center for Biomedical Mass Spectrometry Research, Medical College of Wisconsin, Milwaukee, WI 53226, USA Corresponding author: Rebekah L. Gundry, PhD Department of Biochemistry Medical College of Wisconsin 8701 Watertown Plank Road Milwaukee, WI, 53226 Telephone: 414-955-2825 Fax: 414-955-6568 Email: [email protected] Running Title: Standard flow cytometry protocol for assessing stem cell-derived cardiomyocytes bioRxiv preprint doi: https://doi.org/10.1101/388926; this version posted August 9, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Alteration of Gene Expression in Mice After Glaucoma Filtration Surgery
www.nature.com/scientificreports OPEN Alteration of gene expression in mice after glaucoma fltration surgery Keisuke Adachi, Yosuke Asada, Toshiaki Hirakata, Miki Onoue, Satoshi Iwamoto, Toshimitsu Kasuga & Akira Matsuda* To clarify the early alterations of gene expression using a mouse model of glaucoma fltration surgery, we carried out microarray expression analysis. Using BALB/c mice, a fltration surgery model was made by incision of the limbal conjunctiva, followed by the insertion of a 33G needle tip into the anterior chamber, and 11-0 nylon sutures. Subgroups of mice were treated intraoperatively with 0.4 mg/ml mitomycin-C (MMC). At day 3 after surgery the bleb was maintained. The bleb region tissue was sampled 3 days after the fltration surgery, and gene expression analysis was carried out using a mouse Agilent 8 × 60 K array. We found 755 hyperexpressed transcripts in the bleb region compared to control conjunctiva. The hyperexpressed transcripts included epithelial cell metaplasia-related (Il1b, Krt16, Sprr1b), infammation-related (Ccl2, Il6) and wound healing-related (Lox, Timp1) genes. We also found downregulation of a goblet cell marker gene (Gp2) in the bleb conjunctiva. MMC treatment suppressed elastin (Eln) gene expression and enhanced keratinization-related gene expression (Krt1, Lor) in the bleb region. Our results suggest the importance of epithelial wound healing after fltration surgery, and this fltration surgery model will be a useful tool for further pathophysiological analysis. Glaucoma is an optic neuropathy characterized by degeneration of retinal ganglion cells and cupping of the optic nerve head as well as visual feld defects1,2. Reduction of intraocular pressure is the method of treatment for glaucoma.