Cardiovascular Failure, Inotropes and Vasopressors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Angiotensin II Protocol
Angiotensin II (Giapreza ™) Protocol Background Sepsis and septic shock are medical emergencies that affect millions of people each year and killing as many as 1 in 4.1 The cornerstones of therapy are fluid resuscitation, early appropriate antibiotics, source control if needed and vasopressors. A small portion of patients fail to respond to these therapies and develop refractory shock. The definition of refractory septic shock varies in the literature but is generally considered to be hypotension, with end-organ dysfunction, requiring high-dose vasopressor support.2 The associated mortality of refractory septic shock is up to 60% and as high as 80-90% in patients requiring more than 1 mcg/kg/min of norepinephrine.2,3 Patients who develop refractory septic shock comprise a very small portion of the population in large randomized controlled trials therefore limited data is available regarding outcomes and management. Indications: Angiotensin II (Ang II) is a vasoconstrictor used to increase blood pressure in adults with septic or other distributive shock. Administration: Starting dose of 5 (nanograms) ng/kg/min intravenously via central line only. Titration: Every 5 minutes by increments of 5 ng/kg/min as needed. Maximum dose should not exceed 80 ng/kg/min (During the first 3 hours of administration); after the first 3 hours the maintenance (maximum) dose is 40 ng/kg/min. Monitoring: Critical care setting only with telemetry, arterial blood pressure, and continuous SpO2 monitoring. DVT Prophylaxis should be started (unless contraindicated) -
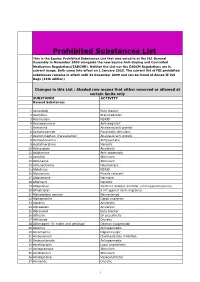
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Pleth Variability Index: a Dynamic Measurement to Help Assess to Help Measurement a Dynamic Index: Variability Pleth Responsiveness and Fluid Physiology
Pleth Variability Index: A Dynamic Measurement to Help Assess TECHNICAL BULLETIN TECHNICAL Physiology and Fluid Responsiveness SUMMARY PVI®, an index available with Masimo SET® pulse oximetry, is the first and only noninvasive, continuous, easy-to-use method to help clinicians manage fluid responsiveness in sedated patients under positive pressure ventilation. Other clinical uses have also been developed for PVI, including helping clinicians to assess the effects of positive end expiratory pressure on cardiac index and to identify patients at risk for hypotension during anesthesia induction. PVI, along with the other innovative noninvasive monitoring technologies available with the Masimo rainbow SET® platform (SpHb®, SpCO®, SpMet®, RRa™), has helped clinicians to realize improved patient outcomes while lowering the cost of care. INTRODUCTION Many pulse oximetry technologies display a processed and filtered representation of the photoplethysmosgraphic waveform. Each manufacturer uses unique proprietary algorithms to calculate the waveform displayed on the pulse oximeter. Masimo has extracted and processed information from the waveform to create two physiologic indices, perfusion index (PI) and pleth variability index (PVI). PI is calculated by indexing the infrared (IR) pulsatile signal against the nonpulsitile signal and expressing this number as a percentage. Masimo SET® PI has been shown to be useful to gauge the severity of illness in newborns1, 2 to assess the effectiveness of epidural blocks3, 4 to indicate successful interscalene nerve block placement in awake patients5 and to quantify peripheral perfusion for diagnosis of congenital heart disease in newborns.6 PVI is the first and only commercially available measurement that automatically and continuously calculates the respiratory variations in the photoplethysmosgraphic waveform. -

(Mibg) Scintigraphy: Procedure Guidelines for Tumour Imaging
Eur J Nucl Med Mol Imaging (2010) 37:2436–2446 DOI 10.1007/s00259-010-1545-7 GUIDELINES 131I/123I-Metaiodobenzylguanidine (mIBG) scintigraphy: procedure guidelines for tumour imaging Emilio Bombardieri & Francesco Giammarile & Cumali Aktolun & Richard P. Baum & Angelika Bischof Delaloye & Lorenzo Maffioli & Roy Moncayo & Luc Mortelmans & Giovanna Pepe & Sven N. Reske & Maria R. Castellani & Arturo Chiti Published online: 20 July 2010 # EANM 2010 Abstract The aim of this document is to provide general existing procedures for neuroendocrine tumours. The information about mIBG scintigraphy in cancer patients. guidelines should therefore not be taken as exclusive of The guidelines describe the mIBG scintigraphy protocol other nuclear medicine modalities that can be used to obtain currently used in clinical routine, but do not include all comparable results. It is important to remember that the The European Association has written and approved guidelines to promote the use of nuclear medicine procedures with high quality. These general recommendations cannot be applied to all patients in all practice settings. The guidelines should not be deemed inclusive of all proper procedures and exclusive of other procedures reasonably directed to obtaining the same results. The spectrum of patients seen in a specialized practice setting may be different than the spectrum usually seen in a more general setting. The appropriateness of a procedure will depend in part on the prevalence of disease in the patient population. In addition, resources available for patient care may vary greatly from one European country or one medical facility to another. For these reasons, guidelines cannot be rigidly applied. These guidelines summarize the views of the Oncology Committee of the EANM and reflect recommendations for which the EANM cannot be held responsible. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

EANM Procedure Guidelines for 131I-Meta-Iodobenzylguanidine (131I-Mibg) Therapy
Eur J Nucl Med Mol Imaging (2008) 35:1039–1047 DOI 10.1007/s00259-008-0715-3 GUIDELINES EANM procedure guidelines for 131I-meta-iodobenzylguanidine (131I-mIBG) therapy Francesco Giammarile & Arturo Chiti & Michael Lassmann & Boudewijn Brans & Glenn Flux Published online: 15 February 2008 # EANM 2008 Abstract Meta-iodobenzylguanidine, or Iobenguane, is an nervous system. The neuroendocrine system is derived from a aralkylguanidine resulting from the combination of the family of cells originating in the neural crest, characterized by benzyl group of bretylium and the guanidine group of an ability to incorporate amine precursors with subsequent guanethidine (an adrenergic neurone blocker). It is a decarboxylation. The purpose of this guideline is to assist noradrenaline (norepinephrine) analogue and so-called nuclear medicine practitioners to evaluate patients who might “false” neurotransmitter. This radiopharmaceutical, labeled be candidates for 131I-meta-iodobenzylguanidine to treat with 131I, could be used as a radiotherapeutic metabolic agent neuro-ectodermal tumours, to provide information for in neuroectodermal tumours, that are derived from the performing this treatment and to understand and evaluate primitive neural crest which develops to form the sympathetic the consequences of therapy. F. Giammarile (*) Keywords Guidelines . Therapy . mIBG CH Lyon Sud, EA 3738, HCL, UCBL, 165 Chemin du Grand Revoyet, Purpose 69495 Pierre Benite Cedex, France e-mail: [email protected] The purpose of this guideline is to assist nuclear medicine A. Chiti practitioners to U.O. di Medicina Nucleare, Istituto Clinico Humanitas, via Manzoni, 56, 1. Evaluate patients who might be candidates for 131I-meta- 20089 Rozzano (MI), Italy iodobenzylguanidine (mIBG) to treat neuro-ectodermal e-mail: [email protected] tumours M. -

Cardiac Work and Contractility J
Br Heart J: first published as 10.1136/hrt.30.4.443 on 1 July 1968. Downloaded from Brit. Heart 7., 1968, 30, 443. Cardiac Work and Contractility J. HAMER* It has been customary to regard the heart as a fibres is needed to maintain the stroke volume in a pump maintaining the flow of blood, and to assess larger ventricle, and ventricular work is correspon- the work done by the heart from the pressure and dingly reduced (Gorlin, 1962). Simple calcula- volume of blood leaving the ventricles. While cor- tions suggest that there is, in fact, little change in rect in physical terms, measurement of external work as the ventricle dilates (Table). The more cardiac work in this way is a poor index of the myo- forceful contraction produced by increased stretch- cardial oxygen consumption which is related to the ing of the muscle fibres through the Starling work done by the ventricular muscle. Systolic mechanism probably gives the dilated ventricle a pressure seems to be a more important determinant functional advantage. of ventricular work than stroke volume, and under Estimates of ventricular work based on force some conditions myocardial oxygen consumption measurements still give an incomplete picture of can be predicted from the systolic pressure, duration myocardial behaviour, as a rapid contraction needs of systole, and heart rate (Sarnoff et al., 1958). more energy than a slow one. The velocity of This relationship does not hold in other situations, contraction of the muscle fibres is an important as ventricular work depends on the force of the con- additional determinant of myocardial oxygen con- traction in the ventricular wall rather than on the sumption (Sonnenblick, 1966). -

Time-Varying Elastance and Left Ventricular Aortic Coupling Keith R
Walley Critical Care (2016) 20:270 DOI 10.1186/s13054-016-1439-6 REVIEW Open Access Left ventricular function: time-varying elastance and left ventricular aortic coupling Keith R. Walley Abstract heart must have special characteristics that allow it to respond appropriately and deliver necessary blood flow Many aspects of left ventricular function are explained and oxygen, even though flow is regulated from outside by considering ventricular pressure–volume characteristics. the heart. Contractility is best measured by the slope, Emax, of the To understand these special cardiac characteristics we end-systolic pressure–volume relationship. Ventricular start with ventricular function curves and show how systole is usefully characterized by a time-varying these curves are generated by underlying ventricular elastance (ΔP/ΔV). An extended area, the pressure– pressure–volume characteristics. Understanding ventricu- volume area, subtended by the ventricular pressure– lar function from a pressure–volume perspective leads to volume loop (useful mechanical work) and the ESPVR consideration of concepts such as time-varying ventricular (energy expended without mechanical work), is linearly elastance and the connection between the work of the related to myocardial oxygen consumption per beat. heart during a cardiac cycle and myocardial oxygen con- For energetically efficient systolic ejection ventricular sumption. Connection of the heart to the arterial circula- elastance should be, and is, matched to aortic elastance. tion is then considered. Diastole and the connection of Without matching, the fraction of energy expended the heart to the venous circulation is considered in an ab- without mechanical work increases and energy is lost breviated form as these relationships, which define how during ejection across the aortic valve. -

Handbook of Drugs in Intensive Care: an A
This page intentionally left blank This page intentionally left blank Handbook of Drugs in Intensive Care Fourth edition This book is dedicated to Georgina Paw Handbook of Drugs in Intensive Care An A-Z Guide Fourth edition Henry G W Paw BPharm MRPharmS MBBS FRCA Consultant in Anaesthesia and Intensive Care York Hospital York Rob Shulman BSc (Pharm) MRPharmS Dip Clin Pham, DHC (Pharm) Lead Pharmacist in Critical Care University College London Hospitals London CAMBRIDGE UNIVERSITY PRESS Cambridge, New York, Melbourne, Madrid, Cape Town, Singapore, São Paulo, Delhi, Dubai, Tokyo Cambridge University Press The Edinburgh Building, Cambridge CB2 8RU, UK Published in the United States of America by Cambridge University Press, New York www.cambridge.org Information on this title: www.cambridge.org/9780521757157 © H. Paw and R. Shulman 2010 This publication is in copyright. Subject to statutory exception and to the provision of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of Cambridge University Press. First published in print format 2010 ISBN-13 978-0-521-75715-7 Paperback Cambridge University Press has no responsibility for the persistence or accuracy of urls for external or third-party internet websites referred to in this publication, and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. CONTENTS Introduction vii How to use this book viii Abbreviations x Acknowledgements xiii DRUGS: An A–Z Guide 1 SHORT NOTES 229 Routes of -

Prodrugs of Morpholine Tachykinin Receptor
Europäisches Patentamt *EP000748320B1* (19) European Patent Office Office européen des brevets (11) EP 0 748 320 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: C07D 413/06, C07D 265/32, of the grant of the patent: C07F 9/6558, A61K 31/535 13.11.2002 Bulletin 2002/46 (86) International application number: (21) Application number: 95912667.3 PCT/US95/02551 (22) Date of filing: 28.02.1995 (87) International publication number: WO 95/023798 (08.09.1995 Gazette 1995/38) (54) PRODRUGS OF MORPHOLINE TACHYKININ RECEPTOR ANTAGONISTS MORPHOLINWIRKSTOFFVORLÄUFER ALS TACHYKININRECEPTORANTAGONISTEN PROMEDICAMENTS A BASE D’ANTAGONISTES DE RECEPTEURS DE LA MORPHOLINE TACHYKININE (84) Designated Contracting States: • MacCOSS, Malcolm AT BE CH DE DK ES FR GB GR IE IT LI LU NL PT Rahway, NJ 07065 (US) SE • MILLS, Sander, G. Designated Extension States: Rahway, NJ 07065 (US) LT SI (74) Representative: Hiscock, Ian James et al (30) Priority: 04.03.1994 US 206771 European Patent Department, Merck & Co., Inc., (43) Date of publication of application: Terlings Park, 18.12.1996 Bulletin 1996/51 Eastwick Road Harlow, Essex CM20 2QR (GB) (73) Proprietor: Merck & Co., Inc. Rahway New Jersey 07065-0900 (US) (56) References cited: EP-A- 0 528 495 EP-A- 0 577 394 (72) Inventors: • DORN, Conrad, P. Remarks: Rahway, NJ 07065 (US) The file contains technical information submitted • HALE, Jeffrey, J. after the application was filed and not included in this Rahway, NJ 07065 (US) specification Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. -

Myocardial Ischemia and Acute Coronary Syndromes
CHAPTER 23 Myocardial Ischemia and Acute Coronary Syndromes Kevin M. Sowinski Myocardial ischemia occurs as a result of increased The specific mechanisms by which drugs may facil- myocardial demand, decreased myocardial oxygen itate or cause MIs will be discussed. supply, or both, and most commonly occurs in An acute coronary syndrome is associated with patients with atherosclerotic coronary artery disease. three clinical manifestations: ST- segment elevation This chapter discusses the specific mechanisms by MI, non-ST- segment elevation MI, and unstable which drug therapy may cause increased myocardial angina.1,2 For the purposes of this chapter, it is dif- oxygen demand or decreased supply. ficult to separate the acute coronary syndromes Angina pectoris is a clinical syndrome of chest because, for the most part, the individual case data discomfort caused by reversible myocardial isch- in the literature do not provide sufficient detail. emia that produces disturbances in myocardial Therefore, in most cases, the specific acute coro- function but no myocardial necrosis. Myocardial nary syndromes will not be discussed separately. ischemia can also occur without any symptoms of Furthermore, based on the available literature, it is angina and is typically referred to as silent myocar- difficult to distinguish drugs based on whether they dial ischemia. Acute myocardial infarction (MI) is a cause myocardial ischemia or infarction. clinical syndrome associated with the development of a prolonged occlusion of a coronary artery lead- CAUSATIVE AGENTS ing to decreased oxygen supply, myocardial isch- emia, and irreversible damage to myocardial tissue. Drugs reported to cause angina pectoris, myocar- MI in patients with coronary artery disease is usu- dial ischemia, an acute coronary syndrome, or all ally associated with a coronary artery thrombosis three are listed in Table 23-1.3-462 Drug- induced superimposed on a ruptured atherosclerotic plaque. -

Pulse Wave Analysis to Estimate Cardiac Output
CLINICAL FOCUS REVIEW Jerrold H. Levy, M.D., F.A.H.A., F.C.C.M., Editor Pulse Wave Analysis to Estimate Cardiac Output Karim Kouz, M.D., Thomas W. L. Scheeren, M.D., Daniel de Backer, M.D., Bernd Saugel, M.D. ardiac output (CO)–guided therapy is a promising reference CO value measured using an indicator dilution Capproach to hemodynamic management in high-risk method (transpulmonary thermodilution or lithium dilu- patients having major surgery1 and in critically ill patients tion).5,9 CO measurement using indicator dilution methods with circulatory shock.2 Pulmonary artery thermodilu- requires a (central) venous catheter for indicator injection tion remains the clinical reference method for CO mea- upstream in the circulation and a dedicated arterial catheter Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/134/1/119/513741/20210100.0-00023.pdf by guest on 29 September 2021 surement,3 but the use of the pulmonary artery catheter and measurement system to detect downstream indicator decreased over the past two decades.4 Today, various CO temperature or concentration changes.5,9–11 monitoring methods with different degrees of invasiveness The VolumeView system (Edwards Lifesciences, are available, including pulse wave analysis.5 Pulse wave USA) and the PiCCO system (Pulsion Medical Systems, analysis is the mathematical analysis of the arterial blood Germany) calibrate pulse wave analysis–derived CO to pressure waveform and enables CO to be estimated con- transpulmonary thermodilution–derived CO. To measure tinuously and in real time.6 In this article, we review pulse CO using transpulmonary thermodilution, a bolus of cold wave analysis methods for CO estimation, including their crystalloid solution is injected in the central venous circu- underlying measurement principles and their clinical appli- lation.10 The cold indicator bolus injection causes changes cation in perioperative and intensive care medicine.