Chapter 6.1 Arsenic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Identification and Quantification of Arsenic Species in Gold Mine Wastes Using Synchrotron-Based X-Ray Techniques
Identification and Quantification of Arsenic Species in Gold Mine Wastes Using Synchrotron-Based X-ray Techniques Andrea L. Foster, PhD U.S. Geological Survey GMEG Menlo Park, CA Arsenic is an element of concern in mined gold deposits around the world Spenceville (Cu-Au-Ag) Lava Cap (Nevada) Ketza River (Au) Empire Mine (Nevada) low-sulfide, qtz Au sulfide and oxide ore Argonaut Mine (Au) bodies Don Pedro Harvard/Jamestown Ruth Mine (Cu) Kelly/Rand (Au/Ag) Goldenville, Caribou, and Montague (Au) The common arsenic-rich particles in hard-rock gold mines have long been known Primary Secondary Secondary/Tertiary Iron oxyhydroxide (“rust”) “arsenian” pyrite containing arsenic up to 20 wt% -1 Scorodite FeAsO 2H O As pyrite Fe(As,S)2 4 2 Kankite : FeAsO4•3.5H2O Reich and Becker (2006): maximum of 6% As-1 Arseniosiderite Ca2Fe3(AsO4)3O2·3H2O Arsenopyrite FeAsS Jarosite KFe3(SO4)2(OH)6 Yukonite Ca7Fe12(AsO4)10(OH)20•15H2O Tooleite [Fe6(AsO3)4(SO4)(OH)4•4H2O Pharmacosiderite KFe (AsO ) (OH) •6–7H O arsenide n- 4 4 3 4 2 n = 1-3 But it is still difficult to predict with an acceptable degree of uncertainty which forms will be present • thermodynamic data lacking or unreliable for many important phases • kinetic barriers to equilibrium • changing geochemical conditions (tailings management) Langmuir et al. (2006) GCA v70 Lava Cap Mine Superfund Site, Nevada Cty, CA Typical exposure pathways at arsenic-contaminated sites are linked to particles and their dissolution in aqueous fluids ingestion of arsenic-bearing water dissolution near-neutral, low -

Arsenic and Lead Contamination in Oklahoma Soils Arsenic and Lead Are Naturally Occurring Elements Present in Rocks
Arsenic and Lead Contamination in Oklahoma Soils Arsenic and lead are naturally occurring elements present in rocks. As these rocks erode, arsenic and lead get in soils, waters and plants. The United States Geological Survey (USGS) reports an average of 7.4 parts per million (ppm) as the arsenic concentration in soils for the entire United States and 7.2 ppm as the average arsenic concentration in soils for the western U.S.(1) Background arsenic concentrations in Central Oklahoma soils range from 0.6 to 21 ppm.(2) The USGS reports an average lead concentration of 13 parts per million (ppm) in soils for central Oklahoma(2) and an average lead concentration of 18 ppm for the Western United States.(3) Pollution from historic lead and zinc smelters in Oklahoma left residues of lead, arsenic and cadmium in area soils. Contamination was also spread by using smelter debris as fill material, driveways and roads. These former smelters were primarily located in eastern Oklahoma. Some arsenic contamination above naturally occurring levels is also attributed to agricultural, energy and industrial practices. For example, arsenic-containing insecticides and herbicides were widely used on vegetables, fruits and field crops from the 1900s to around 1950. Coal combustion, wood preserving and smelting operations are known to be sources of arsenic contamination.(1) Lead was once commonly used in paint and in plumbing. Lead was an additive to gasoline for many years and has also been found in ceramics, mini-blinds and other products. Homes built before 1970 commonly have lead-based paint. Renovation activities and peeling or flaking paint can release lead inside the home. -

The Calcium Arsenates
Station RuIletin 131. June, 1918 Oregon Agricultural College Experiment Station AGRICULTURAL CHEMISTRY DEPARTMENT The Calcium Arsenates By R. H. ROBINSON Acting Chemist, Oregon Agricultural Experiment Station. CORVALLIS, OREGON The regular huIlejne of the Station are sent free to the residents of Oregon who request them. THE CALCIUM ARSENATES By R. H. ROBINSON Acting Chemist, Oregon Agricultural Experiment Station INTRODUCTION Chemical investigations on the calcium arsenates relative to their economfic value and practicability as insecticides have been carried on by the department of Agricultural Chemistry of this Station during the past two years.The results obtained from these investigations are presented in this bulletin.The work was supported by the annual funds provided by the Adams Act of the United States Government.. Commercial calcium arsenate is an arsenical now being produced by reliable manufacturers of spray material and offered for sale as a sub- stitute for the arsenates of lead.The value of the latter as a stomachic insecticide has been demonstrated, and itis now used extensively for the successful controlof the codling moth, the destructionof the cotton boll worm., the tobacco worm, and the Colorado potato beetle. Previous inveatigations on the toxic values and killing power of calcium arsenate and lead arsenate indicate equal efficiency. A consideration of a few figures will show the economic advantages which might be gained if calcium arsenate could be substituted for lead arsenate.A conservative estimate of the quantity of lead arsenate used annually in the United States, as stated by one of the largest manufac- turers of spray materials, is probably more than 30,000,000 pounds. -

Arsenic Summary & Details: Greenfacts
http://www.greenfacts.org/ Copyright © GreenFacts page 1/9 Scientific Facts on Source document: IPCS (2001) Arsenic Summary & Details: GreenFacts Level 2 - Details on Arsenic 1. What is arsenic?.............................................................................................................3 1.1 What are the properties of arsenic?...................................................................................3 1.2 How are arsenic levels measured?.....................................................................................3 2. Where does environmental arsenic come from?....................................................3 2.1 What are the natural sources of environmental arsenic?.......................................................3 2.2 What are the man-made sources of environmental arsenic?..................................................4 2.3 How is arsenic transported and distributed in the environment?............................................4 3. What are the levels of exposure to arsenic?...........................................................4 3.1 How much arsenic is there in the environment?..................................................................4 3.2 What levels of arsenic are found in living organisms?...........................................................5 3.3 What levels of arsenic are humans exposed to?..................................................................5 4. What happens to arsenic in the body?......................................................................6 4.1 -

The Development of the Periodic Table and Its Consequences Citation: J
Firenze University Press www.fupress.com/substantia The Development of the Periodic Table and its Consequences Citation: J. Emsley (2019) The Devel- opment of the Periodic Table and its Consequences. Substantia 3(2) Suppl. 5: 15-27. doi: 10.13128/Substantia-297 John Emsley Copyright: © 2019 J. Emsley. This is Alameda Lodge, 23a Alameda Road, Ampthill, MK45 2LA, UK an open access, peer-reviewed article E-mail: [email protected] published by Firenze University Press (http://www.fupress.com/substantia) and distributed under the terms of the Abstract. Chemistry is fortunate among the sciences in having an icon that is instant- Creative Commons Attribution License, ly recognisable around the world: the periodic table. The United Nations has deemed which permits unrestricted use, distri- 2019 to be the International Year of the Periodic Table, in commemoration of the 150th bution, and reproduction in any medi- anniversary of the first paper in which it appeared. That had been written by a Russian um, provided the original author and chemist, Dmitri Mendeleev, and was published in May 1869. Since then, there have source are credited. been many versions of the table, but one format has come to be the most widely used Data Availability Statement: All rel- and is to be seen everywhere. The route to this preferred form of the table makes an evant data are within the paper and its interesting story. Supporting Information files. Keywords. Periodic table, Mendeleev, Newlands, Deming, Seaborg. Competing Interests: The Author(s) declare(s) no conflict of interest. INTRODUCTION There are hundreds of periodic tables but the one that is widely repro- duced has the approval of the International Union of Pure and Applied Chemistry (IUPAC) and is shown in Fig.1. -

United States Patent Office
Patented Mar. 12, 1946 2,396.465 UNITED STATES PATENT OFFICE PREPARATION OF SODUMARSENTE Erroll Hay Karr, Tacoma, Wash, assignor to The Pennsylvania Salt Manufacturing Company, Philadelphia, Pa, a corporation of Pennsyl vania No Drawing. Application October 12, 1943, Serial No. 506,00 3 Claims. (C. 23-53) This invention relates to the production of metal arsenites from alkali metal hydroxide and high arsenic content water soluble, alkali metal arsenic trioxide without the necessity of using arsenites, and more particularly, it relates to an the alkali metal hydroxide in powder form. improved method of causing a controlled reac Another object of the invention is to provide tion between an alkali metal hydroxide and a cheap and easily performed process for the arsenic trioxide to obtain a granular product in preparation of alkali metal arsenites from con a one-step operation. centrated solutions of caustic alkali and pow It is known that solid sodium arsenite can be dered arsenic trioxide in standard mixing equip prepared by mixing together powdered Solid ment. caustic soda and arsenic oxide in a heap and O An additional object of the invention is to pro initiating the reaction by adding a small quan vide a process for obtaining alkali metal arsenites tity of water. Ullmann's Encyclopedia der Techn. in granular form from concentrated solutions of Chemie., volume I, page 588. This method will caustic alkali and powdered arsenic trioxide. yield a solid material but it is attended by sev A further object of the invention is to provide eral disadvantages. 5 a process for the preparation of granular alkali . -

Arsenic Trioxide Is Highly Cytotoxic to Small Cell Lung Carcinoma Cells
160 Arsenic trioxide is highly cytotoxic to small cell lung carcinoma cells 1 1 Helen M. Pettersson, Alexander Pietras, effect of As2O3 on SCLC growth, as suggested by an Matilda Munksgaard Persson,1 Jenny Karlsson,1 increase in neuroendocrine markers in cultured cells. [Mol Leif Johansson,2 Maria C. Shoshan,3 Cancer Ther 2009;8(1):160–70] and Sven Pa˚hlman1 1Center for Molecular Pathology, CREATE Health and 2Division of Introduction Pathology, Department of Laboratory Medicine, Lund University, 3 Lung cancer is the most frequent cause of cancer deaths University Hospital MAS, Malmo¨, Sweden; and Department of f Oncology-Pathology, Cancer Center Karolinska, Karolinska worldwide and results in 1 million deaths each year (1). Institute and Hospital, Stockholm, Sweden Despite novel treatment strategies, the 5-year survival rate of lung cancer patients is only f15%. Small cell lung carcinoma (SCLC) accounts for 15% to 20% of all lung Abstract cancers diagnosed and is a very aggressive malignancy Small cell lung carcinoma (SCLC) is an extremely with early metastatic spread (2). Despite an initially high aggressive form of cancer and current treatment protocols rate of response to chemotherapy, which currently com- are insufficient. SCLC have neuroendocrine characteristics bines a platinum-based drug with another cytotoxic drug and show phenotypical similarities to the childhood tumor (3, 4), relapses occur in the absolute majority of SCLC neuroblastoma. As multidrug-resistant neuroblastoma patients. At relapse, the efficacy of further chemotherapy is cells are highly sensitive to arsenic trioxide (As2O3) poor and the need for alternative treatments is obvious. in vitro and in vivo, we here studied the cytotoxic effects Arsenic-containing compounds have been used in tradi- of As2O3 on SCLC cells. -

APPENDIX G Acid Dissociation Constants
harxxxxx_App-G.qxd 3/8/10 1:34 PM Page AP11 APPENDIX G Acid Dissociation Constants § ϭ 0.1 M 0 ؍ (Ionic strength ( † ‡ † Name Structure* pKa Ka pKa ϫ Ϫ5 Acetic acid CH3CO2H 4.756 1.75 10 4.56 (ethanoic acid) N ϩ H3 ϫ Ϫ3 Alanine CHCH3 2.344 (CO2H) 4.53 10 2.33 ϫ Ϫ10 9.868 (NH3) 1.36 10 9.71 CO2H ϩ Ϫ5 Aminobenzene NH3 4.601 2.51 ϫ 10 4.64 (aniline) ϪO SNϩ Ϫ4 4-Aminobenzenesulfonic acid 3 H3 3.232 5.86 ϫ 10 3.01 (sulfanilic acid) ϩ NH3 ϫ Ϫ3 2-Aminobenzoic acid 2.08 (CO2H) 8.3 10 2.01 ϫ Ϫ5 (anthranilic acid) 4.96 (NH3) 1.10 10 4.78 CO2H ϩ 2-Aminoethanethiol HSCH2CH2NH3 —— 8.21 (SH) (2-mercaptoethylamine) —— 10.73 (NH3) ϩ ϫ Ϫ10 2-Aminoethanol HOCH2CH2NH3 9.498 3.18 10 9.52 (ethanolamine) O H ϫ Ϫ5 4.70 (NH3) (20°) 2.0 10 4.74 2-Aminophenol Ϫ 9.97 (OH) (20°) 1.05 ϫ 10 10 9.87 ϩ NH3 ϩ ϫ Ϫ10 Ammonia NH4 9.245 5.69 10 9.26 N ϩ H3 N ϩ H2 ϫ Ϫ2 1.823 (CO2H) 1.50 10 2.03 CHCH CH CH NHC ϫ Ϫ9 Arginine 2 2 2 8.991 (NH3) 1.02 10 9.00 NH —— (NH2) —— (12.1) CO2H 2 O Ϫ 2.24 5.8 ϫ 10 3 2.15 Ϫ Arsenic acid HO As OH 6.96 1.10 ϫ 10 7 6.65 Ϫ (hydrogen arsenate) (11.50) 3.2 ϫ 10 12 (11.18) OH ϫ Ϫ10 Arsenious acid As(OH)3 9.29 5.1 10 9.14 (hydrogen arsenite) N ϩ O H3 Asparagine CHCH2CNH2 —— —— 2.16 (CO2H) —— —— 8.73 (NH3) CO2H *Each acid is written in its protonated form. -

Chemical Name Federal P Code CAS Registry Number Acutely
Acutely / Extremely Hazardous Waste List Federal P CAS Registry Acutely / Extremely Chemical Name Code Number Hazardous 4,7-Methano-1H-indene, 1,4,5,6,7,8,8-heptachloro-3a,4,7,7a-tetrahydro- P059 76-44-8 Acutely Hazardous 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide P050 115-29-7 Acutely Hazardous Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- P197 17702-57-7 Acutely Hazardous 1-(o-Chlorophenyl)thiourea P026 5344-82-1 Acutely Hazardous 1-(o-Chlorophenyl)thiourea 5344-82-1 Extremely Hazardous 1,1,1-Trichloro-2, -bis(p-methoxyphenyl)ethane Extremely Hazardous 1,1a,2,2,3,3a,4,5,5,5a,5b,6-Dodecachlorooctahydro-1,3,4-metheno-1H-cyclobuta (cd) pentalene, Dechlorane Extremely Hazardous 1,1a,3,3a,4,5,5,5a,5b,6-Decachloro--octahydro-1,2,4-metheno-2H-cyclobuta (cd) pentalen-2- one, chlorecone Extremely Hazardous 1,1-Dimethylhydrazine 57-14-7 Extremely Hazardous 1,2,3,4,10,10-Hexachloro-6,7-epoxy-1,4,4,4a,5,6,7,8,8a-octahydro-1,4-endo-endo-5,8- dimethanonaph-thalene Extremely Hazardous 1,2,3-Propanetriol, trinitrate P081 55-63-0 Acutely Hazardous 1,2,3-Propanetriol, trinitrate 55-63-0 Extremely Hazardous 1,2,4,5,6,7,8,8-Octachloro-4,7-methano-3a,4,7,7a-tetra- hydro- indane Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]- 51-43-4 Extremely Hazardous 1,2-Benzenediol, 4-[1-hydroxy-2-(methylamino)ethyl]-, P042 51-43-4 Acutely Hazardous 1,2-Dibromo-3-chloropropane 96-12-8 Extremely Hazardous 1,2-Propylenimine P067 75-55-8 Acutely Hazardous 1,2-Propylenimine 75-55-8 Extremely Hazardous 1,3,4,5,6,7,8,8-Octachloro-1,3,3a,4,7,7a-hexahydro-4,7-methanoisobenzofuran Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime 26419-73-8 Extremely Hazardous 1,3-Dithiolane-2-carboxaldehyde, 2,4-dimethyl-, O- [(methylamino)-carbonyl]oxime. -

Chromium, Copper and Arsenic Oxide)-Treated Wood Hata, T.; Bronsveld, Paulus; Vystavel, T.; Kooi, Bart; De Hosson, J.T.M.; Kakitani, T.; Otono, A.; Imamura, Y
University of Groningen Electron microscopic study on pyrolysis of CCA (chromium, copper and arsenic oxide)-treated wood Hata, T.; Bronsveld, Paulus; Vystavel, T.; Kooi, Bart; De Hosson, J.T.M.; Kakitani, T.; Otono, A.; Imamura, Y. Published in: Journal of Analytical and Applied Pyrolysis DOI: 10.1016/S0165-2370(03)00077-9 IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2003 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Hata, T., Bronsveld, P. M., Vystavel, T., Kooi, B. J., de Hosson, J. T. M., Kakitani, T., ... Imamura, Y. (2003). Electron microscopic study on pyrolysis of CCA (chromium, copper and arsenic oxide)-treated wood. Journal of Analytical and Applied Pyrolysis, 68-9(1), 635-643. DOI: 10.1016/S0165-2370(03)00077-9 Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. -

Step-By-Step Guide to Better Laboratory Management Practices
Step-by-Step Guide to Better Laboratory Management Practices Prepared by The Washington State Department of Ecology Hazardous Waste and Toxics Reduction Program Publication No. 97- 431 Revised January 2003 Printed on recycled paper For additional copies of this document, contact: Department of Ecology Publications Distribution Center PO Box 47600 Olympia, WA 98504-7600 (360) 407-7472 or 1 (800) 633-7585 or contact your regional office: Department of Ecology’s Regional Offices (425) 649-7000 (509) 575-2490 (509) 329-3400 (360) 407-6300 The Department of Ecology is an equal opportunity agency and does not discriminate on the basis of race, creed, color, disability, age, religion, national origin, sex, marital status, disabled veteran’s status, Vietnam Era veteran’s status or sexual orientation. If you have special accommodation needs, or require this document in an alternate format, contact the Hazardous Waste and Toxics Reduction Program at (360)407-6700 (voice) or 711 or (800) 833-6388 (TTY). Table of Contents Introduction ....................................................................................................................................iii Section 1 Laboratory Hazardous Waste Management ...........................................................1 Designating Dangerous Waste................................................................................................1 Counting Wastes .......................................................................................................................8 Treatment by Generator...........................................................................................................12 -
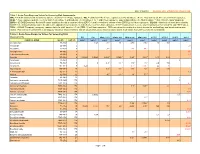
Table 2. Acute Dose-Response Values for Screening Risk Assessments
Date: 6/18/2018 Revisions since 9/18/2014 are shown in red. Table 2. Acute Dose-Response Values for Screening Risk Assessments. MRL = ATSDR minumum risk levels for no adverse effects for 1 to 14-day exposures. REL = California EPA reference exposure level for no adverse effects. Most, but not all, RELs are for 1-hour exposures. AEGL = Acute exposure guideline levels for mild effects (AEGL-1) and moderate effects (AEGL-2) for 1- and 8-hour exposures. Superscripts indicate the AEGL's status: f = final, i=interim, and p=proposed. ERPG = US DOE Emergency Removal Program guidelines for mild or transient effects (ERPG-1) and irreversible or serious effects (ERPG-2) for 1-hour exposures. IDLH/10 = One-tenth of levels determined by NIOSH to be imminently dangerous to life and health, approximately comparable to mild effects levels for 1-hour exposures. IDLH/10 values shown here are only for substances that lack AEGL and ERPG values. TEEL = US DOE Temporary emergency exposure limits for mild, transient effects (TEEL-1) for 1-hour exposures. TEELs are derived according to a tiered, formula-like methodology, and do not undergo peer review. They are not recommended as the basis for regulatory desision-making, and are shown here only to inform situations where acute values from other sources are not available. Table 2. Acute Dose-Response Values for Screening Risk Assessments MRL REL AEGL-1 (1-h) AEGL-1 (8-h) AEGL-2 (1-h) AEGL-2 (8-h) ERPG-1 ERPG-2 IDLH/10 TEEL-1 CHEMICAL NAME CAS NO.