ESKAPE Pathogens Among Pediatric Patients in Iraq
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Detection of ESKAPE Pathogens and Clostridioides Difficile in Simulated
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Detection of ESKAPE pathogens and Clostridioides difficile in 2 Simulated Skin Transmission Events with Metagenomic and 3 Metatranscriptomic Sequencing 4 5 Krista L. Ternusa#, Nicolette C. Keplingera, Anthony D. Kappella, Gene D. Godboldb, Veena 6 Palsikara, Carlos A. Acevedoa, Katharina L. Webera, Danielle S. LeSassiera, Kathleen Q. 7 Schultea, Nicole M. Westfalla, and F. Curtis Hewitta 8 9 aSignature Science, LLC, 8329 North Mopac Expressway, Austin, Texas, USA 10 bSignature Science, LLC, 1670 Discovery Drive, Charlottesville, VA, USA 11 12 #Address correspondence to Krista L. Ternus, [email protected] 13 14 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 15 1 Abstract 16 Background: Antimicrobial resistance is a significant global threat, posing major public health 17 risks and economic costs to healthcare systems. Bacterial cultures are typically used to diagnose 18 healthcare-acquired infections (HAI); however, culture-dependent methods provide limited 19 presence/absence information and are not applicable to all pathogens. -

ESKAPE Pathogens in Animals and Their Antimicrobial Drug Resistance Pattern
Journal of Dairy & Veterinary Sciences ISSN: 2573-2196 Research Article Dairy and Vet Sci J Volume 7 Issue 3 - August 2018 Copyright © All rights are reserved by Bhoj R Singh DOI: 10.19080/JDVS.2018.07.555715 ESKAPE Pathogens in Animals and their Antimicrobial Drug Resistance Pattern Bhoj R Singh* Division of Epidemiology, ICAR-Indian Veterinary Research Institute, India Submission: July 27, 2018; Published: August 24, 2018 *Corresponding author: Bhoj R Singh, Head, Division of Epidemiology, ICAR-Indian Veterinary Research Institute, Izatnagar-243122, Bareilly, UP, India. Phone: +91-8449033222, Email: Abstract The analytical study, of 3240 bacterial isolates from veterinary clinical cases and related sources since 2011 to 2017, aimed to understand the extent of infections in animals associated with ESKAPE group (439) of pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) and to map their antimicrobial sensitivity pattern. All the six ESKAPE pathogens caused infection in animals, the most common being Enterobacter species followed by K. pneumoniae, P. aeruginosa S. aureus, E. faecium and A. baumannii. None of the antibiotics was effective on all the ESKAPE bacterial isolates however, carbapenems (80.4%), tigecycline (76.8%), chloramphenicol (75.8%) and cefepimes (74.6%) inhibited majority of the isolates. More than 76% ESKAPE bacteria had E. faceium (87.5%) and P. aeruginosa multiple drug resistance (MDR), significantly (p, <=0.05) more P. aeruginosa common isolates in but cinnamaldehyde could inhibit (94.5%)almost 98% isolates. of P. aeruginosaMetallo-β- andlactamase >90% (MBL)isolates and of otherextended ESKAPE spectrum-β-lactamase bacteria (except E. (ESBL)faecium production). -

ESKAPE Pathogens
Right Solutions • Right Partner alsenvironmental.co.uk TECHNICAL DATASHEET ESKAPE Pathogens Understanding Nosocomial Risk Factors endocarditis. The monitoring of water used in care homes and healthcare facilities is covered by several pieces of Health Klebsiella pneumoniae and Safety Guidance (HSG). The majority of the guidance In nosocomial settings, Klebsiella bacteria can be spread through is on the monitoring of Legionella and is supported by person-to-person contact or by contamination of the environment; it the Approved Code of Practice for Legionella (ACoP L8) is important to note that the bacteria are not spread through the air. and Health Technical Memorandums (HTM); however, Patients in healthcare settings may be exposed to Klebsiella when there are a range of other risk factors that need to they are on ventilators, or have intravenous catheters or wounds. Unfortunately, these medical tools and conditions may allow be considered in nosocomial scenarios. The ESKAPE Klebsiella to enter the body and cause infection; which can be fatal pathogens are emerging pathogens of concern. in the immuno-compromised. ALS Environmental are able to offer rapid identification of these bacteria using our revolutionary MALDI-ToF confirmation technique. Acinetobacter baumannii The ESKAPE Pathogens are: Acinetobacter baumannii is a rapidly emerging pathogen in the health care system. A. baumannii is usually introduced into a Enterococcus faecium hospital by a colonised patient. Due to it’s ability to survive on artificial surfaces and resist desiccation it can survive and potentially Enterococcus faecium; formerly known as Streptococcus faecium infect new patients for some time. It is suspected that A. baumannii until its re-categorization in 1984, is a human pathogen that causes growth favours nosocomial settings due to the constant use of nosocomial bacteremia, surgical wound infection, endocarditis, and antibiotics by patients in the hospital and causes a wide range of urinary tract infections. -

Structure of ATP Synthase from ESKAPE Pathogen Acinetobacter Baumannii
bioRxiv preprint doi: https://doi.org/10.1101/2021.07.10.451757; this version posted July 11, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Structure of ATP synthase from ESKAPE pathogen Acinetobacter baumannii Julius K Demmer*,1, Ben P Phillips*,1, O Lisa Uhrig1, Alain Filloux2, Luke P Allsopp2,3, Maike Bublitz4, Thomas MeierŦ,1,5 1 Department of Life Sciences Imperial College London Exhibition Road London SW7 2AZ, United Kingdom 2MRC Centre for Molecular Bacteriology and Infection Department of Life Sciences Imperial College London London SW7 2AZ, United Kingdom 3National Heart and Lung Institute Imperial College, London, UK 4Department of Biochemistry University of Oxford South Parks Road Oxford OX1 3QU, United Kingdom 5Private University in the Principality of Liechtenstein Triesen, Liechtenstein *These authors contributed equally. Ŧcorresponding author: Thomas Meier [email protected] One sentence summary: Structure of Acinetobacter baumannii ATP synthase Keywords: F1Fo-ATP synthase, Acinetobacter baumannii, electron cryo-microscopy (cryo- EM), drug target, ESKAPE, multidrug resistance (MDR), extensively drug resistance (XDR), bioenergetics Abbreviations: Adenosine-5’-triphosphate: ATP, electron cryo-microscopy: cryo-EM, multi drug resistance: MDR, extensively drug resistance (XDR) 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.07.10.451757; this version posted July 11, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Acinetobacter baumannii is a clinically relevant pathogen which causes multi-drug resistant, hospital-acquired infections and is a top priority target for antibiotic development. -

Interplay Between ESKAPE Pathogens and Immunity in Skin Infections: an Overview of the Major Determinants of Virulence and Antibiotic Resistance
pathogens Review Interplay between ESKAPE Pathogens and Immunity in Skin Infections: An Overview of the Major Determinants of Virulence and Antibiotic Resistance Gustavo Henrique Rodrigues Vale de Macedo 1,2 , Gabrielle Damasceno Evangelista Costa 1,2, Elane Rodrigues Oliveira 2, Glauciane Viera Damasceno 2, Juliana Silva Pereira Mendonça 1,2, Lucas dos Santos Silva 2, Vitor Lopes Chagas 2, José Manuel Noguera Bazán 3, Amanda Silva dos Santos Aliança 4, Rita de Cássia Mendonça de Miranda 1,5 , Adrielle Zagmignan 2, Andrea de Souza Monteiro 1,6 and Luís Cláudio Nascimento da Silva 1,2,3,* 1 Programa de Pós-graduação em Biologia Microbiana, Universidade CEUMA, 65075-120 São Luís, Brazil; [email protected] (G.H.R.V.d.M.); [email protected] (G.D.E.C.); [email protected] (J.S.P.M.); [email protected] (R.d.C.M.d.M.); [email protected] (A.d.S.M.) 2 Laboratório de Patogenicidade Microbiana, Universidade CEUMA, 65075-120 São Luís, Brazil; [email protected] (E.R.O.); [email protected] (G.V.D.); [email protected] (L.d.S.S.); [email protected] (V.L.C.); [email protected] (A.Z.) 3 Programa de Pós-graduação em Odontologia, Universidade CEUMA, 65075-120 São Luís, Brazil; [email protected] 4 Programa de Pós-graduação em Gestão de Programas e Serviços de Saúde, Universidade CEUMA, 65075-120 São Luís, Brazil; [email protected] Citation: Vale de Macedo, G.H.R.; 5 Programa de Pós-graduação em Meio Ambiente, Universidade CEUMA, 65075-120 São Luís, Brazil Costa, G.D.E.; Oliveira, E.R.; 6 Laboratório de Microbiologia Aplicada, Universidade CEUMA, 65075-120 São Luís, Brazil Damasceno, G.V.; Mendonça, J.S.P.; * Correspondence: [email protected] Silva, L.d.S.; Chagas, V.L.; Bazán, J.M.N.; Aliança, A.S.d.S.; Miranda, Abstract: The skin is the largest organ in the human body, acting as a physical and immunological R.d.C.M.d.; et al. -
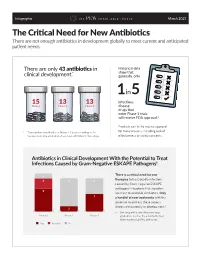
The Critical Need for New Antibiotics There Are Not Enough Antibiotics in Development Globally to Meet Current and Anticipated Patient Needs
Infographic March 2021 The Critical Need for New Antibiotics There are not enough antibiotics in development globally to meet current and anticipated patient needs. There are only 43 antibiotics in Historical data * show that, clinical development. generally, only 1 in 5 15 13 13 infectious Phase 1 Phase 2 Phase 3 disease drugs that enter Phase 1 trials will receive FDA approval.1 Products can fail to receive approval * Total number of antibiotics in Phases 1-3 does not add up to 43 for many reasons, including lack of because new drug applications have been submitted for two drugs. effectiveness or safety concerns. Antibiotics in Clinical Development With the Potential to Treat Infections Caused by Gram-Negative ESKAPE Pathogens† 2 There is a critical need for new therapies to treat deadly infections 4 11 6 caused by Gram-negative ESKAPE pathogens2—bacteria that are often 9 resistant to available antibiotics. Only 7 a handful of new treatments with the potential to address these serious threats are currently in development.3 2 † One drug with a submitted new drug Phase 1 Phase 2 Phase 3 application also has the potential to treat Gram-negative ESKAPE pathogens. Yes Possibly No Critical threat pathogens The World Health Organization considers three bacteria—all of which are resistant to last-line carbapenem antibiotics—to be critical threats to public health. These pathogens—carbapenem-resistant/ESBL-producing Enterobacteriaceae (CRE), Pseudomonas aeruginosa (CRPA), and Acinetobacter baumannii (CRAB)4—often cause severe complications in hospitalized patients, with up to 50 percent of patients dying from bloodstream infections caused by CRE.5 There is an urgent need to address these critical threats, but only 15 antibiotics in development have the potential to treat infections caused by these bacteria. -

ESKAPE Pathogens, Usually Associated with Hospitals, Currently Make up Most of the Antibiotic-Resistant Infections
FINDING LIFE-SAVING MICROBES Angelica Prado Diaz RI: Life Science Lab - BSC Meghan McCarthy 1005L – 039 Anjali Etwaru 04/18/2018 The Antibiotic Crisis • After penicillin’s discovery, there was a breakthrough in antibiotic research. • By the 1980s, many thought infectious disease was a thing of the past. • After the 1980s, no new or different classes of antibiotics have been discovered (Pew Charitable Trusts, 2016). http://www.smallworldinitiative.org/meme-contest-entries/ “If we don’t act, antibiotic resistance will • There has been an increasing level of kill more people than cancer & diabetes bacterial resistance to antibiotics which is combined by 2050” a severe threat to our global health. (CDC, 2016) • Students from all over the world are encouraged to use their local soil to try to discover new antibiotics. • Billions of microbes - both good and bad - inhabit Earth. • Most new antibiotics come from soil bacteria or fungi. • In SWI, students dig up soil, isolate Source:https://static1.squarespace.com/static/555cec2ae4b0902ed19d910b/t/5781e6f3c534a5d68f225213/14681311 their bacteria, and test it for antibiotic 18335/Western+Alabama+Symposium+Cover.jpg?format=1500w characteristics. ESKAPE Pathogens, usually associated with hospitals, currently make up most of the antibiotic-resistant infections. Enterococcus faecium Staphylococcus aureus Klebsiella pneumoniae Acinetobacter baumannii Pseudomonas aeruginosa Enterobacter species Source: https://www.popsci.com/sites/popsci.com/files/styles/1000_1x_/public/images/2017/09/deposit_photo- _worldmap_pills_small.jpg?itok=BmWQy8EB&fc=50,50 SWI Experiments • Lab 1 - There are billions of bacteria found in even a handful of soil. First, we each dug up some soil. Lab 2 - In order to see our bacteria more easily, we had to dilute our soil. -

An Acinetobacter Trilogy
EJMED, European Journal of Medical and Health Sciences Vol. 1, No. 4, September 2019 Biofilm Measurement, Site Specific Variation in Biofilm Production, Biofilm Typing: An Acinetobacter Trilogy Baishali Chakraborty, Dibyendu Banerjee, and Shubhankar Mukherjee In the year 2006, New Delhi Metallo betalactamase (NDM) Abstract—Acinetobacter baumannii is a member of the emerged in India and later the bacteria carrying this gene ESKAPE pathogens, notorious for causing multidrug resistant became known as ‘Superbugs’, which became a worldwide nosocomial infections worldwide. Biofilm has an important role threat. In this category, Pseudomonas aeruginosa was the 1st in its persistence and spread in hospital environment, as well as its multidrug resistance potential. The present study was aimed known superbug. Presently, Acinetobacter baumannii is an at finding out whether the strength of Biofilm formation varies important member of this club among others. with infection of different organs / system. A total of 136 isolates Colistin resistance (chromosomal mediated), was of Acinetobacter baumannii were taken from a variety of there in the earlier days, which became nil due to long disuse samples. Strength of Biofilm formation, determined by Tissue of this drug. Colistin again came into use in recent years in culture plate method, was graded according to OD value in cases where the bacteria were resistant to all other antibiotics. ELISA reader as nil, moderate and strong. It was seen that association between variations in biofilm forming capacity The year 2015 saw the emergence of 1st plasmid mediated depending on different sites of infection was statistically polymyxin resistance mechanism, MCR-1, in significant. We suggest biofilm typing by this method for this Enterobacteriaceae. -

Predictions for ’09: What’S Old Is New Again
10 INFECTIOUS DISEASES JANUARY 2009 • PEDIATRIC NEWS ID CONSULT Predictions for ’09: What’s Old Is New Again appy 2009! It’s time for the an- Klebsiella, Acinetobacter baumannii, a standing order to give vaccine to moth- rose again. There is concern that pro- nual look into the future of in- Pseudomonas aeruginosa, and Enterobacter ers before hospital discharge (if they have longed deferral of the Hib booster in the Hfectious diseases. species—which together are responsible not received a tetanus-containing vac- United States may produce similar re- Two common themes were evident for two-thirds of all health care–associat- cine in the past 2 years, or prior Tdap). sults, so be on the look out. last year: increasing antibiotic resistance, ed infections. While a few new drugs are Ǡ The new improved pneumococcal Ǡ Most physicians are still unaware of and changing epidemiology and vaccine- available or coming for MRSA, there are conjugate vaccine may be closer than the new guidelines for subacute bacteri- preventable infections. Last few that target gram-negative you think. The emergence of multidrug- al prophylaxis. In 2007, the American year’s predictions that were pathogens. For more informa- resistant serotype 19A disease has chal- Heart Association issued the first major on the mark included the rise tion, check out the article by lenged the management of pneumococ- revision of these guidelines and endorsed in pneumococcal serotype Dr. Helen Boucher of Tufts cal infection from acute suppurative antimicrobial prophylaxis for only five 19A, the drop in rotavirus cas- University (Clin. Infect. Dis. otitis media to more serious infections circumstances: prosthetic heart valves, es, the lack of a national so- 2009;48:1-12). -
The Search for Antibiotics
The Search For Antibiotics BY: ASLEY, ELIANA, ISABELLA AND LUNISCHA BSC1005 LAB 4/18/2018 The Need for New Antibiotics Antibiotic crisis An antibiotic is a chemical that kills bacteria. Since the 1980s, there have been no new discoveries of antibiotics Bacteria is becoming resistant to the antibiotics we currently have In the United States, there are over 2 million drug- resistant bacterial illnesses 23,000 deaths and $35 billion in economic losses per YEAR (CDC,2015) “If no significant action is taken by 2050, super bugs will kill more people than cancer and diabetes COMBINED and will result in 300 million premature deaths.” –World Health Organization SWI (Small World Initiative) Small World Initiative A program that encourages students from schools around the world to help discover new antibiotics Established by Dr. Jo Handelsman in 2012 To date there are about 275 schools around the world participating in SWI program Allows credit to go to the student if antibiotics are developed with their soil Soil Microbes Soil Microbes Source of 2/3 of antibiotics today, this includes: bacteria, and fungi. Fun Fact: There are more microbes in a teaspoon of soil than there are people on the earth. Soils contain about 8 to 15 tons of bacteria, fungi, protozoa, nematodes, earthworms, and arthropods. ESKAPE Pathogens ESKAPE pathogens Bacterial infections that ESKAPE Pathogens Corresponding Safe Relatives Acinetobacter baumannii Acinetobacter baylyi are resistant to Enterobacter* Enterobacter aerogenes antibiotics Enterococcus faecium -
Anti-Pathogenic Efficacy of Biogenic Silver Nanoparticles Through
Anti-pathogenic ecacy of biogenic silver nanoparticles through adherence and biolm inhibition in multidrug resistant ESKAPE pathogens Mohd Hashim Khan B S Abdur Rahman Crescent Institute of Science & Technology Sneha Unnikrishnan B S Abdur Rahman Crescent Institute of Science & Technology Karthikeyan Ramalingam ( [email protected] ) B S Abdur Rahman Crescent Institute of Science & Technology https://orcid.org/0000-0002-9334-427X Research article Keywords: ESKAPE pathogens, biogenic AgNPs, anti-pathogenic activity, Live/dead assay, biolm formation Posted Date: August 28th, 2019 DOI: https://doi.org/10.21203/rs.2.13646/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/24 Abstract Background The current study aimed to produce AgNPs through a biogenic approach and assessed for their signicant anti-pathogenic activities against multi-drug resistant ESKAPE pathogens. The biogenic AgNPs were synthesized through non-toxic manner and characterized by using UV-vis, XRD, DLS, TGA- DTA, FTIR, SEM along with EDX and UHRTEM were used to determine the absorption spectra, shape, size, thermal behaviour, functional groups, morphology, elemental constituents and dened particle size distribution prole, respectively. The AgNPs were evaluated for their anti-pathogenic effects against eleven strains of multi drug resistant ESKAPE pathogens by growth inhibition, biolm adhesion, growth kinetics and Live/dead assays.Results The inhibitory range of AgNPs concentration was investigated as higher zones at escalating concentration (50 to 200 µg/ml). The growth kinetics of inhibition of all tested pathogens occurred after 4 hrs of treatment with AgNPs. Adherence assay exhibited highest inhibition in E. -

Antibiotic Resistant Infection of the Bacterial Group ESKAPE
z Available online at http://www.sjomr.org SCIENTIFIC JOURNAL OF MEDICAL RESEARCH Vo. x, Issue x, pp xx - xx, Winter Vol. 2, Issue 8, pp2018 166 -171, Autumn 2018 ISSN: 2520-5234 ORIGINAL ARTICLE Antibiotic Resistant Infection of the Bacterial Group ESKAPE Dunea W. Khaled 1 and Basima A. Abdullah 2 1,2 Department of Microbiology, College of Science, University of Mosul, Mosul, Iraq. ARTICLE INFORMATIONS ABSTRACT Article History: Objectives: The antibiotic resistant infection of six bacterial species have Submitted: 15 August 2018 been designated as 'Red Alert' human pathogens, which are responsible for Revised version received: 2/3 of all hospital acquired infection, they are grouped under acronym 8 September 2018 Accepted: 12 September 2018 ESKAPE which include: 1- Enterococcus faecim or faecalis, 2- Published online: x December 2018 Staphylococcus aureus, 3- Klebsiella pneumoniae, 4- Acinetobacter baumannii, 5- Pseudomonas aeruginosa, 6- Enterobacter spp. For the first Key words: time as group in Mosul and Duhok / Iraq. ESKAPE Antibiotic-resistant Methods: Three hundred and thirty-two samples from different sources as HAIs Urine, Blood, Wounds, Burn, High Vaginal Swab (H.V.S.), Throat Mosul infection, Nose infection, Cerebrospinal fluid (C.S.F.) and Sputum were Duhok collected from hospital patients in city of Mosul and Duhok in Iraq. These samples were cultured on blood and Macconkey's agar. The bacterial Corresponding author: Dunea W. Khaled colonies were purified and identified to species level using morphological, Email: [email protected] Biochemical tests , API and confirmed by Vitek 2 System and antibiotic Department of Microbiology sensitivity was carried out using Vitek 2 System.