Risk of Type 2 Diabetes Is Lower in US Adults Taking Chromium-Containing Supplements1–3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Does Dietary Fiber Affect the Levels of Nutritional Components After Feed Formulation?
fibers Article Does Dietary Fiber Affect the Levels of Nutritional Components after Feed Formulation? Seidu Adams 1 ID , Cornelius Tlotliso Sello 2, Gui-Xin Qin 1,3,4, Dongsheng Che 1,3,4,* and Rui Han 1,3,4 1 College of Animal Science and Technology, Jilin Agricultural University, Changchun 130118, China; [email protected] (S.A.); [email protected] (G.-X.Q.); [email protected] (R.H.) 2 College of Animal Science and Technology, Department of Animal Genetics, Breeding and Reproduction, Jilin Agricultural University, Changchun 130118, China; [email protected] 3 Key Laboratory of Animal Production, Product Quality and Security, Jilin Agricultural University, Ministry of Education, Changchun 130118, China 4 Jilin Provincial Key Laboratory of Animal Nutrition and Feed Science, Jilin Agricultural University, Changchun 130118, China * Correspondence: [email protected]; Tel.: +86-136-4431-9554 Received: 12 January 2018; Accepted: 25 April 2018; Published: 7 May 2018 Abstract: Studies on dietary fiber and nutrient bioavailability have gained an increasing interest in both human and animal nutrition. Questions are increasingly being asked regarding the faith of nutrient components such as proteins, minerals, vitamins, and lipids after feed formulation. The aim of this review is to evaluate the evidence with the perspective of fiber usage in feed formulation. The consumption of dietary fiber may affect the absorption of nutrients in different ways. The physicochemical factors of dietary fiber, such as fermentation, bulking ability, binding ability, viscosity and gel formation, water-holding capacity and solubility affect nutrient absorption. The dietary fiber intake influences the different methods in which nutrients are absorbed. -

Co-Administration of Iron and a Bioavailable Curcumin Supplement Increases Serum BDNF Levels in Healthy Adults
antioxidants Article Co-Administration of Iron and a Bioavailable Curcumin Supplement Increases Serum BDNF Levels in Healthy Adults 1, 1, 1,2 3 Helena Tiekou Lorinczova y, Owen Fitzsimons y, Leah Mursaleen , Derek Renshaw , Gulshanara Begum 1 and Mohammed Gulrez Zariwala 1,* 1 School of Life Sciences, University of Westminster, 115 New Cavendish Street, London W1W 6UW, UK; [email protected] (H.T.L.); [email protected] (O.F.); [email protected] (L.M.); [email protected] (G.B.) 2 The Cure Parkinson’s Trust, 120 New Cavendish St, Fitzrovia, London W1W 6XX, UK 3 Centre for Sport, Exercise and Life Sciences, Faculty of Health and Life Sciences, Coventry University, Priory St, Coventry CV1 5FB, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-20-7911-5000 (ext. 65086) These authors contributed equally to this work. y Received: 19 June 2020; Accepted: 16 July 2020; Published: 22 July 2020 Abstract: Brain-derived neurotrophic factor (BDNF) is key for the maintenance of normal neuronal function and energy homeostasis and has been suggested to improve cognitive function, including learning and memory. Iron and the antioxidant curcumin have been shown to influence BDNF homeostasis. This 6-week, double blind, randomized, placebo-controlled study examined the effects of oral iron supplementation at low (18 mg) and high (65 mg) ferrous (FS) iron dosages, compared to a combination of these iron doses with a bioavailable formulated form of curcumin (HydroCurcTM; 500 mg) on BDNF levels in a healthy adult cohort of 155 male (26.42 years 0.55) and female ± (25.82 years 0.54) participants. -

Iron and Physical Activity: Bioavailability Enhancers, Properties of Black Pepper (Bioperine®) and Potential Applications
nutrients Review Iron and Physical Activity: Bioavailability Enhancers, Properties of Black Pepper (Bioperine®) and Potential Applications Diego Fernández-Lázaro 1,* , Juan Mielgo-Ayuso 2 , Alfredo Córdova Martínez 2 and Jesús Seco-Calvo 3 1 Department of Cellular Biology, Histology and PHArmacology, Faculty of Health Sciences, University of Valladolid, Campus de Soria, 42003 Soria, Spain 2 Department of Biochemistry, Molecular Biology and Physiology, Faculty of Health Sciences, University of Valladolid, Campus de Soria, 42003 Soria, Spain; [email protected] (J.M.-A.); [email protected] (A.C.M.) 3 Institute of Biomedicine (IBIOMED), Physiotherapy Department, University of Leon, Visiting Researcher of Basque Country University, Campus de Vegazana, 24071 Leon, Spain; [email protected] * Correspondence: [email protected]; Tel.: +34-975-129-185 Received: 17 April 2020; Accepted: 22 June 2020; Published: 24 June 2020 Abstract: Black pepper (Piper nigrum L.) has been employed in medicine (epilepsy, headaches, and diabetes), where its effects are mainly attributed to a nitrogen alkaloid called piperidine (1-(1-[1,3-benzodioxol-5-yl]-1-oxo-2,4 pentenyl) piperidine). Piperine co-administered with vitamins and minerals has improved its absorption. Therefore, this study aimed to describe the impact of the joint administration of iron (Fe) plus black pepper in physically active healthy individuals. Fe is a micronutrient that aids athletic performance by influencing the physiological functions involved in endurance sports by improving the transport, storage, and utilization of oxygen. Consequently, athletes have risk factors for Fe depletion, Fe deficiency, and eventually, anemia, mainly from mechanical hemolysis, gastrointestinal disturbances, and loss of Fe through excessive sweating. -

Ferronyl™ Iron Supplement
™ ferronyl iron supplement introduction Iron deficiency continues to be a concern around benefits of ferronyl™ the world, especially in women and children, often iron supplement resulting in anemia.1 One approach to prevent iron deficiency is supplementation of food, vitamins, ¢ low use levels and nutritional products.2 When selecting an iron ¢ higher bioavailabilty source for supplementation it is important to consider ¢ easy to formulate bioavailability, toxicity, potential side effects, iron ¢ generally recognized as safe (GRAS) content, taste and ease of formulation. Ferronyl™ iron supplement is an ideal source of essentially pure iron with minimal metallic taste and excellent bioavailability demonstrated in preclinical studies.3,4,5 Thus, it is the physical and chemical properties 6,7 better choice for iron supplementation formulators. product description Ferronyl™ iron supplement powder is elemental iron (Fe) Ferronyl™ iron supplement is elemental iron with high (> 98%) iron content. High iron content enables manufactured by the chemical decomposition of iron lower use levels to achieve the same daily intake levels pentacarbonyl. The resulting iron particles are small, compared with ferrous (Fe2+) salts (e.g., ferrous sulfate, uniform spheres of high purity with only traces of carbon, ferrous fumarate or ferrous gluconate). This is important oxygen and nitrogen. in multivitamin formulations where smaller tablets are preferred to encourage consumer use, but are often chemical description elemental iron difficult to achieve with the -

Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Pharmacological Approach to Sleep Disturbances in Autism Spectrum Disorders with Psychiatric Comorbidities: a Literature Review
medical sciences Review Pharmacological Approach to Sleep Disturbances in Autism Spectrum Disorders with Psychiatric Comorbidities: A Literature Review Sachin Relia 1,* and Vijayabharathi Ekambaram 2,* 1 Department of Psychiatry, University of Tennessee Health Sciences Center, 920, Madison Avenue, Suite 200, Memphis, TN 38105, USA 2 Department of Psychiatry, University of Oklahoma Health Sciences Center, 920, Stanton L Young Blvd, Oklahoma City, OK 73104, USA * Correspondence: [email protected] (S.R.); [email protected] (V.E.); Tel.: +1-901-448-4266 (S.R.); +1-405-271-5251 (V.E.); Fax: +1-901-297-6337 (S.R.); +1-405-271-3808 (V.E.) Received: 15 August 2018; Accepted: 17 October 2018; Published: 25 October 2018 Abstract: Autism is a developmental disability that can cause significant emotional, social and behavioral dysfunction. Sleep disorders co-occur in approximately half of the patients with autism spectrum disorder (ASD). Sleep problems in individuals with ASD have also been associated with poor social interaction, increased stereotypy, problems in communication, and overall autistic behavior. Behavioral interventions are considered a primary modality of treatment. There is limited evidence for psychopharmacological treatments in autism; however, these are frequently prescribed. Melatonin, antipsychotics, antidepressants, and α agonists have generally been used with melatonin, having a relatively large body of evidence. Further research and information are needed to guide and individualize treatment for this population group. Keywords: autism spectrum disorder; sleep disorders in ASD; medications for sleep disorders in ASD; comorbidities in ASD 1. Introduction Autism is a developmental disability that can cause significant emotional, social, and behavioral dysfunction. According to the Diagnostic and Statistical Manual (DSM-V) classification [1], autism spectrum disorder (ASD) is characterized by persistent deficits in domains of social communication, social interaction, restricted and repetitive patterns of behavior, interests, or activities. -
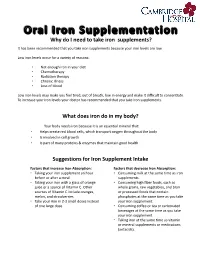
Why Do I Need to Take Iron Supplements? It Has Been Recommended That You Take Iron Supplements Because Your Iron Levels Are Low
Why do I need to take iron supplements? It has been recommended that you take iron supplements because your iron levels are low. Low iron levels occur for a variety of reasons: • Not enough iron in your diet • Chemotherapy • Radiation therapy • Chronic illness • Loss of blood Low iron levels may make you feel tired, out of breath, low in energy and make it difficult to concentrate. To increase your iron levels your doctor has recommended that you take iron supplements. What does iron do in my body? Your body needs iron because it is an essential mineral that: • Helps create red blood cells, which transport oxygen throughout the body • Is involved in cell growth • Is part of many proteins & enzymes that maintain good health Suggestions for Iron Supplement Intake Factors that increase Iron Absorption: Factors that decrease Iron Absorption: • Taking your iron supplement an hour • Consuming milk at the same time as iron before or after a meal supplements. • Taking your iron with a glass of orange • Consuming high fiber foods, such as juice or a source of Vitamin C .Other whole grains, raw vegetables, and bran sources of Vitamin C include oranges, or processed foods that contain melon, and strawberries. phosphates at the same time as you take • Take your iron in 2-3 small doses instead your iron supplement. of one large dose. • Consuming coffee or tea or carbonated beverages at the same time as you take your iron supplement • Taking iron at the same time as vitamin or mineral supplements or medications (antacids). Side Effects of Iron Supplements Iron supplements will increase your energy levels however they sometimes cause these side effects: • Constipation • Nausea • Vomiting • Dark coloured stools • Diarrhea • Abdominal discomfort Tips to Minimize Side Effects • Start with half the recommended dose and gradually increase to full dose • If the iron is making you nauseous take it with a meal. -

Dopamine and Iron in the Pathophysiology of Restless Legs Syndrome (RLS)
Sleep Medicine 5 (2004) 385–391 www.elsevier.com/locate/sleep Udine Special Section Dopamine and iron in the pathophysiology of restless legs syndrome (RLS) Richard Allen* Neurology and Sleep Medicine, Johns Hopkins Bayview Medical Center, Asthma and Allergy Bldg 1B46b, 5501 Hopkins Bayview Circle, Baltimore, MD 21224, USA Received 1 January 2003; accepted 15 October 2003 Abstract Background and purpose: The evaluation of the pathophysiology of restless legs syndrome (RLS) stems largely from recognition of the information provided by both pharmacological treatment of the disorder and the secondary forms of the disorder. This article examines the pathophysiological implications of each of these clinical aspects of RLS. Patients and methods: The article reviews the existing literature in relation to possible pathology suggested by the clinical data. It will then explore other data supporting each of the possible pathologies and examine the relationships between these pathologies. Results: The pharmacological treatment data strongly support a dopaminergic abnormality for RLS. Other pharmacological data and some imaging data also support this, although the data are not entirely consistent. The secondary forms of RLS strongly support an iron deficiency abnormality for RLS, further documented by several other studies. Some animal studies have shown a relation between iron deficiency and dopaminergic abnormalities that have some similarity to those seen in the RLS patient. Conclusions: It is concluded that there may be an iron–dopamine connection central to the pathophysiology of RLS for at least some if not most patients with this disorder. q 2004 Elsevier B.V. All rights reserved. Keywords: Restless legs syndrome; Dopamine; Iron; Pathophysiology; Ferritin; CSF 1. -

Nutrition- Focused Physical Assessment in Pediatric Chronic Disease Ellen Mccloy, MS, RD, CNSC Esther Berenhaut, RD, CSP, CSR
Nutrition- Focused Physical Assessment in Pediatric Chronic Disease Ellen McCloy, MS, RD, CNSC Esther Berenhaut, RD, CSP, CSR, CNSC Objectives • Identify common physical assessment indicators in pediatric chronic disease. • Identify physical signs of micronutrient deficiencies common in pediatric chronic disease. Chronic Kidney Disease Cerebral Palsy Inborn Errors of Metabolism CHRONIC KIDNEY DISEASE Pediatric CKD Overview • Congenital vs Glomerular – Congenital disorders have earlier onset • Growth failure is most frequent and severe with congenital renal anomalies and when the onset of CKD is during the first two years of life – 50% of a child’s growth occurs during this time and is mostly dependent on nutritional status – Glomerular • Focal segmental glomerular sclerosis is the most prevalent acquired renal disease in children – Increasing in pediatrics due to obesity Chronic Malnutrition • Disease related – Uremia, metabolic acidosis – Polyuria – Altered mineral metabolism – Growth hormone – Reflux – Anemia – Frequent catabolic illness • Non-disease related – Feeds held for surgeries – Late placement of Gtube Common Physical Findings • Short stature • Pallor • Body mass/habitus • Bowed legs, poor posture • Large abdomen, thin limbs Other Nutrient Concerns • Wounds • Micronutrients – Carnitine – Zinc Nutrition Interventions • Uremia -> decrease protein load, if appropriate • Metabolic acidosis -> correct acidosis with alkalizing agent • Polyuria -> replace renal losses (sodium, sometimes potassium, etc) • Altered mineral metabolism -

Good Neighbor Script
Good Neighbor Script INSPIRATION FOR LIVING WELL FROM GOOD NEIGHBOR PHARMACY | MARCH 2021 5 Ways to Make the Most of Your Vitamins HEALTH & FITNESS When it comes to getting the vitamins and minerals your body needs, it’s important to eat a healthy, balanced diet. However, taking vitamins is a good insurance policy — a way to make sure that you’re not — missing out on important nutrients, especially if you have a chronic medical condition or eat a restricted diet. Here’s how to make the most of your vitamin routine. 3 Ways to Use Probiotics 1. Take your multivitamin with food. your liver and fat tissues. Therefore, it takes a long for Better Health According to Harvard Health, a daily multivitamin is time for your body to get rid of any excess, and useful for people who don’t get adequate nutrition overdosing is possible. If you take a multivitamin, Although many people think of bacteria as through food, whether due to a restricted diet or make sure that it doesn’t have more than the RDA harmful and unhealthy, certain types are good a condition that increases their nutrient needs. for all four fat-soluble vitamins. Most don’t. Due for your health. According to the National Because certain vitamins are helpful only when to the risk of overdose, most people should avoid Institutes of Health (NIH), probiotics are taken with food, it’s best to take your multivitamin taking individual fat-soluble vitamin supplements microorganisms containing several types of with a meal or snack. Vitamins A, D, E and K are unless told otherwise by a doctor. -

Iron Supplement
What you need to know if your physician has recommended an extra iron supplement Iron Iron is a mineral that is stored primarily in your liver, but it's also stored in your bone marrow, spleen and muscles. Iron is essential because it helps your red blood cells (RBC) carry and deliver oxygen to other parts of your body, as well as aiding in energy production. Iron is another nutrient that pregnant women need more of. This is due to the increased volume of blood supply during pregnancy to accommodate a woman's unborn child. Women already have an increased need for iron because of menstrual periods; pregnancy just adds to this need. Supplements Depending upon the type of supplement you're considering, you may find iron (Slow Fe) and folic acid (Folate) in a multi‐blend or as individual supplements. Almost any drug store or retail store will carry multivitamins, prenatal vitamins and individual supplements. It's very important that you do not rely on the supplement alone to supply your need for a particular vitamin or mineral as they are merely a supplement to your daily food intake. They are not meant to supply your daily needs on a regular basis. Supplements only help complete your daily recommended allowance if you do not get enough of them during the day. Recommended Dosage During normal pregnancy, the recommended intake of iron is 27 milligrams (mg) a day. Women between the ages of 19 and 50 who aren't pregnant need only 18 mg a day, and women age 51 and older and all adult men need around 8 mg a day. -

Taking Iron Supplements
Oxford University Hospitals NHS Trust Taking Iron Supplements Information for patients Why do I need to take iron supplements? We have recommended that you take iron supplements because you are anaemic or at risk of developing anaemia. This is because the iron stores in your body are low. How do the supplements work? Iron is needed for the production of haemoglobin, which is an essential ingredient in red blood cells. Haemoglobin is very important, as it carries oxygen from the lungs to the rest of the body. If you don’t have enough iron you can develop anaemia, which means you aren’t making enough red blood cells to carry oxygen around your body. You may become breathless, tired and have a lack of energy, your skin may become pale and you may have palpitations (noticeable heartbeats). Which types of iron supplements are available? The main types of iron supplements used are: • ferrous sulphate (high strength tablets) • ferrous fumarate (high strength tablets or syrup) • ferrous gluconate (medium strength tablets) • Sytron® syrup (sodium feredetate) (low strength). How do I take them? You should take your iron supplement on an empty stomach (preferably one hour before a meal) with a drink containing vitamin C, such as a glass of orange juice or another juice drink with added vitamin C. Why is the way I take them important? Absorption of iron from the gut is reduced by food, tea and milk, so these should be avoided for one hour before and after taking the iron supplement. Some medications also affect absorption of iron from the gut, particularly medications which reduce stomach acid (antacids) and certain antibiotics.