Dysbindin-1 Involvement in the Etiology of Schizophrenia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mouse Germ Line Mutations Due to Retrotransposon Insertions Liane Gagnier1, Victoria P
Gagnier et al. Mobile DNA (2019) 10:15 https://doi.org/10.1186/s13100-019-0157-4 REVIEW Open Access Mouse germ line mutations due to retrotransposon insertions Liane Gagnier1, Victoria P. Belancio2 and Dixie L. Mager1* Abstract Transposable element (TE) insertions are responsible for a significant fraction of spontaneous germ line mutations reported in inbred mouse strains. This major contribution of TEs to the mutational landscape in mouse contrasts with the situation in human, where their relative contribution as germ line insertional mutagens is much lower. In this focussed review, we provide comprehensive lists of TE-induced mouse mutations, discuss the different TE types involved in these insertional mutations and elaborate on particularly interesting cases. We also discuss differences and similarities between the mutational role of TEs in mice and humans. Keywords: Endogenous retroviruses, Long terminal repeats, Long interspersed elements, Short interspersed elements, Germ line mutation, Inbred mice, Insertional mutagenesis, Transcriptional interference Background promoter and polyadenylation motifs and often a splice The mouse and human genomes harbor similar types of donor site [10, 11]. Sequences of full-length ERVs can TEs that have been discussed in many reviews, to which encode gag, pol and sometimes env, although groups of we refer the reader for more in depth and general infor- LTR retrotransposons with little or no retroviral hom- mation [1–9]. In general, both human and mouse con- ology also exist [6–9]. While not the subject of this re- tain ancient families of DNA transposons, none view, ERV LTRs can often act as cellular enhancers or currently active, which comprise 1–3% of these genomes promoters, creating chimeric transcripts with genes, and as well as many families or groups of retrotransposons, have been implicated in other regulatory functions [11– which have caused all the TE insertional mutations in 13]. -

Mapping Our Genes—Genome Projects: How Big? How Fast?
Mapping Our Genes—Genome Projects: How Big? How Fast? April 1988 NTIS order #PB88-212402 Recommended Citation: U.S. Congress, Office of Technology Assessment, Mapping Our Genes-The Genmne Projects.’ How Big, How Fast? OTA-BA-373 (Washington, DC: U.S. Government Printing Office, April 1988). Library of Congress Catalog Card Number 87-619898 For sale by the Superintendent of Documents U.S. Government Printing Office, Washington, DC 20402-9325 (order form can be found in the back of this report) Foreword For the past 2 years, scientific and technical journals in biology and medicine have extensively covered a debate about whether and how to determine the function and order of human genes on human chromosomes and when to determine the sequence of molecular building blocks that comprise DNA in those chromosomes. In 1987, these issues rose to become part of the public agenda. The debate involves science, technol- ogy, and politics. Congress is responsible for ‘(writing the rules” of what various Federal agencies do and for funding their work. This report surveys the points made so far in the debate, focusing on those that most directly influence the policy options facing the U.S. Congress, The House Committee on Energy and Commerce requested that OTA undertake the project. The House Committee on Science, Space, and Technology, the Senate Com- mittee on Labor and Human Resources, and the Senate Committee on Energy and Natu- ral Resources also asked OTA to address specific points of concern to them. Congres- sional interest focused on several issues: ● how to assess the rationales for conducting human genome projects, ● how to fund human genome projects (at what level and through which mech- anisms), ● how to coordinate the scientific and technical programs of the several Federal agencies and private interests already supporting various genome projects, and ● how to strike a balance regarding the impact of genome projects on international scientific cooperation and international economic competition in biotechnology. -
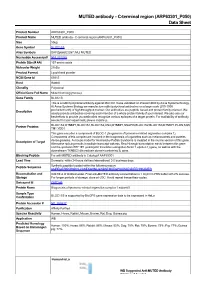
MUTED Antibody - C-Terminal Region (ARP63301 P050) Data Sheet
MUTED antibody - C-terminal region (ARP63301_P050) Data Sheet Product Number ARP63301_P050 Product Name MUTED antibody - C-terminal region (ARP63301_P050) Size 50ug Gene Symbol BLOC1S5 Alias Symbols DKFZp686E2287; MU; MUTED Nucleotide Accession# NM_201280 Protein Size (# AA) 187 amino acids Molecular Weight 21kDa Product Format Lyophilized powder NCBI Gene Id 63915 Host Rabbit Clonality Polyclonal Official Gene Full Name Muted homolog (mouse) Gene Family BLOC1S This is a rabbit polyclonal antibody against MUTED. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Partner Proteins BLOC1S2,DTNBP1,BLOC1S1,BLOC1S2,CNO,DTNBP1,SNAPIN,BLOC1S2,BLOC1S3,DTNBP1,PLDN,SQS TM1,YOD1 This gene encodes a component of BLOC-1 (biogenesis of lysosome-related organelles complex 1). Components of this complex are involved in the biogenesis of organelles such as melanosomes and platelet- Description of Target dense granules. A mouse model for Hermansky-Pudlak Syndrome is mutated in the murine version of this gene. Alternative splicing results in multiple transcript variants. Read-through transcription exists between this gene and the upstream EEF1E1 (eukaryotic translation elongation factor 1 epsilon 1) gene, as well as with the downstream TXNDC5 (thioredoxin domain containing 5) gene. -

Product Information
Product information PLDN, 1-172aa Human, His-tagged, Recombinant, E.coli Cat. No. IBATGP1472 Full name: pallidin NCBI Accession No.: NP_036520 Synonyms: HPS9, PA, PALLID Description: PLDN (Pallidin) may play a role in intracellular vesicle trafficking. It interacts with Syntaxin 13 which mediates intracellular membrane fusion. Several alternatively spliced transcript variants of this gene have been described, but the full-length nature of some of these variants has not been determined. This protein involved in the development of lysosome-related organelles, such as melanosomes and platelet-dense granules. PLDN has been shown to interact with BLOC1S1, STX12, Dysbindin, CNO, BLOC1S2, MUTED and SNAPAP. Recombinant human PLDN protein, fused to His-tag at N-terminus, was expressed in E.coli and purified by using conventional chromatography techniques. Form: Liquid. In 20mM Tris-HCl buffer (pH 8.0) containing 2mM DTT, 10% glycerol, 100mM NaCl Molecular Weight: 21.9kDa (192aa), confirmed by MALDI-TOF (Molecular weight on SDS-PAGE will appear higher) Purity: > 90% by SDS - PAGE Concentration: 1mg/ml (determined by Bradford assay) 15% SDS-PAGE (3ug) Sequences of amino acids: MGSSHHHHHH SSGLVPRGSH MSVPGPSSPD GALTRPPYCL EAGEPTPGLS DTSPDEGLIE DLTIEDKAVE QLAEGLLSHY LPDLQRSKQA LQELTQNQVV LLDTLEQEIS KFKECHSMLD INALFAEAKH YHAKLVNIRK EMLMLHEKTS KLKKRALKLQ QKRQKEELER EQQREKEFER EKQLTARPAK RM General references: Huang L, et al. (1999). Nat Genet 23 (3): 329–32. Moriyama K., et al. (2002) Traffic 3:666-677 Storage: Can be stored at +4°C short term (1-2 weeks). For long term storage, aliquot and store at -20°C or -70°C. Avoid repeated freezing and thawing cycles. For research use only. This product is not intended or approved for human, diagnostics or veterinary use. -

Impaired Maturation of Large Dense-Core Vesicles in Muted
ß 2015. Published by The Company of Biologists Ltd | Journal of Cell Science (2015) 128, 1365–1374 doi:10.1242/jcs.161414 RESEARCH ARTICLE Impaired maturation of large dense-core vesicles in muted-deficient adrenal chromaffin cells Zhenhua Hao1,2, Lisi Wei3, Yaqin Feng1,4, Xiaowei Chen3, Wen Du5, Jing Ma1, Zhuan Zhou3, Liangyi Chen3 and Wei Li1,6,* ABSTRACT Previous studies have suggested that the granin family plays an important role in LDCV biogenesis (Kim et al., 2001), but the The large dense-core vesicle (LDCV), a type of lysosome-related machinery for granin sorting into LDCVs is largely unknown. organelle, is involved in the secretion of hormones and The adaptor protein-3 (AP-3) complex is likely involved in granin neuropeptides in specialized secretory cells. The granin family is a sorting into immature LDCVs. In AP-3-deficient chromaffin driving force in LDCV biogenesis, but the machinery for granin sorting cells, LDCVs contain less granins, chromogranin A (CgA, also to this biogenesis pathway is largely unknown. The mu mutant known as CHGA) and secretogranin II (SgII, also known as mouse, which carries a spontaneous null mutation on the Muted gene SCG2), and exhibit enlarged size, decreased number and an (also known as Bloc1s5), which encodes a subunit of the biogenesis increase in releasing quantal size (i.e. the amount of transmitter of lysosome-related organelles complex-1 (BLOC-1), is a mouse released per vesicle) (Asensio et al., 2010; Grabner et al., 2006). model of Hermansky–Pudlak syndrome. Here, we found that LDCVs AP-3 and the HOPS complex interact physically and might act in were enlarged in mu adrenal chromaffin cells. -

Network Analysis of Genome-Wide Selective Constraint Reveals a Gene Network Active in Early Fetal Brain Intolerant of Mutation
RESEARCH ARTICLE Network Analysis of Genome-Wide Selective Constraint Reveals a Gene Network Active in Early Fetal Brain Intolerant of Mutation Jinmyung Choi1, Parisa Shooshtari1, Kaitlin E. Samocha2,3,4,5, Mark J. Daly2,3,4, Chris Cotsapas1,2,3,4,6* 1 Department of Neurology, Yale School of Medicine, New Haven Connecticut, United States of America, 2 Analytic and Translational Genetics Unit, Department of Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts, United States of America, 3 Program in Medical and Population Genetics, Broad Institute of Harvard and MIT, Cambridge, Massachusetts, United States of America, 4 Stanley Center for Psychiatric Research, Broad Institute of Harvard and MIT, Cambridge, Massachusetts, United States of America, 5 Program in Genetics and Genomics, Biological and Biomedical Sciences, Harvard Medical School, Boston, Massachusetts, United States of America, 6 Department of Genetics, Yale School of Medicine, New Haven CT, United States of America a11111 * [email protected] Abstract Using robust, integrated analysis of multiple genomic datasets, we show that genes de novo OPEN ACCESS depleted for non-synonymous mutations form a subnetwork of 72 members under strong selective constraint. We further show this subnetwork is preferentially expressed in Citation: Choi J, Shooshtari P, Samocha KE, Daly MJ, Cotsapas C (2016) Network Analysis of the early development of the human hippocampus and is enriched for genes mutated in Genome-Wide Selective Constraint Reveals a Gene neurological Mendelian disorders. We thus conclude that carefully orchestrated develop- Network Active in Early Fetal Brain Intolerant of mental processes are under strong constraint in early brain development, and perturbations Mutation. -

Dysregulation of Specialized Delay/Interference-Dependent Working Memory Following Loss of Dysbindin-1A in Schizophrenia-Related Phenotypes
Neuropsychopharmacology (2017) 42, 1349–1360 © 2017 American College of Neuropsychopharmacology. All rights reserved 0893-133X/17 www.neuropsychopharmacology.org Dysregulation of Specialized Delay/Interference-Dependent Working Memory Following Loss of Dysbindin-1A in Schizophrenia-Related Phenotypes 1,2 3,4 1 ’ 1,5 1,6 1 Emilie I Petit , Zuzanna Michalak , Rachel Cox , Colm MP O Tuathaigh , Niamh Clarke , Orna Tighe , 7 8 9,10 9 9,11 Konrad Talbot , Derek Blake , Josephine Joel , Alexander Shaw , Steven A Sheardown , 9,12 9,13 9 3 9 Alastair D Morrison , Stephen Wilson , Ellen M Shapland , David C Henshall , James N Kew , Brian P Kirby14 and John L Waddington*,1,15 1 2 Molecular and Cellular Therapeutics, Royal College of Surgeons in Ireland, Dublin, Ireland; Molecular Pharmacology, Albert Einstein College of 3 4 Medicine, Bronx, NY, USA; Department of Physiology and Medical Physics, Royal College of Surgeons in Ireland, Dublin, Ireland; Clinical and Experimental Epilepsy, University College London Institute of Neurology, London, UK; 5School of Medicine, University College Cork, Cork, Ireland; 6Office of Research and Innovation, Royal College of Surgeons in Ireland, Dublin, Ireland; 7Department of Neurology, University of California at 8 Los Angeles, Los Angeles, CA, USA; Institute of Psychological Medicine and Clinical Neurosciences, MRC Centre for Neuropsychiatric Genetics and 9 10 Genomics, Cardiff University, Cardiff, UK; Neurology Centre of Excellence for Drug Discovery, GlaxoSmithKline, Harlow, UK; Horizon Discovery, 11 12 13 Cambridge, -

Molecular Function of Rim1α: Role of Phosphorylation Sites
Molecular function of RIM1α: role of phosphorylation sites Dissertation zur Erlangung des Doktorgrades (Dr. rer. nat) der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Johannes Alexander Müller aus Bonn Bonn, Juli 2019 Angefertigt mit der Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn. 1. Gutachter: Prof. Dr. Susanne Schoch McGovern 2. Gutachter: Prof. Dr. Thorsten Lang Tag der Promotion: 09.10.2019 Erscheinungsjahr: 2020 Declaration: Parts of this thesis are already published in: Engholm-Keller K, Waardenberg AJ, Müller JA, Wark JR, Fernando RN, Arthur JW, Robinson PJ, Diet- rich D, Schoch S, Graham ME. The temporal profile of activity-dependent presynaptic phospho-signalling reveals long-lasting patterns of poststimulus regulation. PLoS Biology 2019; 17(3): e3000170 Marvin JS, Scholl B, Wilson DE, Podgorski K, Kazemipour A, Müller JA, Schoch S, Quiroz FJU, Rebola N, Bao H, Little JP, Tkachuuk AN, Cai E, Hantman AW, Wang SS, DePiero VJ, Borghuis BG, Chapman ER, Dietrich D, DiGregorio DA, Fitzpatrick D, Looger LL. Stability, affinity, and chromatic variants of the glutamate sensor iGluSnFR. Nature Methods 2018; 15(11): 936-939 For a full list of publications, book chapters and conference presentations (also including works, that are not part of this thesis) please refer to section 11 (Publications). Finally. Index i Index List of Abbreviations vi List of Figures viii List of Tables xi 1 Summary 1 2 Introduction 3 2.1 Synapses . 3 2.2 The presynaptic terminal - a highly specialized subcellular compartment . 4 2.3 Generation, fusion and recycling of synaptic vesicles . 5 2.4 Heterogeneity of presynaptic vesicle pools . -

BLOS2 Negatively Regulates Notch Signaling During Neural and Hematopoietic Stem And
1 BLOS2 negatively regulates Notch signaling during neural and hematopoietic stem and 2 progenitor cell development 3 4 Wenwen Zhou 1, 6 #, Qiuping He 2, 6 #, Chunxia Zhang 2, 6, Xin He 1, Zongbin Cui 3, 5 Feng Liu 2, 6 *, and Wei Li 1, 4, 5 * 6 7 1 State Key Laboratory of Molecular Developmental Biology, Institute of Genetics and 8 Developmental Biology, Chinese Academy of Sciences, Beijing 100101, China; 9 2 State Key Laboratory of Membrane Biology, Institute of Zoology, Chinese Academy of 10 Sciences, Beijing 100101, China 11 3 State Key Laboratory of Freshwater Ecology and Biotechnology, Institute of Hydrobiology, 12 Chinese Academy of Sciences, Wuhan 430072, China 13 4 Center for Medical Genetics, Beijing Children’s Hospital, Capital Medical University; 14 Beijing Pediatric Research Institute; MOE Key Laboratory of Major Diseases in Children, 15 Beijing 100045, China; 16 5 Center of Alzheimer's Disease, Beijing Institute for Brain Disorders, Beijing 100053, China; 17 6 University of Chinese Academy of Sciences, Beijing 100039, China. 18 19 # Co-first authors. 20 * Correspondence should be addressed to: 21 Wei Li, Ph.D., Beijing Children’s Hospital, Capital Medical University, 56 Nan-Li-Shi Road, 1 22 Xicheng District, Beijing 100045, China. Tel: +86-10-5961-6628; Fax: +86-5971-8699; 23 e-mail: [email protected]; 24 Feng Liu, Ph.D., State Key Laboratory of Membrane Biology, Institute of Zoology, Chinese 25 Academy of Sciences, Beijing 100101, China. Tel.: +86 (10) 64807307; Fax: +86 (10) 26 64807313; Email: [email protected]. 27 28 Running Title: BLOS2 negatively regulates Notch signaling 29 30 Key Words: BLOS2; Notch; stem and progenitor cell development; neurogenesis; 31 hematopoiesis; endo-lysosomal trafficking 32 33 The authors declare that no competing interests exist. -

Human BLOC1S2 / BLOS2 Protein (GST Tag)
Human BLOC1S2 / BLOS2 Protein (GST Tag) Catalog Number: 13916-H09E General Information SDS-PAGE: Gene Name Synonym: BLOS2; CEAP; CEAP11 Protein Construction: A DNA sequence encoding the human BLOC1S2 (Q6QNY1-2) (Met1- Arg99) was fused with the GST tag at the N-terminus. Source: Human Expression Host: E. coli QC Testing Purity: > 74 % as determined by SDS-PAGE Endotoxin: Protein Description Please contact us for more information. BLOC1S2, also known as BLOS2, belongs to the BLOC1S2 family. It is a Stability: component of BLOC-1 complex. The BLOC-1 complex is composed of BLOC1S1, BLOC1S2, BLOC1S3, DTNBP1, MUTED, PLDN, Samples are stable for up to twelve months from date of receipt at -70 ℃ CNO/cappuccino and SNAPIN. The BLOC-1 complex is required for normal biogenesis of lysosome-related organelles, such as platelet dense Predicted N terminal: Met granules and melanosomes. BLOC1S2 interacts directly with BLOC1S1, Molecular Mass: BLOC1S3, MUTED, CNO/cappuccino and SNAPIN. It may play a role in cell proliferation. It also plays a role in intracellular vesicle trafficking. The recombinant human BLOC1S2 /GST chimera consists of 333 amino Functionally, BLOC1S2 gene has been proposed to participate in acids and has a predicted molecular mass of 38.7 kDa. It migrates as an processes (melanosome organization, microtubule nucleation, platelet approximately 39 KDa band in SDS-PAGE under reducing conditions. dense granule organization, positive regulation of cell proliferation, positive regulation of transcription, regulation of apoptosis, positive regulation of Formulation: transcription from RNA polymerase II promoter). Lyophilized from sterile PBS, pH 7.4 References Normally 5 % - 8 % trehalose, mannitol and 0.01% Tween80 are added as 1.Sowa ME, et al. -

A BLOC-1 Mutation Screen Reveals That PLDN Is Mutated in Hermansky-Pudlak Syndrome Type 9
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector ARTICLE A BLOC-1 Mutation Screen Reveals that PLDN Is Mutated in Hermansky-Pudlak Syndrome Type 9 Andrew R. Cullinane,1,* James A. Curry,1 Carmelo Carmona-Rivera,1 C. Gail Summers,2 Carla Ciccone,1 Nicholas D. Cardillo,1 Heidi Dorward,1 Richard A. Hess,1 James G. White,3 David Adams,1,4 Marjan Huizing,1 and William A. Gahl1,4 Hermansky-Pudlak Syndrome (HPS) is an autosomal-recessive condition characterized by oculocutaneous albinism and a bleeding diath- esis due to absent platelet delta granules. HPS is a genetically heterogeneous disorder of intracellular vesicle biogenesis. We first screened all our patients with HPS-like symptoms for mutations in the genes responsible for HPS-1 through HPS-6 and found no functional muta- tions in 38 individuals. We then examined all eight genes encoding the biogenesis of lysosome-related organelles complex-1, or BLOC-1, proteins in these individuals. This identified a homozygous nonsense mutation in PLDN in a boy with characteristic features of HPS. PLDN is mutated in the HPS mouse model pallid and encodes the protein pallidin, which interacts with the early endosomal t-SNARE syntaxin-13. We could not detect any full-length pallidin in our patient’s cells despite normal mRNA expression of the mutant transcript. We could detect an alternative transcript that would skip the exon that harbored the mutation, but we demonstrate that if this transcript is translated into protein, although it correctly localizes to early endosomes, it does not interact with syntaxin-13. -

Hermansky-Pudlak Syndrome
Chapter 8 Hermansky-Pudlak Syndrome Naoki Oiso and Akira Kawada Additional information is available at the end of the chapter http://dx.doi.org/10.5772/53573 1. Introduction Oculocutaneous albinism is classified into non-syndromic oculocutaneous albinism (OCA) and syndromic OCA including Hermansky-Pudlak syndrome (HPS), Chediak-Higashi syndrome (CHS) and Griscelli syndrome (GS). Both non-syndromic and syndromic OCAs are autosomal recessive disorders. Human HPS is genetically divided into nine forms, HPS type 1 (HPS-1) to HPS-9. Human HPS can be sub-classified into four subgroups which are associated with protein complexes encoded by the causative genes. In this session, we summarize (1) the clinical features of HPS, (2) the mice and rat models of HPS, and (3) the molecular functions. 2. The clinical features of HPS In 1959, Hermansky and Pudklak described two cases of OCA associated with hemorrhagic diathesis.1 Currently, the condition is known as HPS. HPS is a rare heterogeneous autosomal recessive syndrome which is typically characterized by OCA, bleeding diathesis, and lysosomal ceroid storage resulting from defects of multiple cytoplasmic organelles: melanosomes, platelet dense core granules, and lysosomes.2 The storage of ceroid-like material in lysosomes induces restrictive lung disease, ulcerative colitis, kidney failure, and cardiomyopathy. Accumulation of mice models, identification of causative genes and functional analysis indicated that HPS could be sub-classified into four groups according to four protein complexes, biogenesis of lysosome-related organelles complex-3 (BLOC-3) (HPS-1 and HPS- 4), adaptor protein-3 (AP-3) (HPS-2), BLOC-2 (HPS-3, HPS-5 and HPS-6) and BLOC-1( HPS- 7, HPS-8 and HPS-9).3-5 Currently, more than 16 mice strains and more than 2 rat strains are known as models of human HPS (Table 1).