Health System Committee Public Agenda
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Milestones in NZ Sexual Health Compiled by Margaret Sparrow
MILESTONES IN NEW ZEALAND SEXUAL HEALTH by Dr Margaret Sparrow For The Australasian Sexual Health Conference Christchurch, New Zealand, June 2003 To celebrate The 25th Annual General Meeting of the New Zealand Venereological Society And The 25 years since the inaugural meeting of the Society in Wellington on 4 December 1978 And The 15th anniversary of the incorporation of the Australasian College of Sexual Health Physicians on 23 February 1988 TABLE OF CONTENTS Pg Acknowledgments 3 Foreword 4 Glossary of abbreviations 5 Chapter 1 Chronological Synopsis of World Events 7 Chapter 2 New Zealand: Milestones from 1914 to the Present 11 Chapter 3 Dr Bill Platts MBE (1909-2001) 25 Chapter 4 The New Zealand Venereological Society 28 Chapter 5 The Australasian College 45 Chapter 6 International Links 53 Chapter 7 Health Education and Health Promotion 57 Chapter 8 AIDS: Milestones Reflected in the Media 63 Postscript 69 References 70 2 ACKNOWLEDGMENTS Dr Ross Philpot has always been a role model in demonstrating through his own publications the importance of historical records. Dr Janet Say was as knowledgeable, helpful and encouraging as ever. I drew especially on her international experience to help with the chapter on our international links. Dr Heather Lyttle, now in Perth, greatly enhanced the chapter on Dr Bill Platts with her personal reminiscences. Dr Gordon Scrimgeour read the chapter on the NZVS and remembered some things I had forgotten. I am grateful to John Boyd who some years ago found a copy of “The Shadow over New Zealand” in a second hand bookstore in Wellington. Dr Craig Young kindly read the first three chapters and made useful suggestions. -

Do You Oppose Adding Fluoride (Hydrofluorosilicic Acid) to Our Water
Oppose Aware topical Aware other Who should Other comments? fluoridation? application? programmes? decide? Please note: Over Do you Are you Are you Do you If you would like to include comments 2000 candidates oppose aware that aware of think having we will publish them along with your were sent the adding promoters other fluoridated answer survey but a few fluoride now say the successful water were not if we (hydrofluoro primary public dental should be: could not get their silicic acid) benefit from health A personal address. Nearly to our fluoride is programmes choice 500 replied. Where water? topical rather such as Decided by candidates did not than CHILDSMILE DHBs; reply but we knew 289 say YES, systemic (i.e. in Scotland Central their position we Opposed to it needs to or NEXO Govt; local have entered it in Fluoridation: be applied to programme councils; or italics Support the surface in Denmark? Other FFNZ of the tooth rather than swallowed)? Ashburton District Council Marie Hibbert Yes Yes No A personal choice Stuart Wilson No No Yes Decided by I am in favour of adding fluoride to all DHBs drinking water Edward gates Yes No No A personal I believe the individual public should be choice able to decide whether to use fluoride, or not. Furthermore, the decline in qualified staff and corresponding appalling decline in services offered by many small district councils, would not see them in a position, to decide, the use of a chemical such as fluoride. Auckland Council Rochelle Gormly Yes No Yes Decided by local councils Saffron Toms Yes Yes No A personal choice Alezix HENETI No No No Other I pay a lot of money every week as I only drink PURE distilled water 4-6 litres EVERYDAY, 7X days of the week. -

Super City Debate Series Governance
SUPER CITY DEBATE SERIES GOVERNANCE The Wellington Branch’s of the NZPI and RMLA invite you to attend and take part in a debate about whether there should be or should not be a new Super City for the Wellington Region. The second in the three part series will focus on ‘governance’. The final session will be held at the beginning of April and will consider ‘economics and commerce’. The governance debate will be led by: Fran Wilde: Chair of Greater Wellington Regional Council Celia Wade-Brown: Mayor of Wellington City Doug Martin: Director, Martin Jenkins Associates Mike Reid: Local Government New Zealand The debate series is intended to stimulate discussions and to grow understanding of the issues that surround the concept of creating a super city. The NZPI have teamed up with the RMLA to help generate multi-disciplinary inputs into the debate. Date: Tuesday 27 March 2012 Theme: Super City debate series: Governance Venue: Chapman Tripp, Level 17, 10 Customhouse Quay Time: 5:45pm – 8:00pm (Doors open at 5.20pm) Cost: $10 members / $15 non-members1 Please register by 12:00pm on Monday 26 March at: [email protected] Event sponsors: See over for payment options 1 Non-members applies to those who are not members of the RMLA or NZPI Payment options (please let us know when you register how you will be paying and if you are a member of the NZPI or of the RMLA): Cheque made out to “NZPI Wellington Branch” and post to NZPI Wellington Branch 19 Boundary Road Kelburn Wellington 6012 Send invoice to email or postal address. -

A Poststructural Analysis of the Health and Wellbeing of Young Lesbian Identified Women in New Zealand
A Poststructural Analysis of the Health and Wellbeing of Young Lesbian Identified Women in New Zealand. Katie Palmer du Preez A thesis submitted to Auckland University of Technology in fulfilment of the requirements for the degree of Doctor of Philosophy (PhD). 2016 Faculty of Health and Environmental Sciences. School of Clinical Sciences. ABSTRACT New Zealand is regarded internationally as a forerunner in the recognition of gay rights. Despite the wide circulation of discourses of gay rights and equality, research shows that young women who identify as lesbian continue to be marginalised by society, which constrains their health and wellbeing. This study was an inquiry into the health and wellbeing of young lesbians in New Zealand, from a poststructural feminist perspective. It posed the research question: what are the discourses in play in relation to the health and wellbeing of young lesbian identified women in New Zealand? The methodology employed was a poststructural feminist discourse analysis, drawing on the philosopher Michel Foucault’s concepts of genealogy and the history of the present. Interviews with young lesbians were conducted in 2012 amid public debate around same- sex marriage. Historical data sources were the extant texts Broadsheet, a feminist periodical with strong health and wellbeing emphasis, and Hansard, a record of New Zealand parliamentary debate. Issues of these publications were selected from the early 1970s, during which the second wave feminist movement emerged, and the mid-1980s when the campaign for Homosexual Law Reform took place in New Zealand. The discourse analysis made visible the production of multiple ‘truths’ of young lesbian health and wellbeing. -
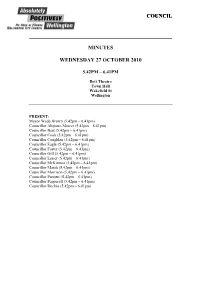
Minutes (112KB PDF)
COUNCIL MINUTES WEDNESDAY 27 OCTOBER 2010 5.42PM – 6.41PM Ilott Theatre Town Hall Wakefield St Wellington PRESENT: Mayor Wade-Brown (5.42pm – 6.41pm) Councillor Ahipene-Mercer (5.42pm – 6.41pm) Councillor Best (5.42pm – 6.41pm) Councillor Cook (5.42pm – 6.41pm) Councillor Coughlan (5.42pm – 6.41pm) Councillor Eagle (5.42pm – 6.41pm) Councillor Foster (5.42pm – 6.41pm) Councillor Gill (5.42pm – 6.41pm) Councillor Lester (5.42pm – 6.41pm) Councillor McKinnon (5.42pm – 6.41pm) Councillor Marsh (5.42pm – 6.41pm) Councillor Morrison (5.42pm – 6.41pm) Councillor Pannett (5.42pm – 6.41pm) Councillor Pepperell (5.42pm – 6.41pm) Councillor Ritchie (5.42pm – 6.41pm) 2 161/10C CHIEF EXECUTIVE’S WELCOME (1215/11/IM) NOTED: The Chief Executive Garry Poole opened the meeting and welcomed those present. 162/10C APOLOGIES (1215/11/IM) NOTED: There were no apologies. 163/10C DECLARATION OF THE MAYOR ELECT MADE PURSUANT TO CLAUSE 14 OF SCHEDULE 7 OF THE LOCAL GOVERNMENT ACT 2002 (1215/11/IM) 1. The Chief Executive Garry Poole called Mayor Elect Celia Wade- Brown forward to make her declaration. 2. The Mayor Elect made her declaration as follows: “Ko au a Celia Margaret Wade-Brown, Ko taku kupu tēnei. Ka tutuki i ahau, ki tāku e pono nei, ngā kawenga katoa hei painga mō te Tāone o Pōneke i runga i te mana kua riro mai i ahau, hei Kahika o Te Kaunihera o te Tāone o Pōneke, i raro i te Ture Kāwanatanga ā-Rohe 2002, te Ture Pārongo, Huinga Ōkawa ā-Kāwanatanga 1987, me ētahi atu ture rānei.” “I, Celia Margaret Wade-Brown, declare that I will faithfully and impartially, and according to the best of my skill and judgment, execute and perform, in the best interests of Wellington City, the powers, authorities, and duties vested in, or imposed upon, me as Mayor of the Wellington City Council by virtue of the Local Government Act 2002, the Local Government Official Information & Meetings Act 1987, or any other Act.” 3. -

Decolonisation and Free Association: The
DECOLONISATION AND FREE ASSOCIATION: THE RELATIONSHIPS OF THE COOK ISLANDS AND NIUE WITH NEW ZEALAND BY CAROLINE JENNY MCDONALD A thesis submitted to the Victoria University of Wellington in fulfilment of the requirements for the degree of Doctor of Philosophy Victoria University of Wellington 2018 ABSTRACT The Cook Islands and Niue are self-governing states in free association with New Zealand. The free association arrangements met United Nations decolonisation requirements. They reflected the needs and wishes of the Cook Islands and Niue, and the interests of New Zealand. Views are divided on what influenced the emergence of the arrangements for free association, whose interests they represented, and whether they have fulfilled the expectations of the Governments involved. The purpose of this thesis is to determine the formative influences shaping self- government in free association of these two states, and to reach a conclusion on how effective the free association arrangements have been in fulfilling initial expectations. The first half of this thesis draws on primary and secondary sources to establish what influenced the offer of self-determination, the options available, the choice made, the free association arrangements that emerged and whose interests these represented. The second half of this thesis turns to fulfilment of those expectations. It explores the flexibility of free association – the ability of the Cook Islands and Niue to make constitutional change. It examines each of the major elements of free association: holding New Zealand citizenship, New Zealand provision of necessary economic and administrative assistance and New Zealand responsibility for external affairs and defence. The conclusion is that the free association arrangements have been of mixed effectiveness in meeting the Governments’ initial expectations. -

Her Worship the Mayor: Women's Leadership in New Zealand Local
Copyright is owned by the Author of the thesis. Permission is given for a copy to be downloaded by an individual for the purpose of research and private study only. The thesis may not be reproduced elsewhere without the permission of the Author. HER WORSHIP THE MAYOR: Women's leadership ·in New Zealand local government A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy in Management Massey University, Palmerston North Aotearoa New Zealand Marianne Gaye Nicol Tremaine 2007 DEDICATION For my dear friend and colleague, Suzann Clair Olsson, whose passing came far too soon for everyone who loved her and benefited from her creative spirit and her ability to be open to the moment. ABSTRACT This study began with the premise that looking at leadership in a different setting might generate new understanding of how leadership works. Only four women mayors had held office in New Zealand before the 1980s but when their numbers grew over the next two decades, there were signs of a difference in their approach to leadership. Although the amount of scholarly work published on leadership is vast, the body of academic literature on local government leadership is slender. The possibility of finding new knowledge about leadership by studying women mayors made them an intriguing area to research. The research sought answers to two questions: - how do women mayors perceive exemplary mayoral leadership and explain their own leadership practice; and .. how do women mayors' views of leadership compare with leadership theory? The information gathered to assist in answering the research questions included: . -

The Workshop Was Hosted at the Museum of New Zealand
A RO A TE O A Aotearoa New Zealand THE WORKSHOP WAS HOSTED AT THE MUSEUM OF NEW ZEALAND TE PAPA TONGAREWA AND THE LEGISLATIVE COUNCIL CHAMBER, WELLINGTON, NEW ZEALAND Ten groups share their outputs from the March 2011 workshop: 1. A magazine cover that showcases success for New Zealand in the year 2058. 2. A coat of arms that illustrates what New Zealand should focus on going forward. 3. A strategy map that articulates a vision and outlines how that vision might be achieved. Groups at work Each of the ten groups preparing their strategy maps; navy blue, rust orange, purple, brown, teal, plum, yellow, red, avocado and emerald green (in clockwise order). 1 Introduction This booklet outlines the outputs of the Institute’s Output 1 two-day workshop, StrategyNZ: Mapping Our A cover design of the New Zealand Listener magazine Future, held on 30–31 March 2011. The workshop in 2058 to display where the vision would take us. started at the Museum of New Zealand Te Papa Output 2 Tongarewa and finished at the Legislative Council A redesigned New Zealand Coat of Arms to represent Chamber in Parliament, Wellington, New Zealand. the vision. See the front cover for the ten proposed This publication provides participants and other Coat of Arms and the back cover to learn more about interested parties with a resource that they can New Zealand’s current Coat of Arms. use to revisit the methods, ideas and strategies Output 3 generated at the workshop. A strategy map that shows the scope in which the country intends to operate. -

Hosts Report
Wellington, NZ 18-22 March 2019 Hosts Report 30 July 2019 Introduction In December 2016, three New Zealand community organisations were successful in their bid to host the International Lesbian, Gay, Bisexual, Trans and Intersex (ILGA) World Conference in Wellington, New Zealand. They were Intersex Trust Aotearoa New Zealand, Rainbow Youth and Tiwhanawhana Trust (the Host Rōpū). In bringing ILGA World to Wellington the Host Rōpū provided the opportunity for; Increased participation by New Zealand, Australian and Pa- cific LGBTIQ+ groups, in particular, indigenous and youth, at this international forum. ILGA World to experience, witness and learn from New Zea- land and Pacific experiences. The conference also celebrated important milestones; the 1st World Conference held in Oceania the 40th anniversary of ILGA World the 50th anniversary of the Stonewall Uprising (and along with it, the birth of the modern gay rights movement in the west). This report reflects what was achieved by the Host Rōpū, how it was done and why. Though brief, it provides a combined histori- cal, pictorial and financial overview. Included is a special section on the work achieved by the Host Rōpū to participants from the Pacific. It is hoped this report provides a useful overview for IL- GA members. The 2019 ILGA World Conference was a resounding success not- withstanding the tragedies in Christchurch. It was achieved be- cause of the generous support in kind, in sponsorship , in fund- ing and advice from many sectors of New Zealand society. All this from a journey that began in 2016. Wellington City, the Mayor of Wellington Justin Lester, the Cross Party NZ Parliamentary Rainbow Network through MP’s Jan Lo- gie, Louisa Wall and Chris Bishop, and the New Zealand Rain- bow community can justifiably be proud of the role they played in the success of this event. -

Labour Tops Poll
Vol 11 No 5 Wednesday May 6 1987 Serving Newtown, Te Aro, Mt Cook, Mt Victoria FREE Labour tops poll A poll conducted by Wellington Polytechnic journalism students in the Wellington electorates indicates that Labour will retain the seats of Wdlington Central and Island Bay. Island Bay secretary of the Clerical by Mary Wilson Workers Union. One in every three National: Sandra Clarke, consultant librarian. people in the Island Democrat: Paul Douche, Bay electorate so far retired company director. Wellington Polytechnic students joined their Victoria University colleagues in a seems undecided who march on Parliament to protest against moves by the Government to introduce to vote for in this Wellington the user pays principle into tertiary education. year's general Central election. by Andrea McKay Journalism students polled Labour's Fran Wilde 53 Island Bay electors in the should retain the Multi -culturalism attracts week before Easter as part of Wellington Central an overall poll of 500 voters seat at this year's in greater Wellington. general election, Forty-seven percent said parents to Mt Cook School they would vote Labour, 17 according to a recent b An N b emphasis on fa'a Samoa or and children alike would yards and a Polytech percent National while 34 telephone poll. .'Y ne . ew ery Taha Maori." overcome any physical extension block. pcr;;ent ,,i:re unllecided. Two The poll .x·.;d;.::td bj' White flight does Insn,ad, he said, newly disarlv~tagc the school has. " As the inner city is thirds of the undecided voters Wellington Polytechnic affect Mount Cook arrived families would look Despite these problems the redeveloped yuppies (young, said they voted Labour last journalism students in the School said Principal at alternative schools school role has increased, up upwardly mobile time. -

Draft PICT Paper
The Development of Learning Regions in New Zealand: an ICT perspective By Janet Mary Toland A thesis submitted to the Victoria University of Wellington in fulfilment of the requirements for the degree of Doctor of Philosophy in Information Systems Victoria University of Wellington 2010 ABSTRACT The term “Learning Region” is used to identify a region which is innovative, economically successful, and inhabited by citizens who are active members of their local community. Such regions are characterised by strong links between local businesses, community groups, and education providers. Within a regional area interaction and exchange of information is easier and cheaper than in a national or international context. The success of an individual organisation is directly related to the quality of information available locally. Information technology can be an important tool in improving the flow of knowledge between the stakeholders within a region. The study examines the role that information and communication technologies (ICTs) play in the development of learning regions in New Zealand, and how they can be used to improve the quality of information flows both within the region itself, and between the region and the outside world. In particular the research considers what contribution ICTs make to organisational learning and innovation. Historical methods are used to build up a picture of the significant changes that have taken place within two contrasting regions of New Zealand between 1985 and 2005. The two selected regions are Southland and Wellington. Data was collected by searching regional newspapers, and conducting interviews with key figures in each region. A “6- I”framework of the “ideal” features of a learning region was developed from the literature review and this was used to analyse the data. -

Clarence Beeby, the ‘Brains Behind the Blackboard’1
Clarence Beeby, the ‘Brains behind the Blackboard’1 ‘C E Beeby in an Indonesian classroom examining a student’s work’, 1973 Alexander Turnbull Library, Reference Number: PA1-0-877-13 1 Brown, Karen (1992) The brains behind the blackboard, in Evening Post, 13 Jun 1992, p.13 2 Beeby – The Brains behind the Blackboard: A Philosophical Biography ___________________________________________ A thesis submitted in partial fulfilment of the requirements for the Degree of DOCTOR OF PHILOSOPHY in PHILOSOPHY at the UNIVERSITY OF CANTERBURY ___________________________________________ by Michael Peter Couch ________________________________________ University of Canterbury August 2017 3 TABLE OF CONTENTS List of Appendices ............................................................................................................ 6 List of Graphs ................................................................................................................... 7 List of Tables ................................................................................................................... 8 Acknowledgments ........................................................................................................... 8 Abstract ............................................................................................................................ 9 Common Abbreviations ................................................................................................. 10 SECTION I STARTING UP: ‘A HAPPY KNACK OF BEING IN THE RIGHT PLACE AT THE RIGHT TIME’