124 Epochs of Anosmia and Ageusia in Multiple Sclerosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Second Edition
COVID-19 Evidence Update COVID-19 Update from SAHMRI, Health Translation SA and the Commission on Excellence and Innovation in Health Updated 4 May 2020 – 2nd Edition “What is the prevalence, positive predictive value, negative predictive value, sensitivity and specificity of anosmia in the diagnosis of COVID-19?” Executive Summary There is widespread reporting of a potential link between anosmia (loss of smell) and ageusia (loss of taste) and SARS-COV-2 infection, as an early sign and with sudden onset predominantly without nasal obstruction. There are calls for anosmia and ageusia to be recognised as symptoms for COVID-19. Since the 1st edition of this briefing (25 March 2020), there has been a significant expansion of literature on this topic, including 3 systematic reviews. Predictive value: The reported prevalence of anosmia/hyposmia and ageusia/hypogeusia in SARS-COV-2 positive patients are in the order of 36-68% and 33-71% respectively. There are reports of anosmia as the first symptom in some patients. Estimates from one study for hyposmia and hypogeusia: • Positive likelihood ratios: 4.5 and 5.8 • Sensitivity: 46% and 62% • Specificity: 90% and 89% The US Centres for Disease Control and Prevention (CDC) has added new loss or taste or smell to its list of recognised symptoms for SARS-COV-2 infection. To date, the World Health Organization has not. Conclusion: There is sufficient evidence to warrant adding loss of taste and smell to the list of symptoms for COVID-19 and promoting this information to the public. Context • Early detection of COVID-19 is key to the ongoing management of the pandemic. -

Taste and Smell Disorders in Clinical Neurology
TASTE AND SMELL DISORDERS IN CLINICAL NEUROLOGY OUTLINE A. Anatomy and Physiology of the Taste and Smell System B. Quantifying Chemosensory Disturbances C. Common Neurological and Medical Disorders causing Primary Smell Impairment with Secondary Loss of Food Flavors a. Post Traumatic Anosmia b. Medications (prescribed & over the counter) c. Alcohol Abuse d. Neurodegenerative Disorders e. Multiple Sclerosis f. Migraine g. Chronic Medical Disorders (liver and kidney disease, thyroid deficiency, Diabetes). D. Common Neurological and Medical Disorders Causing a Primary Taste disorder with usually Normal Olfactory Function. a. Medications (prescribed and over the counter), b. Toxins (smoking and Radiation Treatments) c. Chronic medical Disorders ( Liver and Kidney Disease, Hypothyroidism, GERD, Diabetes,) d. Neurological Disorders( Bell’s Palsy, Stroke, MS,) e. Intubation during an emergency or for general anesthesia. E. Abnormal Smells and Tastes (Dysosmia and Dysgeusia): Diagnosis and Treatment F. Morbidity of Smell and Taste Impairment. G. Treatment of Smell and Taste Impairment (Education, Counseling ,Changes in Food Preparation) H. Role of Smell Testing in the Diagnosis of Neurodegenerative Disorders 1 BACKGROUND Disorders of taste and smell play a very important role in many neurological conditions such as; head trauma, facial and trigeminal nerve impairment, and many neurodegenerative disorders such as Alzheimer’s, Parkinson Disorders, Lewy Body Disease and Frontal Temporal Dementia. Impaired smell and taste impairs quality of life such as loss of food enjoyment, weight loss or weight gain, decreased appetite and safety concerns such as inability to smell smoke, gas, spoiled food and one’s body odor. Dysosmia and Dysgeusia are very unpleasant disorders that often accompany smell and taste impairments. -

Unifying the Motor & Non-Motor Features of Parkinson's Disease
Unifying the Motor & Non-motor Features of Parkinson’s Disease Ali Shalash Professor of Neurology Chair of Ain Shams Movement Disorders Group Department of Neurology, Ain Shams Univeristy Cairo, Egypt AGENDA 1. Motor and non-motor Symptoms 2. Pathophysiology of Motor & NMS 3. Relation To Disease Course 4. NMS in motor subtypes 5. Motor & NMS fluctuation 6. Treatment of Motor & NMS: links Parkinson’s Disease • PD prevalence 1 % of populations older than 65 years (Abbas et al., 2018) • From 1990 to 2015, the number of with PD patients doubled to over 6 million, and double again to over 12 million by 2040 (Dorsey et al, 2018) • Aging populations, increasing longevity, decreasing smoking rates, and the by- products of industrialization MDS Clinical Diagnostic Criteria for PD Postuma et al 2015 MDS Clinical Diagnostic Criteria for PD Postuma et al 2015 Non-motor Symptoms of PD • Neuropsychiatric symptoms • Autonomic dysfunction • Depression up to 50-70 % • Drooling • Anxiety up to 60 % • Orthostatic hypotension 30–58% • Apathy 60 % • Urinary dysfunction • Psychosis up to 40% • Erectile dysfunction • Impulse control and related disorders • Gastrointestinal dysfunction 25–67% • Dementia, 24% to 40%. • Excessive sweating • Cognitive impairment 20-25% (other • Others than dementia mainly mild cognitive impairment) • Pain 30–85% • Fatigue 50% • Disorders of sleep and wakefulness • Olfactory dysfunction 90% • • Sleep fragmentation and insomnia Ophthalmologic dysfunction • Rapid eye movement sleep behavior disorder 65 % • Excessive daytime sleepiness Pathophysiology of Motor & NMS Neuropathology of PD: Motor Symptoms Two major pathologic processes: (a) premature selective loss of dopamine neurons: 30–70% cell loss ⇢ motor symptoms. (b) the accumulation of Lewy bodies, composed of α-synuclein Poewe, W. -

COVID-19 Psychosis: a Potential New Neuropsychiatric Condition Triggered by Novel Coronavirus Infection and the Inflammatory Response?
Journal Articles 2020 COVID-19 Psychosis: A Potential New Neuropsychiatric Condition Triggered by Novel Coronavirus Infection and the Inflammatory Response? S. J. Ferrando L. Klepacz Northwell Health, [email protected] S. Lynch M. Tavakkoli R. Dornbush See next page for additional authors Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Psychiatry Commons Recommended Citation Ferrando SJ, Klepacz L, Lynch S, Tavakkoli M, Dornbush R, Baharani R, Smolin Y, Bartell A. COVID-19 Psychosis: A Potential New Neuropsychiatric Condition Triggered by Novel Coronavirus Infection and the Inflammatory Response?. 2020 Jan 01; 61(5):Article 6623 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/6623. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. For more information, please contact [email protected]. Authors S. J. Ferrando, L. Klepacz, S. Lynch, M. Tavakkoli, R. Dornbush, R. Baharani, Y. Smolin, and A. Bartell This article is available at Donald and Barbara Zucker School of Medicine Academic Works: https://academicworks.medicine.hofstra.edu/articles/6623 Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre - including this research content - immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. -

Abadie's Sign Abadie's Sign Is the Absence Or Diminution of Pain Sensation When Exerting Deep Pressure on the Achilles Tendo
A.qxd 9/29/05 04:02 PM Page 1 A Abadie’s Sign Abadie’s sign is the absence or diminution of pain sensation when exerting deep pressure on the Achilles tendon by squeezing. This is a frequent finding in the tabes dorsalis variant of neurosyphilis (i.e., with dorsal column disease). Cross References Argyll Robertson pupil Abdominal Paradox - see PARADOXICAL BREATHING Abdominal Reflexes Both superficial and deep abdominal reflexes are described, of which the superficial (cutaneous) reflexes are the more commonly tested in clinical practice. A wooden stick or pin is used to scratch the abdomi- nal wall, from the flank to the midline, parallel to the line of the der- matomal strips, in upper (supraumbilical), middle (umbilical), and lower (infraumbilical) areas. The maneuver is best performed at the end of expiration when the abdominal muscles are relaxed, since the reflexes may be lost with muscle tensing; to avoid this, patients should lie supine with their arms by their sides. Superficial abdominal reflexes are lost in a number of circum- stances: normal old age obesity after abdominal surgery after multiple pregnancies in acute abdominal disorders (Rosenbach’s sign). However, absence of all superficial abdominal reflexes may be of localizing value for corticospinal pathway damage (upper motor neu- rone lesions) above T6. Lesions at or below T10 lead to selective loss of the lower reflexes with the upper and middle reflexes intact, in which case Beevor’s sign may also be present. All abdominal reflexes are preserved with lesions below T12. Abdominal reflexes are said to be lost early in multiple sclerosis, but late in motor neurone disease, an observation of possible clinical use, particularly when differentiating the primary lateral sclerosis vari- ant of motor neurone disease from multiple sclerosis. -

Clinical Diagnosis and Treatment of Olfactory Dysfunction
Clinical Diagnosis and Treatment of Olfactory Dysfunction Seok Hyun Cho Hanyang Med Rev 2014;34:107-115 http://dx.doi.org/10.7599/hmr.2014.34.3.107 Department of Otorhinolaryngology-Head and Neck Surgery, Hanyang University College of Medicine, Seoul, Korea pISSN 1738-429X eISSN 2234-4446 Olfactory dysfunction is a relatively common disorder that is often under-recognized by Correspondence to: Seok Hyun Cho Department of Otorhinolaryngology-Head both patients and clinicians. It occurs more frequently in older ages and men, and decreases and Neck Surgery, Hanyang University patients’ quality of life, as olfactory dysfunction may affect the emotion and memory func- Hospital, 222 Wangsimni-ro, Seongdong-gu, tions. Three main causes of olfactory dysfunction are sinonasal diseases, upper respiratory Seoul 133-792, Korea Tel: +82-2-2290-8583 viral infection, and head trauma. Olfactory dysfunction is classified quantitatively (hypos- Fax: +82-2-2293-3335 mia and anosmia) and qualitatively (parosmia and phantosmia). From a pathophysiologi- E-mail: [email protected] cal perspective, olfactory dysfunction is also classified by conductive or sensorineural types. All patients with olfactory dysfunction will need a complete history and physical examina- Received 17 April 2014 Revised 23 June 2014 tion to identify any possible or underlying causes and psychophysical olfactory tests are Accepted 3 July 2014 essential to estimate the residual olfactory function, which is the most important prognos- This is an Open Access article distributed under tic factor. CT or MRI may be adjunctively used in some indicated cases such as head trauma the terms of the Creative Commons Attribution and neurodegenerative disorders. -

Timeline and Outcome of Anosmia and Ageusia Associated with Covid-19 Infection: a Case Report
Crimson Publishers Case Report Wings to the Research Timeline and Outcome of Anosmia and Ageusia Associated with Covid-19 Infection: A Case Report Viviane Flumignan Z1*, Cristina Scavasine V1, Ghizoni Teive HA1, Branco Germiniani FM1, Azevedo VF2, Paulo Roberto Z3 and Camargo Rogenski CAM4 1Neurology division, Brazil ISSN: 2639-0531 2Rheumatology division, Brazil 3Occupational medicine division, Brazil 4Othorrinolaringology division, Brazil Abstract Background: Viral respiratory diseases can present with ageusia (hypogeusia) and anosmia (hyposmia) due to viral neurotropism, usually manifest together with other symptoms in the acute phase neurologicand have in manifestations most instances do both not aprovide good and information short recovery. about Duringneither the the epidemic timeline, periodnor the of outcome COVID-19, of thesedoctors symptoms should consider in this scenario. SARS-CoV-2 infection as a differential diagnosis. Recent series reporting these Patient’s concerns: *Corresponding author: onset of fever, followed by A dry54-year-old cough on female the second physician day, andwith on well-controlled the 4th day the diabetes, patient hypertensionnoticed a sudden and gnan Z, Department of vascular neurolo arrhythmia who presented with an acute respiratory syndrome with influenza symptoms, with sudden gy, Brazil Viviane Flumi- - and total loss of smell and taste sensations. After 20 days, she noticed a mild return of flavor perception, Submission: mainly for spicy foods, but still complained of hyposmia and dysgeusia until the end of this report (30 Diagnoses: Published: days after the onset of neuropathic symptoms). April 28, 2020 COVID 19 associated with anosmia and ageusia induced by viral respiratory disease May 12, 2020 inflammation.Intervention: Outcomes: HowVolume to 2 - Issuecite 4this article: cyanocobalamin supplementation to 9,000 micrograms per day. -

Both Anxiety and Joint Laxity Determine the Olfactory Features in Panic Disorder
Psychiatry Research xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Psychiatry Research journal homepage: www.elsevier.com/locate/psychres Both anxiety and joint laxity determine the olfactory features in panic disorder ⁎ Emma Buróna, , Antonio Bulbenaa,b, Andrea Bulbena-Cabréa,c, Sílvia Rosadob, Guillem Pailhezb a Autonomous University of Barcelona, Department of Psychiatry and Forensic Medicine (UAB), Bellaterra, Spain b Mar Health Park, Neuropsychiatry and Drug Addiction Institute (INAD), Barcelona, Spain c Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, USA ARTICLE INFO ABSTRACT Keywords: Previous research showed a high sensitivity in sensorial modalities in panic disorder (PD). This disorder has been Panic disorder consistently associated to the joint hypermobility syndrome (JHS). In non-clinical samples, this collagen al- Olfactory threshold teration has been also related to an enhanced sensitivity in some sensorial modalities. The main aim of this study Smell reactivity is to explore the olfactory functioning in PD in relation to JHS. Sixty patients with PD and sixty healthy controls Olfactory awareness performed the Sniffin’ Sticks Test (SST) (threshold subtest), and completed the Affective Impact of Odors scale Joint hypermobility syndrome (AIO), the Relational Scale of Olfaction (EROL), and the Odor Awareness Scale (OAS). Clinical symptom rating scales and JHS assessment were also obtained. PD patients showed enhanced odor acuity, greater reactivity to smells and also increased odor awareness compared to the healthy controls. Within the patients group, those suffering from JHS displayed higher functioning in all olfactory domains compared to the non-JHS ones. The JHS and anxiety measures emerged as predictor variables of the olfactory function. -

Neuropsychiatric Manifestations of COVID-19 Can Be Clustered in Three
www.nature.com/scientificreports OPEN Neuropsychiatric manifestations of COVID‑19 can be clustered in three distinct symptom categories Fatemeh Sadat Mirfazeli1,8, Atiye Sarabi‑Jamab2,8, Amin Jahanbakhshi3, Alireza Kordi4, Parisa Javadnia4, Seyed Vahid Shariat1, Oldooz Aloosh5, Mostafa Almasi‑Dooghaee6 & Seyed Hamid Reza Faiz7* Several studies have reported clinical manifestations of the new coronavirus disease. However, few studies have systematically evaluated the neuropsychiatric complications of COVID‑19. We reviewed the medical records of 201 patients with confrmed COVID‑19 (52 outpatients and 149 inpatients) that were treated in a large referral center in Tehran, Iran from March 2019 to May 2020. We used clustering approach to categorize clinical symptoms. One hundred and ffty‑one patients showed at least one neuropsychiatric symptom. Limb force reductions, headache followed by anosmia, hypogeusia were among the most common neuropsychiatric symptoms in COVID‑19 patients. Hierarchical clustering analysis showed that neuropsychiatric symptoms group together in three distinct groups: anosmia and hypogeusia; dizziness, headache, and limb force reduction; photophobia, mental state change, hallucination, vision and speech problem, seizure, stroke, and balance disturbance. Three non‑ neuropsychiatric cluster of symptoms included diarrhea and nausea; cough and dyspnea; and fever and weakness. Neuropsychiatric presentations are very prevalent and heterogeneous in patients with coronavirus 2 infection and these heterogeneous presentations may be originating from diferent underlying mechanisms. Anosmia and hypogeusia seem to be distinct from more general constitutional‑like and more specifc neuropsychiatric symptoms. Skeletal muscular manifestations might be a constitutional or a neuropsychiatric symptom. In December 2019 a number of severe acute respiratory syndrome (SARS) were reported in Wuhan, China that became eventually a pandemic infection with over 8 million reported cases until June 2020 1. -

Ageusia and Anosmia, a Common Sign of COVID-19? a Case Series from Four Countries
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 20 May 2020 doi:10.20944/preprints202005.0327.v1 Peer-reviewed version available at J. Neurovirol. 2020; doi:10.1007/s13365-020-00875-8 1 Ageusia and anosmia, a common sign of COVID-19? A case series from four countries Jair Vargas-Gandica,1,2 Daniel Winter,1 Rainer Schnippe,1 Andrea G. Rodriguez- Morales,2,3 Johana Mondragon,2 Juan Pablo Escalera-Antezana,2,4,5 María del Pilar Trelles-Thorne,6 D. Katterine Bonilla-Aldana,2,7,8 Alfonso J. Rodriguez-Morales,2,5,8,9,10,* Alberto Paniz-Mondolfi.2,6,10,11,12,13 1Klinik für Allgemeine Innere Medizin, Sankt Vinzenz Hospital, Rheda-Wiedenbrück, Germany. 2Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19), Pereira, Risaralda, Colombia. 3Unidad Procedimientos, Policlínico Neurología, Centro de Referencia de Salud Dr. Salvador Allende Gossens, Santiago de Chile, Chile. 4National Telehealth Program, Ministry of Health, La Paz, Bolivia. 5Universidad Privada Franz Tamayo/UNIFRANZ, Cochabamba, Bolivia. 6Icahn School of Medicine at Mount Sinai, New York, USA. 7Semillero de Zoonosis, Grupo de Investigación BIOECOS, Fundación Universitaria Autónoma de las Américas, Sede Pereira, Pereira, Risaralda, Colombia. 8Public Health and Infection Research Group, Faculty of Health Sciences, Universidad Tecnologica de Pereira, Pereira, Risaralda, Colombia. 9Grupo de Investigación Biomedicina, Faculty of Medicine, Fundación Universitaria Autónoma de las Américas, Pereira, Risaralda, Colombia. 10Committee on Travel Medicine, Pan-American Infectious Diseases Association, Asuncion, Paraguay. 11Laboratorio de Señalización Celular y Bioquímica de Parásitos, Instituto de Estudios Avanzados (IDEA), Caracas, Caracas, Venezuela. 12Academia Nacional de Medicina, Caracas, Venezuela. 13Instituto de Investigaciones Biomedicas IDB / Incubadora Venezolana de la Ciencia, Cabudare, Edo. -

Alteration, Reduction and Taste Loss: Main Causes and Potential Implications on Dietary Habits
nutrients Review Alteration, Reduction and Taste Loss: Main Causes and Potential Implications on Dietary Habits Davide Risso 1,* , Dennis Drayna 2 and Gabriella Morini 3 1 Ferrero Group, Soremartec Italia Srl, 12051 Alba, CN, Italy 2 National Institute on Deafness and Other Communication Disorders, NIH, Bethesda, MD 20892, USA; [email protected] 3 University of Gastronomic Sciences, Piazza Vittorio Emanuele 9, Bra, 12042 Pollenzo, CN, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0173-313214 Received: 3 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Abstract: Our sense of taste arises from the sensory information generated after compounds in the oral cavity and oropharynx activate taste receptor cells situated on taste buds. This produces the perception of sweet, bitter, salty, sour, or umami stimuli, depending on the chemical nature of the tastant. Taste impairments (dysgeusia) are alterations of this normal gustatory functioning that may result in complete taste losses (ageusia), partial reductions (hypogeusia), or over-acuteness of the sense of taste (hypergeusia). Taste impairments are not life-threatening conditions, but they can cause sufficient discomfort and lead to appetite loss and changes in eating habits, with possible effects on health. Determinants of such alterations are multiple and consist of both genetic and environmental factors, including aging, exposure to chemicals, drugs, trauma, high alcohol consumption, cigarette smoking, poor oral health, malnutrition, and viral upper respiratory infections including influenza. Disturbances or loss of smell, taste, and chemesthesis have also emerged as predominant neurological symptoms of infection by the recent Coronavirus disease 2019 (COVID-19), caused by Severe Acute Respiratory Syndrome Coronavirus strain 2 (SARS-CoV-2), as well as by previous both endemic and pandemic coronaviruses such as Middle East Respiratory Syndrome Coronavirus (MERS-CoV) and SARS-CoV. -
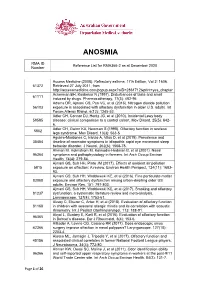
Reference List Concerning Anosmia
ANOSMIA RMA ID Reference List for RMA366-2 as at December 2020 Number Access Medicine (2008). Refractory asthma. 17th Edition, Vol 2: 1606. 61372 Retrieved 27 July 2011, from http://accessmedicine.com/popup.aspx?aID=2861712&print=yes_chapter Ackerman BH, Kasbekar N (1997). Disturbances of taste and smell 61111 induced by drugs. Pharmacotherapy, 17(3): 482-96. Adams DR, Ajmani GS, Pun VC, et al (2016). Nitrogen dioxide pollution 56103 exposure is associated with olfactory dysfunction in older U.S. adults. Int Forum Allergy Rhinol, 6(12): 1245-52. Adler CH, Connor DJ, Hentz JG, et al (2010). Incidental Lewy body 59585 disease: clinical comparison to a control cohort. Mov Disord, 25(5): 642- 6. Adler CH, Gwinn KA, Newman S (1998). Olfactory function in restless 5802 legs syndrome. Mov Disord, 13(3): 563-5. Aguirre-Mardones C, Iranzo A, Vilas D, et al (2015). Prevalence and 35454 timeline of nonmotor symptoms in idiopathic rapid eye movement sleep behavior disorder. J Neurol, 262(6): 1568-78. Ahman M, Holmstrom M, Kolmodin-Hedman B, et al (2001). Nasal 96364 symptoms and pathophysiology in farmers. Int Arch Occup Environ Health, 74(4): 279-84. Ajmani GS, Suh HH, Pinto JM (2017). Effects of ambient air pollution 5815 exposure on olfaction: A review. Environ Health Perspect, 124(11): 1683- 93. Ajmani GS, Suh HH, Wroblewski KE, et al (2016). Fine particulate matter 83088 exposure and olfactory dysfunction among urban-dwelling older US adults. Environ Res, 151: 797-803. Ajmani GS, Suh HH, Wroblewski KE, et al (2017). Smoking and olfactory 81237 dysfunction: a systematic literature review and meta-analysis.