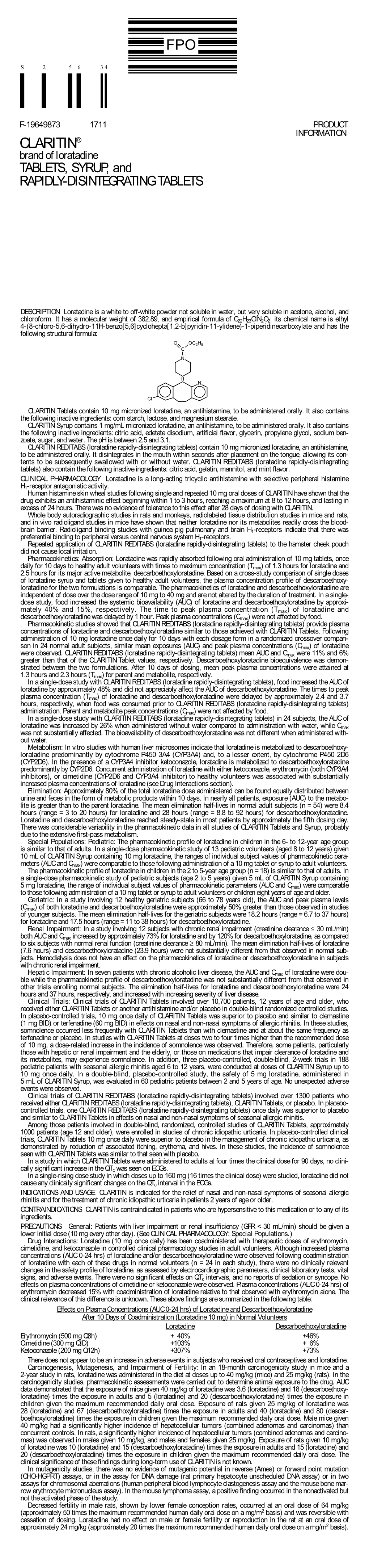
CLARITIN® Brand of Loratadine TABLETS, SYRUP, and RAPIDLY-DISINTEGRATING TABLETS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Male Anorgasmia: from “No” to “Go!”
Male Anorgasmia: From “No” to “Go!” Alexander W. Pastuszak, MD, PhD Assistant Professor Center for Reproductive Medicine Division of Male Reproductive Medicine and Surgery Scott Department of Urology Baylor College of Medicine Disclosures • Endo – speaker, consultant, advisor • Boston Scientific / AMS – consultant • Woven Health – founder, CMO Objectives • Understand what delayed ejaculation (DE) and anorgasmia are • Review the anatomy and physiology relevant to these conditions • Review what is known about the causes of DE and anorgasmia • Discuss management of DE and anorgasmia Definitions Delayed Ejaculation (DE) / Anorgasmia • The persistent or recurrent delay, difficulty, or absence of orgasm after sufficient sexual stimulation that causes personal distress Intravaginal Ejaculatory Latency Time (IELT) • Normal (median) à 5.4 minutes (0.55-44.1 minutes) • DE à mean IELT + 2 SD = 25 minutes • Incidence à 2-11% • Depends in part on definition used J Sex Med. 2005; 2: 492. Int J Impot Res. 2012; 24: 131. Ejaculation • Separate event from erection! • Thus, can occur in the ABSENCE of erection! Periurethral muscle Sensory input - glans (S2-4) contraction Emission Vas deferens contraction Sympathetic input (T12-L1) SV, prostate contraction Bladder neck contraction Expulsion Bulbocavernosus / Somatic input (S1-3) spongiosus contraction Projectile ejaculation J Sex Med. 2011; 8 (Suppl 4): 310. Neurochemistry Sexual Response Areas of the Brain • Pons • Nucleus paragigantocellularis Neurochemicals • Norepinephrine, serotonin: • Inhibit libido, -

Antihistamines in the Treatment of Chronic Urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 a Del Cuvillo,6 J Mullol,7 J Sastre,8 a Valero5
Antihistamines in the treatment of chronic urticaria I Jáuregui,1 M Ferrer,2 J Montoro,3 I Dávila,4 J Bartra,5 A del Cuvillo,6 J Mullol,7 J Sastre,8 A Valero5 1 Service of Allergy, Hospital de Basurto, Bilbao, Spain 2 Department of Allergology, Clínica Universitaria de Navarra, Pamplona, Spain 3 Allergy Unit, Hospital La Plana, Villarreal (Castellón), Spain 4 Service of Immunoallergy, Hospital Clínico, Salamanca, Spain 5 Allergy Unit, Service of Pneumology and Respiratory Allergy, Hospital Clínic (ICT), Barcelona, Spain 6 Clínica Dr. Lobatón, Cádiz, Spain 7 Rhinology Unit, ENT Service (ICEMEQ), Hospital Clínic, Barcelona, Spain 8 Service of Allergy, Fundación Jiménez Díaz, Madrid, Spain ■ Summary Chronic urticaria is highly prevalent in the general population, and while there are multiple treatments for the disorder, the results obtained are not completely satisfactory. The second-generation H1 antihistamines remain the symptomatic treatment option of choice. Depending on the different pharmacokinetics and H1 receptor affi nity of each drug substance, different concentrations in skin can be expected, together with different effi cacy in relation to the histamine-induced wheal inhibition test - though this does not necessarily have repercussions upon clinical response. The antiinfl ammatory properties of the H1 antihistamines could be of relevance in chronic urticaria, though it is not clear to what degree they infl uence the fi nal therapeutic result. Before moving on to another therapeutic level, the advisability of antihistamine dose escalation should be considered, involving increments even above those approved in the Summary of Product Characteristics. Physical urticaria, when manifesting isolatedly, tends to respond well to H1 antihistamines, with the exception of genuine solar urticaria and delayed pressure urticaria. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Thermodynamic Investigation of Promethazine, Loratadine, Cetirizine and Buclizine As Antihistamine Drugs; Monte Carlo and Semi-Empirical Studies
ISSN-E 1995-9516 Universidad Nacional de Ingeniería COPYRIGHT © (UNI). TODOS LOS DERECHOS RESERVADOS http://revistas.uni.edu.ni/index.php/Nexo https://doi.org/10.5377/nexo.v33i01.10050 Vol. 33, No. 01, pp. 94-108/Junio 2020 THERMODYNAMIC INVESTIGATION OF PROMETHAZINE, LORATADINE, CETIRIZINE AND BUCLIZINE AS ANTIHISTAMINE DRUGS; MONTE CARLO AND SEMI-EMPIRICAL STUDIES INVESTIGACIÓN TERMODINÁMICA DE PROMETAZINA, LORATADINA, CETIRIZINA Y BUCLIZINA COMO MEDICAMENTOS ANTIHISTAMÍNICOS; MONTE CARLO Y ESTUDIOS SEMI-EMPÍRICOS Mina Zakeri1, Majid Monajjemi2*, Ali Ebrahimi3 1Department of Chemistry, Science and Research Branch, Islamic Azad University, Tehran, Iran 2Department of Chemical Engineering, Central Tehran branch, Islamic Azad University Tehran, Iran 3Department of chemistry, Computational Quantum Chemistry Laboratory, University of Sistan and Baluchestan, Iran *[email protected] (recibido/received: 14-diciembre-2019; aceptado/accepted: 21-febrero-2020) ABSTRACT In this article, we discussed about four antihistamine drug called promethazine, loratadine, cetirizine and buclizine. Promethazine in this list is the only one in first generation antihistamine classification with CNS sedation effect and the other three belongs to second generation antihistamine group which are non- sedation and used to treat in many different anti-allergenic fields. In the following we optimized potential, kinetic and total energy of these molecules at body temperature (310 k˚) and environment temperature (298 k ˚) using Mont Carlo method in Amber force field in 500 ns. The quantum mechanics calculations and molecular structure of these molecules investigated using B3LYP level of theory with 6-31 G (d) as a basis set. Theoretical computations were performed to study thermodynamic parameters and frequency analysis. Electronic, thermal, zero point and gibs free energy and enthalpy were estimated in frequency analysis. -

Loratadine for Allergy Symptoms
information for parents and carers Loratadine for allergy symptoms This leaflet is about the use of loratadine to reduce the symptoms of allergy, such as in hay fever, urticaria (itchy rash) or pruritis (itchy skin) This leaflet has been written for parents and carers about how If you have bought your medicine over the counter, then to use this medicine in children. Our information sometimes please follow the instructions on the package carefully. If you differs from that provided by the manufacturers, because their are not sure how much to give, then contact your pharmacist information is usually aimed at adult patients. Please read or doctor. this leaflet carefully. Keep it somewhere safe so that you can It is important that you follow your doctor’s read it again. instructions or the instructions on the packaging about how much to give. Name of drug Loratadine How should I give it? Loratadine is available as many common brands, including: Tablets should be swallowed with a glass of Clarityn Allergy® or Clarityn Rapide Allergy®. water, milk or juice. Your child should not chew the tablet. Why is it important for my child to take this medicine? Liquid medicine: Measure out the right amount Loratadine is a medicine known as an antihistamine. When using an oral syringe or medicine spoon. You the body comes into contact with something it is allergic to, can get these from your pharmacist. Do not use such as pollen, animal hair or fur, house dust or insect bites, 5.0 ml 5.0 2.5 ml 2.5 a kitchen teaspoon as it will not give the right it produces a chemical called histamine. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

Loratadine and Pseudoephedrine | Memorial Sloan Kettering Cancer
PATIENT & CAREGIVER EDUCATION Loratadine and Pseudoephedrine This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Alavert Allergy and Sinus [OTC]; Allergy Relief-D [OTC]; Claritin-D 12 Hour Allergy & Congestion [OTC]; Claritin-D 24 Hour Allergy & Congestion [OTC]; Loratadine-D 12 Hour [OTC]; Loratadine-D 24 Hour [OTC] Brand Names: Canada Chlor-Tripolon ND; Claritin Extra; Claritin Liberator What is this drug used for? It is used to treat nose stuffiness. It is used to ease allergy signs. What do I need to tell my doctor BEFORE I take this drug? If you have an allergy to loratadine, pseudoephedrine, or any other part of this drug. If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you have taken certain drugs for depression or Parkinson’s disease in the last 14 days. This includes isocarboxazid, phenelzine, tranylcypromine, selegiline, or rasagiline. Very high blood pressure may happen. Loratadine and Pseudoephedrine 1/6 This is not a list of all drugs or health problems that interact with this drug. Tell your doctor and pharmacist about all of your drugs (prescription or OTC, natural products, vitamins) and health problems. You must check to make sure that it is safe for you to take this drug with all of your drugs and health problems. Do not start, stop, or change the dose of any drug without checking with your doctor. -

Medications to Avoid Before Skin Testing
PLEASE STOP ANTIHISTAMINES 5 DAYS PRIOR TO NEW PATIENT APPOINTMENTS OR ALLERGY SKIN TESTING *Do not stop asthma medications or any other medications that do not contain antihistamine! **If you have major hives or swelling, do not stop your antihistamines. ***Please call us if you have questions about any of your medications interfering with skin testing. ****Do not use oil, cream or lotion on the back or arms for 24 hours prior to skin testing. COMMON MEDICATIONS CONTAINING ANTIHISTAMINES • Actifed (chlorpheniramine) • Elavil (amitriptyline) • Advil PM, Advil Allergy • Excedrin PM • Alavert/Claritin (loratadine) • Fexofenadine (Allegra) • Allegra (fexofenadine) • Hydroxyzine (Atarax, Vistaril) • Alka Seltzer P.M. • Imipramine (Tofranil) • Amitriptyline (Elavil) • Levocetirizine (Xyzal) • Antivert (Meclizine) • Loratadine (Claritin) • Astelin Nasal Spray (azelastine) • Meclizine (Antivert, Bonine) • Astepro Nasal Spray (azelastine) • Norpramine (desipramine) • Atarax (hydroxyzine) • Nortriptyline (Pamelor) • Azelastine nose spray (Astepro, Astelin) • Nyquil • Benadryl (diphenhydramine) • Nytol • Bonine (meclizine) • Olopatadine (Patanase nasal spray) • Cetirizine (Zyrtec) • Pamelor (nortriptyline) • Chlorpheniramine (Chlor-Trimeton, Actifed, • Patanase Nasal Spray (olopatadine) Tussionex) • PBZ (pyribenzamine) • Chlor-Trimeton (chlorpheniramine) • Pediacare • Clarinex (desloratadine) • Periactin (Cyproheptadine) • Claritin (loratadine) • Phenergan (promethazine) • Clemastine (Tavist) • Promethazine (Phenergan) • Cogentin (for Parkinson's -

Top Prescription Drugs Older Adults Should Avoid Page 1 of 2
Top Prescription Drugs Older Adults Should Avoid page 1 of 2 Drug Problem Pain relievers amitriptyline (elavil) Amitriptyline can cause dry mouth, constipation, drowsiness, confusion and even hallucinations. indomethacin (indocin) Of all nonsteroidal anti-inflammatory drugs, indomethacin affects the brain the most. It can cause confusion or dizziness. narcotics Propoxyphene (Darvon) These are all opioids. Any opioid can cause constipation, urinary and combination products retention, drowsiness and confusion. However, those listed here that includes it (Darvocet-n) are particularly problematic. Propoxyphene, the main ingredient in Darvon and Darvocet, provides no more pain relief than acetaminophen. It may interfere with sleep and cause confusion. meperidine (Demerol) Meperidine lowers the seizure threshold in older adults, particularly those with renal insufficiency. It may be more likely to cause confusion than other narcotics. Pentazocine (talwin) Pentazocine is more likely to cause confusion and hallucinations than other opioids. antiDePressants Fluoxetine (Prozac) Fluoxetine’s effect lasts a long time. It may cause sleep taken daily disturbances, restlessness and increased agitation. It also may decrease appetite in some older adults who do not need to lose weight. If used, consider once weekly dosing. Doxepin (sinequan) Used to treat depression or sleep. These medications can amitriptyline (elavil) cause sedation, weakness, blood pressure changes, dry mouth, problems with urination, and can lead to falls and fractures. These are rarely the drugs of choice for older adults. clevelandclinic.org/geriatrics 10-GER-004 Top Prescription Drugs Older Adults Should Avoid page 2 of 2 Drug Problem sleeP anD anti-anxiety meDications benzodiazepines (long-acting): The effect of these medications last a long time (often days) Flurazepam (Dalmane) producing prolonged sedation and increasing the incidence of falls Diazepam (valium) and fractures. -

Validation of Cotinine As a Selective Probe Substrate, Inhibition by UGT Enzyme-Se
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2015/12/15/dmd.115.068213.DC1 1521-009X/44/3/378–388$25.00 http://dx.doi.org/10.1124/dmd.115.068213 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:378–388, March 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Human UDP-Glucuronosyltransferase (UGT) 2B10: Validation of Cotinine as a Selective Probe Substrate, Inhibition by UGT Enzyme-Selective Inhibitors and Antidepressant and Antipsychotic Drugs, and Structural Determinants of Enzyme Inhibition s Attarat Pattanawongsa, Pramod C. Nair, Andrew Rowland, and John O. Miners Department of Clinical Pharmacology (A.P., P.C.N., A.R., J.O.M.) and Flinders Centre for Innovation in Cancer (A.R., P.C.N., J.O.M.), Flinders University School of Medicine, Adelaide, Australia Received November 2, 2015; accepted December 14, 2015 ABSTRACT Downloaded from Although there is evidence for an important role of UGT2B10 in the antidepressant and antipsychotic drugs screened for effects on N-glucuronidation of drugs and other xenobiotics, the inhibitor UGT2B10 inhibited enzyme activity with IC50 values <100 mM. The selectivity of this enzyme is poorly understood. This study sought most potent inhibition was observed with the tricyclic antidepres- primarily to characterize the inhibition selectivity of UGT2B10 by sants amitriptyline and doxepin and the tetracyclic antidepressant UDP-glucuronosyltransferase (UGT) enzyme-selective inhibitors mianserin, and the structurally related compounds desloratadine dmd.aspetjournals.org used for reaction phenotyping, and 34 antidepressant and antipsy- and loratadine. Molecular modeling using a ligand-based approach chotic drugs that contain an amine functional group.