Trauma Treatment for Children in War : Build-Up of an Evidence-Based
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wikipedia, the Free Encyclopedia List of Commanders of the LTTE
4/29/2016 List of commanders of the LTTE Wikipedia, the free encyclopedia List of commanders of the LTTE From Wikipedia, the free encyclopedia The following is a list of commanders of theLiberation Tigers of Tamil Eelam (LTTE), also known as the Tamil Tigers, a separatist militant Tamil nationalist organisation, which operated in northern and eastern Sri Lanka from late 1970s to May 2009, until it was defeated by the Sri Lankan Military.[1][2] Date & Place Date & Place Nom de Guerre Real Name Position(s) Notes of Birth of Death Thambi (used only by Velupillai 26 November 1954 19 May Leader of the LTTE Prabhakaran was the supreme closest associates) and Prabhakaran † Velvettithurai 2009(aged 54)[3][4][5] leader of LTTE, which waged a Anna (elder brother) Vellamullivaikkal 25year violent secessionist campaign in Sri Lanka. His death in Nanthikadal lagoon,Vellamullivaikkal,Mullaitivu, brought an immediate end to the Sri Lankan Civil War. Pottu Amman alias Shanmugalingam 1962 18 May 2009 Leader of Tiger Pottu Amman was the secondin Papa Oscar alias Sivashankar † Nayanmarkaddu[6] (aged 47) Organization Security command of LTTE. His death was Sobhigemoorthyalias Kailan Vellamullivaikkal Intelligence Service initially disputed because the dead (TOSIS) and Black body was not found. But in Tigers October 2010,TADA court judge K. Dakshinamurthy dropped charges against Amman, on the Assassination of Rajiv Gandhi, accepting the CBI's report on his demise.[7][8] Selvarasa Shanmugam 6 April 1955 Leader of LTTE since As the chief arms procurer since Pathmanathan (POW) Kumaran Kankesanthurai the death of the origin of the organisation, alias Kumaran Tharmalingam Prabhakaran. -
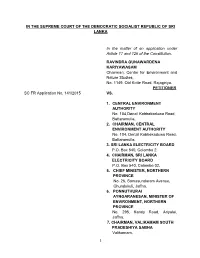
Documents in Support of Their Respective Positions
IN THE SUPREME COURT OF THE DEMOCRATIC SOCIALIST REPUBLIC OF SRI LANKA In the matter of an application under Article 17 and 126 of the Constitution. RAVINDRA GUNAWARDENA KARIYAWASAM Chairman, Centre for Environment and Nature Studies, No. 1149, Old Kotte Road, Rajagiriya. PETITIONER SC FR Application No. 141/2015 VS. 1. CENTRAL ENVIRONMENT AUTHORITY No. 104,Denzil Kobbekaduwa Road, Battaramulla. 2. CHAIRMAN, CENTRAL ENVIRONMENT AUTHORITY No. 104, Denzil Kobbekaduwa Road, Battaramulla. 3. SRI LANKA ELECTRICITY BOARD P.O. Box 540, Colombo 2. 4. CHAIRMAN, SRI LANKA ELECTRICITY BOARD P.O. Box 540, Colombo 02. 5. CHIEF MINISTER, NORTHERN PROVINCE No. 26, Somasundaram Avenue, Chundukuli, Jaffna. 6. PONNUTHURAI AYNGARANESAN, MINISTER OF ENVIRONMENT, NORTHERN PROVINCE No. 295, Kandy Road, Ariyalai, Jaffna. 7. CHAIRMAN, VALIKAMAM SOUTH PRADESHIYA SABHA Valikamam. 1 8. NORTHERN POWER COMPANY (PVT) LTD. No. 29, Castle Street, Colombo 10. 9. HON. ATTORNEY GENERAL Attorney General‟s Department, Colombo 12. 10. BOARD OF INVESTMENT OF SRI LANKA Level 26, West Tower, World Trade Center, Colombo 1. 11. NATIONAL WATER SUPPLY AND DRAINAGE BOARD P.O. Box 14, Galle Road, Mt. Lavinia. RESPONDENTS 1. DR. RAJALINGAM SIVASANGAR Chunnakam East, Chunnakam. 2. SINNATHURAI SIVAMAINTHAN Chunnakam East, Chunnakam. 3. SIVASAKTHIVEL SIVARATHEES Chunnakam East, Chunnakam. ADDED RESPONDENTS BEFORE: Priyantha Jayawardena, PC, J. Prasanna Jayawardena, PC, J. L.T.B. Dehideniya, J. COUNSEL: Nuwan Bopage with Chathura Weththasinghe for the Petitioner. Dr. Avanti Perera, SSC for the 1st to 4th, 9th, 10th and 11th Respondents. Dr. K.Kanag-Isvaran,PC with L.Jeyakumar instructed by M/S Sinnadurai Sundaralingam and Balendra for the 5th Respondent. Dinal Phillips,PC with Nalin Dissanayake and Pulasthi Hewamanne instructed by Ms. -

Integrated Strategic Environmental Assessment of the Northern Province of Sri Lanka Report
Integrated Strategic Environmental Assessment of the Northern Province of Sri Lanka A multi-agency approach coordinated by Central Environment Authority and Disaster Management Centre, Supported by United Nations Development Programme and United Nations Environment Programme Integrated Strategic Environmental Assessment of the Northern Province of Sri Lanka November 2014 A Multi-agency approach coordinated by the Central Environmental Authority (CEA) of the Ministry of Environment and Renewable Energy and Disaster Management Centre (DMC) of the Ministry of Disaster Management, supported by United Nations Development Programme (UNDP) and United Nations Environment Programme (UNEP) Integrated Strategic Environment Assessment of the Northern Province of Sri Lanka ISBN number: 978-955-9012-55-9 First edition: November 2014 © Editors: Dr. Ananda Mallawatantri Prof. Buddhi Marambe Dr. Connor Skehan Published by: Central Environment Authority 104, Parisara Piyasa, Battaramulla Sri Lanka Disaster Management Centre No 2, Vidya Mawatha, Colombo 7 Sri Lanka Related publication: Map Atlas: ISEA-North ii Message from the Hon. Minister of Environment and Renewable Energy Strategic Environmental Assessment (SEA) is a systematic decision support process, aiming to ensure that due consideration is given to environmental and other sustainability aspects during the development of plans, policies and programmes. SEA is widely used in many countries as an aid to strategic decision making. In May 2006, the Cabinet of Ministers approved a Cabinet of Memorandum -

Tides of Violence: Mapping the Sri Lankan Conflict from 1983 to 2009 About the Public Interest Advocacy Centre
Tides of violence: mapping the Sri Lankan conflict from 1983 to 2009 About the Public Interest Advocacy Centre The Public Interest Advocacy Centre (PIAC) is an independent, non-profit legal centre based in Sydney. Established in 1982, PIAC tackles barriers to justice and fairness experienced by people who are vulnerable or facing disadvantage. We ensure basic rights are enjoyed across the community through legal assistance and strategic litigation, public policy development, communication and training. 2nd edition May 2019 Contact: Public Interest Advocacy Centre Level 5, 175 Liverpool St Sydney NSW 2000 Website: www.piac.asn.au Public Interest Advocacy Centre @PIACnews The Public Interest Advocacy Centre office is located on the land of the Gadigal of the Eora Nation. TIDES OF VIOLENCE: MAPPING THE SRI LANKAN CONFLICT FROM 1983 TO 2009 03 EXECUTIVE SUMMARY ....................................................................................................................... 09 Background to CMAP .............................................................................................................................................09 Report overview .......................................................................................................................................................09 Key violation patterns in each time period ......................................................................................................09 24 July 1983 – 28 July 1987 .................................................................................................................................10 -

Transitional Justice for Women Ex-Combatants in Sri Lanka
Transitional Justice for Women Ex-Combatants in Sri Lanka Nirekha De Silva Transitional Justice for Women Ex-Combatants in Sri Lanka Copyright© WISCOMP Foundation for Universal Responsibility Of His Holiness The Dalai Lama, New Delhi, India, 2006. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher. Published by WISCOMP Foundation for Universal Responsibility Of His Holiness The Dalai Lama Core 4A, UGF, India Habitat Centre Lodhi Road, New Delhi 110 003, India This initiative was made possible by a grant from the Ford Foundation. The views expressed are those of the author. They do not necessarily reflect those of WISCOMP or the Foundation for Universal Responsibility of HH The Dalai Lama, nor are they endorsed by them. 2 Contents Acknowledgements 5 Preface 7 Introduction 9 Methodology 11 List of Abbreviations 13 Civil War in Sri Lanka 14 Army Women 20 LTTE Women 34 Peace and the process of Disarmament, Demobilization and Reintegration 45 Human Needs and Human Rights in Reintegration 55 Psychological Barriers in Reintegration 68 Social Adjustment to Civil Life 81 Available Mechanisms 87 Recommendations 96 Directory of Available Resources 100 • Counselling Centres 100 • Foreign Recruitment 102 • Local Recruitment 132 • Vocational Training 133 • Financial Resources 160 • Non-Government Organizations (NGO’s) 163 Bibliography 199 List of People Interviewed 204 3 4 Acknowledgements I am grateful to Dr. Meenakshi Gopinath and Sumona DasGupta of Women in Security, Conflict Management and Peace (WISCOMP), India, for offering the Scholar for Peace Fellowship in 2005. -

Jaffna District – 2007
BASIC POPULATION INFORMATION ON JAFFNA DISTRICT – 2007 Preliminary Report Based on Special Enumeration – 2007 Department of Census and Statistics June 2008 Foreword The Department of Census and Statistics (DCS), carried out a special enumeration in Eastern province and in Jaffna district in Northern province. The objective of this enumeration is to provide the necessary basic information needed to formulate development programmes and relief activities for the people. This preliminary publication for Jaffna district has been compiled from the reports obtained from the District based on summaries prepared by enumerators and supervisors. A final detailed publication will be disseminated after the computer processing of questionnaires. This preliminary release gives some basic information for Jaffna district, such as population by divisional secretary’s division, urban/rural population, sex, age (under 18 years and 18 years and over) and ethnicity. Data on displaced persons due to conflict or tsunami are also included. Some important information which is useful for regional level planning purposes are given by Grama Niladhari Divisions. This enumeration is based on the usual residents of households in the district. These figures should be regarded as provisional. I wish to express my sincere thanks to the staff of the department and all other government officials and others who worked with dedication and diligence for the successful completion of the enumeration. I am also grateful to the general public for extending their fullest co‐operation in this important undertaking. This publication has been prepared by Population Census Division of this Department. D.B.P. Suranjana Vidyaratne Director General of Census and Statistics 6th June 2008 Department of Census and Statistics, 15/12, Maitland Crescent, Colombo 7. -

Census Codes of Administrative Units Northern Province Sri Lanka Province District DS Division GN Division Name Code Name Code Name Code Name No
Census Codes of Administrative Units Northern Province Sri Lanka Province District DS Division GN Division Name Code Name Code Name Code Name No. Code Northern 4 Jaffna 1 Island North (Kayts) 03 Analaitivu North J/37 005 Northern 4 Jaffna 1 Island North (Kayts) 03 Analaitivu South J/38 010 Northern 4 Jaffna 1 Island North (Kayts) 03 Eluvaitivu J/39 015 Northern 4 Jaffna 1 Island North (Kayts) 03 Paruthiyadaippu J/50 020 Northern 4 Jaffna 1 Island North (Kayts) 03 Kayts J/49 025 Northern 4 Jaffna 1 Island North (Kayts) 03 Karampon J/51 030 Northern 4 Jaffna 1 Island North (Kayts) 03 Karampon East J/52 035 Northern 4 Jaffna 1 Island North (Kayts) 03 Naranthanai North West J/56 040 Northern 4 Jaffna 1 Island North (Kayts) 03 Naranthanai North J/55 045 Northern 4 Jaffna 1 Island North (Kayts) 03 Naranthanai J/57 050 Northern 4 Jaffna 1 Island North (Kayts) 03 Naranthanai South J/58 055 Northern 4 Jaffna 1 Island North (Kayts) 03 Karampon South East J/53 060 Northern 4 Jaffna 1 Island North (Kayts) 03 Karampon West J/54 065 Northern 4 Jaffna 1 Island North (Kayts) 03 Puliyankoodal J/60 070 Northern 4 Jaffna 1 Island North (Kayts) 03 Suruvil J/59 075 Northern 4 Jaffna 1 Karainagar 04 Karainagar North J/46 005 Northern 4 Jaffna 1 Karainagar 04 Karainagar North East J/47 010 Northern 4 Jaffna 1 Karainagar 04 Karainagar East J/42 015 Northern 4 Jaffna 1 Karainagar 04 Karainagar Centre J/48 020 Northern 4 Jaffna 1 Karainagar 04 Karainagar North West J/41 025 Northern 4 Jaffna 1 Karainagar 04 Karainagar West J/40 030 Northern 4 Jaffna 1 Karainagar -
International Human Rights Instruments and Several Optional Protocols
UNITED NATIONS HRI International Distr. Human Rights GENERAL Instruments HRI/CORE/LKA/2008 23 September 2008 Original: ENGLISH CORE DOCUMENT FORMING PART OF THE REPORTS OF STATES PARTIES SRI LANKA* [23 April 2008] * In accordance with the information transmitted to States parties regarding the processing of their reports, the present document was not edited before being sent to the United Nations translation services. GE.08-44221 (E) 221008 HRI/CORE/LKA/2008 page 2 CONTENTS Chapter Paragraphs Page I. GENERAL INFORMATION ABOUT THE STATE OF SRI LANKA ................................................................................... 1 - 110 3 A. History, geography, demography, economy, government, social infrastructure, post-tsunami reconstruction ...................... 1 - 59 3 B. Constitutional, political and legal structure of the State ............. 60 - 110 14 II. GENERAL FRAMEWORK FOR THE PROMOTION AND PROTECTION OF HUMAN RIGHTS ............................................... 111 - 220 23 A. Acceptance of international human rights norms ....................... 111 - 118 23 B. Legal framework for the protection of human rights at the national level ..................................................................... 119 - 134 26 C. Framework within which human rights are promoted at the national level ..................................................................... 135 29 D. Education programmes and public information .......................... 193 - 220 43 III. INFORMATION ON NON-DISCRIMINATION AND EQUALITY AND EFFECTIVE REMEDIES -

Sri Lankan Civil War
Sri Lankan Civil War The Sri Lankan Civil War was an armed conflict of the entire area previously controlled by the Tamil fought on the island of Sri Lanka. Beginning on 23 Tigers, including their de facto capital Kilinochchi, main July 1983, there was an intermittent insurgency against military base Mullaitivu and the entire A9 highway,[29] the government by the Liberation Tigers of Tamil Ee- leading the LTTE to finally admit defeat on 17 May lam (the LTTE, also known as the Tamil Tigers), an 2009.[30] Following the end of the war, the Sri Lankan independent militant organisation which fought to cre- government claimed Sri Lanka as the first country in the ate an independent Tamil state called Tamil Eelam in the modern world to eradicate terrorism on its own soil.[31] north and the east of the island. After a 26-year military Following the LTTE’s defeat, pro-LTTE Tamil National campaign, the Sri Lankan military defeated the Tamil Alliance dropped its demand for a separate state, in Tigers in May 2009, bringing the civil war to an end.[1] favour of a federal solution.[32][33] In May 2010, Mahinda For over 25 years, the war caused significant hardships Rajapaksa, the president of Sri Lanka, appointed the for the population, environment and the economy of the Lessons Learnt and Reconciliation Commission (LLRC) country, with an initial estimated 80,000–100,000 peo- to assess the conflict between the time of the cease- [18] fire agreement in 2002 and the defeat of the LTTE in ple killed during its course. -

Gold in Early Southeast Asia L’Or Dans Le Sud-Est Asiatique Ancien
ArcheoSciences Revue d'archéométrie 33 | 2009 Authentication and analysis of goldwork Gold in early Southeast Asia L’or dans le Sud-Est asiatique ancien Anna T. N. Bennett Electronic version URL: http://journals.openedition.org/archeosciences/2072 DOI: 10.4000/archeosciences.2072 ISBN: 978-2-7535-1598-7 ISSN: 2104-3728 Publisher Presses universitaires de Rennes Printed version Date of publication: 31 December 2009 Number of pages: 99-107 ISBN: 978-2-7535-1181-1 ISSN: 1960-1360 Electronic reference Anna T. N. Bennett, « Gold in early Southeast Asia », ArcheoSciences [Online], 33 | 2009, Online since 10 December 2012, connection on 10 December 2020. URL : http://journals.openedition.org/ archeosciences/2072 ; DOI : https://doi.org/10.4000/archeosciences.2072 Article L.111-1 du Code de la propriété intellectuelle. Gold in early Southeast Asia L’or dans le Sud-Est asiatique ancien Anna T. N. Bennett * Abstract: Gold is fairly widely, though irregularly, distributed throughout Southeast Asia in igneous and metamorphic hard rock deposits and in sedimentary placer deposits. he region was known to the Indian merchants of the 1st millennium BPE as Suvarnabhumi: ‘Land of Gold’, which is thought to refer to the mainland, including lower Burma and the hai Malay Peninsula, and Suvarnadvipa: ‘Islands of Gold’, which may correspond to the Indonesian Archipelago, including Sumatra. he historical sources inform us that the Chinese were clearly impressed by the quantities of gold present, and there is evidence to suggest that the gold deposits were one of the stimulating factors in the development of early contacts with India and China. Gold irst appears in the archaeological record in 400 BPE, at about the same time as iron, semiprecious stone polishing and glass working, suggesting that the techniques of gold extraction and working were quite plausibly introduced to Southeast Asia via Indian and/or Chinese merchants seeking gold ores. -
Newsletter-10-22-2020
Join us October 27th! We all know about the various Hindu traditions in India, but different forms of Hinduism are practiced in many places around the world, from Bhutan and Bali to Sri Lanka and Pakistan. In this week’s presentation, we will be exploring how Hinduism is practiced outside of India and the history of Hinduism in Asia, the Caribbean, and the West. We will also touch on the persecution of Hindus, including Hindu genocides and state-sponsored systemic violence, particularly against Hindus from historically oppressed castes. Here’s a quick document with informal notes and some preliminary resources if you’re interested: https://docs.google.com/document/d/1HKFPBXxXw-9Cy3FfKUKi87ttTd6ZuO9ck0Fb-Mfe3Yw/edit? usp=sharing Zoom link: https://tufts.zoom.us/j/96496822108 Password: hsc#2020 Weekly Showcase https://www.youtube.com/watch?v=h7kTQWNzKCY&list=PL9OwQaBQNytA87qCO1LvWjlelJKDl-yve&index=6 Sithara performs the Kuchipudi piece, Bhama Kalapam, which depicts the story of one of Krishna’s egotistical and envious wives, Satyabhama. She prides herself on her pure love for Krishna, but remains perpetually jealous of goddess Rukmini, another one of Krishna’s pious wives. This piece portrays the famous Parijata story, in which Krishna placates both his wives by planting a Parijatha tree in Satyabhama’s courtyard in such a way that its flowers would fall into Rukmini’s garden. Kuchipudi is one of the numerous styles of Indian Classical dance that originated from the state of Andhra Pradesh and is known for its unique style of elaborate footwork, dramatic characterization, and expressive narratives. Sithara performed this piece in September 2015 as part of her Arangetram - a traditional debut performance marking the completion of formal training in the art form - following 10 years under the tutelage of Smt. -

Tamil Militancy in Sri Lanka and the Role of Religion
Tamil Militancy in Sri Lanka and the Role of Religion Summary From the late 1970s to its defeat by the Government of Sri Lanka in 2009, the Liberation Tigers of Tamil Eelam (LTTE) fought for Tamil independence in Sri Lanka. The ultimate aim of what was often considered to be one of the world‘s most disciplined and efficient insurgency groups was to create an independent Tamil homeland (which they called Tamil Eelam) in the northern and eastern parts of the island. The LTTE based itself on a unique mix of Tamil nationalist, socialist, and feminist visions of a new future for the marginalized Tamil communities of Sri Lanka. The LTTE became feared for its extensive use of suicide missions, carried out by soldiers of both Hindu and Catholic backgrounds. Because of the marginalization of the Tamil-speaking Muslims from the Tamil nationalist project, none of the LTTE soldiers were Muslims. Generally speaking, religion played—and in the 21st century continues to play—a minor role in the ultimate nationalist goal of establishing Tamil Eelam. Tamil nationalism in Sri Lanka centers around Tamil culture, language, literature, and regional identity, not religion. The LTTE‘s official ideology was strictly secularist, expressing a clear separation between religion, the state, and politics. The LTTE accepted individual religious practices in its ranks—for example, having a personal crucifix or a holy picture within military camps, but did not facilitate institutionalized religious practice. Yet religious formations, controversies, and practices have been important, if not crucial, to Tamil separatism and, ultimately, to the LTTE itself. In a short period of time, the LTTE developed a unique martial culture and martyr cult, drawing on numerous cultural and religious sources in Tamil society.