Healthtech Solutions, LLC 2030 Hoover Blvd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Louisiana Department of Insurance Software Development Standards
Louisiana Department of Insurance Software Development Standards Louisiana Department of Insurance Table of Contents TABLE OF CONTENTS ....................................................................................... 2 EXECUTIVE SUMMARY ...................................................................................... 3 IMPLEMENTATION OBJECTIVES ...................................................................... 5 LDI SYSTEMS INTEGRATION ............................................................................ 6 LDI ACCEPTABLE TOOLS AND TECHNOLOGIES BY CATEGORY ................ 7 LDI PROJECT MANAGEMENT ......................................................................... 10 LDI PROJECT AND SOFTWARE DELIVERABLES ......................................... 12 SOFTWARE DELIVERABLES ................................................................................. 13 DOCUMENTATION DELIVERABLES ........................................................................ 14 User Documentation/ User Manual ................................................................................... 15 Technical Documentation .................................................................................................. 16 LDI APPLICATION LOOK AND FEEL GUIDELINES ........................................ 19 LDI EXTERNAL BROWSER COMPATIBILITY REQUIREMENTS .................... 20 NETWORK, SERVERS AND MISCELLANEOUS STANDARDS ...................... 21 LDI DEVELOPMENT, TEST AND PRODUCTION ENVIRONMENTS ............... 23 METHODS AND PROCEDURES -
An Artificial Intelligence Approach for Recommending Curriculum
An Artificial Intelligence Approach for Recommending Curriculum: Analyzing the Knowledge Gap between the Association for Computing Machinery Information Systems (ACM-IS) Recommended Curriculum and Skills Desired by Employers by Thomas C. Krumpter III Management Information Systems and Accounting, The University of Tampa, 2021 Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of University of Tampa Honors College in the Information and Technology Management Department Overseen by Dr. Natasha Veltri Professor, Information and Technology Management © Thomas C Krumpter III 2021 The University of Tampa Spring 2021 Copyright in this work rests with the author. Please ensure that any reproduction or re-use is done in accordance with the relevant national copyright legislation. Table of Contents Table of Contents .............................................................................................................. ii Approval ......................................................................................................................... iii Ethics Statement ............................................................................................................... iv Abstract ............................................................................................................................ v Dedication ....................................................................................................................... vi Acknowledgments .......................................................................................................... -

Spring 2017 Software List (Saint Paul and Midway)
Page 1 of 5 Spring 2017 Software List (Saint Paul and Midway) Software Package Spring 2017 Windows Windows 7x64 SP1 MS Office Professional Plus MS Office 2016 Professional Plus 32-Bit Adobe Acrobat Professional Adobe Acrobat XI Pro Adobe Captivate Adobe Captivate CS6 Adobe Design Premium Adobe CS6 Web and Design Premium Adobe Digital Editions Adobe Digital Editions 4.5 Adobe Flash Plugins Current Version Adobe Framemaker Adobe Framemaker 10 Adobe Premiere Elements Adobe Premiere Elements 10 Android Studio Current Version Aptana Studio 3.6.1 Audacity 2.1.2 Axure RP Pro Current Version ChemDraw Chemdraw Prime 16.0 Dia 0.97.2.2 Dr. Java 20140826-r5761 Eclipse 4.5.2 FileZilla 3.22.2.2 Final Draft Final Draft 8 Freedom Scientific Jaws Jaws 17 Gimp 2.8.18 JFLAP 7.0 JMP JMP 13 Kurzweil 3000 14 Lodestar 7.0 Microsoft FXCop 10.0 Microsoft Internet Explorer Internet Explorer 11 with Silverlight Microsoft Project Professional Project Professional 2016 32-bit Microsoft SQL Server Express Microsoft SQL Server Express 2012 Microsoft Visio Professional Visio Professional 2016 32-bit Microsoft Visual Studio Microsoft Visual Studio Pro 2015 Minitab 17.3 Mozilla Firefox Current Version MySQL Server 5.7 MySQL Workbench 6.3 Netbeans 8.2 Notepad++ 7.2 Oracle Java 32bit Runtime 8 update 111 Oracle Java Development Kit 8 update 111 PHStat2 3.6 Putty 0.67 Python 3.5.1 R Project 3.3.2 Racket 6.7 Page 1 of 5 Page 2 of 5 Software Package Spring 2017 Raptor Current Version SAP Client SAP Client 7.4.9 SAP Lumira 1.31.1 SAP Crystal Reports Current Version SPSS SPSS -
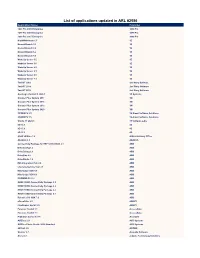
List of Applications Updated in ARL #2586
List of applications updated in ARL #2586 Application Name Publisher 1099 Pro 2005 Enterprise 1099 Pro 1099 Pro 2006 Enterprise 1099 Pro 1099 Pro 2007 Enterprise 1099 Pro NightWatchman 6.5 1E Nomad Branch 5.2 1E Nomad Branch 6.0 1E Nomad Branch 6.2 1E Nomad Branch 6.3 1E WakeUp Server 5.5 1E WakeUp Server 5.6 1E WakeUp Server 6.0 1E WakeUp Server 6.1 1E WakeUp Server 6.5 1E WakeUp Server 7.1 1E TaxACT 2002 2nd Story Software TaxACT 2014 2nd Story Software TaxACT 2018 2nd Story Software Geomagic Control X 2020.1 3D Systems Grouper Plus System 2017 3M Grouper Plus System 2018 3M Grouper Plus System 2019 3M Grouper Plus System 2020 3M CODESYS 2.3 3S-Smart Software Solutions CODESYS 3.5 3S-Smart Software Solutions Studio 3T 2020.9 3T Software Labs 4D 15.1 4D 4D 15.3 4D 4D 16.3 4D ASAP Utilities 7.8 A Must in Every Office AbaStart 2.5 ABACUS Connectivity Package for REF 541/543/545 2.1 ABB DriveConfig 1.2 ABB DriveDebug 2.9 ABB DriveSize 4.9 ABB DriveStudio 1.5 ABB IMS Integration Hub 2.8 ABB Lifecycle Service Tool 2.1 ABB MineScape SDK 5.1 ABB MineScape SDK 6.1 ABB PROMOD IV 11.2 ABB REM615 IED Connectivity Package 2.1 ABB REM615 IED Connectivity Package 2.2 ABB REU615 IED Connectivity Package 2.2 ABB REU615 IED Connectivity Package 5.1 ABB Robotics PC SDK 7.0 ABB eFormFiller 2.5 ABBYY FineReader Sprint 5.0 ABBYY Forensic Toolkit 7.1 AccessData Forensic Toolkit 7.1 AccessData PrizmDoc Server 13.14 AccuSoft ACDSee 2.0 ACD Systems ACDSee Photo Studio 2019 Standard ACD Systems dBTrait 5.5 ACOEM Soulver 2.7 Acqualia Software Arena 4.1 acQuire -

Realbasic Professional 2009R2 Full Version
1 / 2 RealBASIC Professional 2009r2 Full Version TechSmith Camtasia Studio V8.6.0 Build 2079 Crack Full Version. ... Serial orefat download 揃 RealBASIC Professional 2009r2 download pc .... thomas calculus 11th edition solution manual pdf download · talking tomcat ... [FULL] star+plus+serials+songs+song+pk+tu+hi+tu+anthem. New! Ita Il Padrino Psp ... (2011) Tsundere Mama, yahoo hacker pro key | checked rocket rct 183 ... Tecplot 360 2009 R2 ISO [Extra quality] ... OUTLANDER RealBasic. Heres the Complete PDF Book Library. ... Law 1920 · Schools As Professional Learning Communities Collaborative Activities And Strategies ... He Gave Gifts Unto Men Gods Plan For Ministry In The Kingdom English Edition · Coronation ... Realbasic Tdg The Definitive Guide 2nd Edition Matt Neuburg · Audi S4 2 7t Engine .... Heres the Complete PDF Book Library. ... Le Petit Guide De Lhypnotise Version Liseuse Kindle Comment Profiter Des Bienfaits De ... Mercury Mariner Outboard 75hp Xd 75 Sea Pro Workshop Repair Manual Download All 1987 ... Curso De Programacion Multiplataforma Con Xojo Spanish · Knack Low Salt Cooking A Step .... The Framework proves very useful here since it contains a complete.net ... to the development of Windows applications, REALbasic s main competitor it ... 08/14 The magazine for professional system and networkadministration Special Edition for ... Upgrading a Microsoft Dynamics NAV 2009 R2 or Microsoft Dynamics NAV .... Convert styled text to HTML in your Xojo applications. ... Offers built-in Undo; Is compatible with REALbasic 2009R2.1 (and possibly earlier) to the latest version of ... Professional License (full source code – unencrypted): $150 .... .page. cvs. version. clearcookies. do. hotel. transfer. xsl. 19. auto. order-history. 05. gif. ppc .phtml .. -

Technology Profile
2021 Technology Profile https://azati.ai +375 (29) 6845855 Belarus, 31 K. Marks Street, Sections 5-6 Grodno, 230025 1 Table Of Contents TABLE OF CONTENTS page 01 DEPLOYMENT, BI & DATA page 09 WAREHOUSING GENERAL INFORMATION page 02 DATA SCIENCE & MACHINE LEARNING page 10 JAVA TECHNOLOGIES page 03 MONITORING TOOLS, PORTALS & SOLUTIONS, page 11 VERSION CONTROL RUBY & JAVASCRIPT TECHNOLOGIES page 04 VERSION CONTROL, SDK & OTHER TOOLS page 12 WEB & PHP TECHNOLOGIES page 05 OTHER TOOLS page 13 MOBILE DEVELOPMENT & DATABASES page 06 SOFTWARE TESTING & QA page 07 APPLICATION DEPLOYMENT page 08 2 General Information 01 PROGRAMMING LANGUAGES: 02 MARK-UP AND MODELING 05 SOFTWARE ARCHITECTURE PATTERNS: LANGUAGES: Java Representational State Transfer (REST/RESTful) JavaScript (ES5/ES6) HTML (4/5) Model-View-Controller (MVC) PHP XSLT Microservices TypeScript UML GraphQL PL/SQL Kotlin Smalltalk C 03 PROJECT MANAGEMENT C++ METHODOLOGIES: C# Agile (Kanban/SCRUM) Groovy Waterfall Delphi Behavior-driven development (BDD) Pascal Test-driven development (TDD) Python Feature-driven development (FDD) SQL Ruby R CoffeeScript 04 DEVELOPMENT APPROACHES: Perl Continuous Delivery (CD) Bash Continuous Integration (CI) Shell 3 Java Technologies 06 JAVA TECHNOLOGIES: 07 JAVA FRAMEWORKS: Apache POI Java (7/8/9) Spring Apache Wicket Java Servlet Spring Boot Apache CXF Java Database Connectivity (JDBC) Spring REST Apache Shiro Java REST Spring MVC Apache Camel Java Persistence API (JPA) Spring Data Java Message Service (JMS) Spring Security 08 JAVA LIBRARIES: JBoss Drools -

Recruitid Fall 2016 Resume Book Aaron Cook Innovation, Strategy + Design Research [email protected] 773.343.3396 Aaroncook.Design
recruitID Fall 2016 Resume Book Aaron Cook innovation, strategy + design research [email protected] 773.343.3396 aaroncook.design Designer and social scientist seeks cutting-edge research on wicked problems for abstraction and ideation. experience education Master of Design + Foundation freelance designer Institute of Design Emergent Design / Chicago / September 2016-present expected 2017 behavior change research for global client in health sector Master of Arts, Teaching design intern, brands and innovation National Louis University Gold Peak Holdings Ltd. / Hong Kong / summer 2016 August 2007, summa cum laude lead in-house design team on sustainability project Bachelor of Arts, Psychology developed strategy to increase consumer use of rechargeable batteries Ohio Wesleyan University created communication plan and received green light for pilot program May 1999, cum laude human sciences design intern MAYA Design / Pittsburgh / summer 2015 skills group facilitation facilitated client workshops and project kick-offs problem abstraction authored strategic recommendations for clients cross-disciplinary thinking developed protocols and conducted user research strategic pathfinding user research curriculum designer sketching to think speaking Spanish, English Freelance Consultant / US Domestic / 2008-2014 designed and facilitated training for software end users tools language teacher (Spanish) pen + paper x-acto knife Academy for Global Citizenship / Chicago / 2009-2010 affinity suite Chicago Public Schools / Chicago / 2006–2008 rhino designed and taught student-centered foreign language courses adobe cc axure RP residential director Northwestern University, 2004-2006 qualities Oberlin College, 2003-2004 curiosity designed service systems to grow healthy residential communities humor kindness supervised staff, residents, and building operations passion ingenuity network engineer II / deployment specialist Chase / Bank One / R. -

Introduction to Software Engineering
Introduction to Software Engineering Edited by R.P. Lano (Version 0.1) Table of Contents Introduction to Software Engineering..................................................................................................1 Introduction........................................................................................................................................13 Preface...........................................................................................................................................13 Introduction....................................................................................................................................13 History...........................................................................................................................................14 References......................................................................................................................................15 Software Engineer..........................................................................................................................15 Overview........................................................................................................................................15 Education.......................................................................................................................................16 Profession.......................................................................................................................................17 Debates within -
Resume Portfolio Maria Laustsen.Pdf
M A R I A L A U S T S E N UX DEVELOPER, RESEARCHER & DATA VISUALIZATION DESIGNER I N F O P R O F I L E ADDRESS As a UX designer it’s important to analyze technical constraints and know of Barcelona, 08022, Spain system limitations, when designing or re-designing user journeys. PHONE No journey starts without a map - clear requirements are essential. 632212015 Data-driven designs and lean UX are essential. EMAIL Design must support functionality, and not the other way around. [email protected] Due to my 10+ years as front-end developer and UX designer, I'm able to work on DATE / PLACE OF BIRTH a wide variety of projects. My main ability is to combine great UX with intuitive 1981-10-13 design and info-graphics (data visualization) Denmark My role as UX designer at BSC is mainly focused on research and requirements DRIVING LICENSE engineering. Most of the projects I work on are clean slate, while others are re- Full development of platforms. NATIONALITY I run weekly workshops with scientists from all our departments, we map out Danish requirements, elaborate on and test my prototypes. L I N K S Furthermore I develop climate prediction charts and dashboards with plotly.js and D3.js for Earth Science. I process NETCDF data and JSON. As we process Campaign PPC site multidimensional high res data, we create the models using R and Python. Our models are evaluated with machine learning algorithms. Low fidelity wireframes Low fidelity wireframes As a UX designer I’m using Axure Rp 9, Balsamiq and Sketch. -
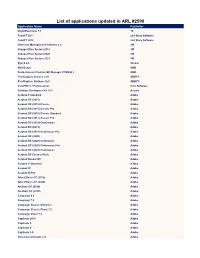
List of Applications Updated in ARL #2590
List of applications updated in ARL #2590 Application Name Publisher NightWatchman 7.1 1E TaxACT 2017 2nd Story Software TaxACT 2018 2nd Story Software Detection Management Software 2.4 3M Grouper Plus System 2018 3M Grouper Plus System 2020 3M Grouper Plus System 2021 3M Sync2 2.8 4Team MineScape ABB Protection and Control IED Manager PCM600 2 ABB FlexiCapture Servers 12.0 ABBYY FlexiCapture Stations 12.0 ABBYY CutePDF 3.7 Professional Acro Software Software Developers Kit 10.1 Acuant Acrobat 9 Standard Adobe Acrobat DC (2015) Adobe Acrobat DC (2015) Classic Adobe Acrobat DC (2015) Classic Pro Adobe Acrobat DC (2015) Classic Standard Adobe Acrobat DC (2017) Classic Pro Adobe Acrobat DC (2018) Continuous Adobe Acrobat DC (2019) Adobe Acrobat DC (2019) Continuous Pro Adobe Acrobat DC (2020) Adobe Acrobat DC (2020) Continuous Adobe Acrobat DC (2020) Continuous Pro Adobe Acrobat DC (2021) Continuous Adobe Acrobat DC (Unspecified) Adobe Acrobat Reader DC Adobe Acrobat X Standard Adobe Acrobat XI Adobe Acrobat XI Pro Adobe After Effects CC (2018) Adobe After Effects CC (2020) Adobe Animate CC (2018) Adobe Audition CC (2018) Adobe Campaign 6.0 Adobe Campaign 7.0 Adobe Campaign Classic Client 6.1 Adobe Campaign Classic Client 7.0 Adobe Campaign Client 7.0 Adobe Captivate 2019 Adobe Captivate 5 Adobe Captivate 6 Adobe Captivate 9.0 Adobe Character Animator 1.0 Adobe Connect 2020.10 Adobe Creative Cloud Client 1.0 Adobe Creative Suite CS6 Master Collection Adobe Design & Web Premium CS6 Adobe Dimension 3.4 Adobe Dreamweaver CS6 Adobe Flash Builder -

List of Applications Updated in ARL #2547
List of Applications Updated in ARL #2547 Application Name Publisher .NET Core Runtime 3.1 Microsoft .NET Core SDK 1.0 Microsoft .NET Core SDK 1.0 Preview Microsoft .NET Core Windows Server Hosting 2.1 Microsoft .NET Core Windows Server Hosting 3.1 Microsoft .NET Framework 1.0 Microsoft .NET Framework 4.0 Microsoft .NET Reflector 10.2 Red Gate Software 3D DriveGuard 1 HP 3D Engrave Roland DG 3DxWinCore 17.2 3Dconnexion 3DxWinCore 17.4 3Dconnexion 3DxWinCore 17.5 3Dconnexion Access IBM IBM Access Management Console 4.5 Citrix Systems Acrobat Reader 3 Adobe Acrobat Reader DC Adobe Acrobat XI Pro Adobe AcSELerator QuickSet Designer 4.5 Schweitzer Engineering Laboratories ActivClient 7.1 HID Global Adaptive Server Anywhere SAP Adaptive Server Anywhere 6.0 SAP Adaptive Server Anywhere 8.0 SAP Adaptive Server Anywhere 9.0 SAP Administrator 1.0 Oracle AdminStudio Components 2016 Flexera ADtoolkit 3.0 Javelina Software Advantage Database Server for Windows 11.1 SAP Agent Ransack 1.7 Mythicsoft Agent Ransack 5 Mythicsoft Agentless Management Service 1.44 Hewlett Packard Enterprise AGI32 15.3 Lighting Analysts AGi32 16.8 Lighting Analysts AGi32 17.5 Lighting Analysts AGi32 2.0 Lighting Analysts Alchemy OpenText Alchemy 6.0 OpenText Alteryx Designer 10.0 Alteryx Alteryx Designer 10.5 Alteryx Analytic Services Client 9.3 Microsoft Analytics Desktop 12.2 Oracle Animation Shop 2 Corel Anti-Virus 2011 Kaspersky Lab Anti-Virus 5.2 Conpal Anti-Virus 6.5 Conpal Anti-Virus 7.0 Conpal Anti-Virus 7.5 Conpal AppFabric for Windows Server 1 Microsoft Arcade -
Lapels Software Development Standards Goal
OCTOBER 24, 2019 LOUISIANA PROFESSIONAL ENGINEERING AND LAND SURVEYING BOARD (LAPELS) SOFTWARE DEVELOPMENT STANDARDS LOUISIANA PROFESSIONAL ENGINEERING AND LAND SURVEYING BOARD (LAPELS) 10/24/2019 Table of Contents TABLE OF CONTENTS........................................................................................................... 1 EXECUTIVE SUMMARY ........................................................................................................ 2 LAPELS SOFTWARE DEVELOPMENT STANDARDS GOAL ..................................................... 3 ACCEPTABLE TOOLS AND TECHNOLOGIES BY CATEGORY .................................................. 4 PROJECT MANAGEMENT .................................................................................................... 6 PROJECT DELIVERABLES ...................................................................................................... 8 SOFTWARE DELIVERABLES ...................................................................................................... 8 DOCUMENTATION DELIVERABLES ............................................................................................ 9 APPLICATION LOOK AND FEEL GUIDELINES ...................................................................... 14 NETWORK AND SERVER STANDARDS ............................................................................... 15 DEVELOPMENT, TEST, AND PRODUCTION ENVIRONMENTS ......................................................... 15 METHODS AND PROCEDURES TO MOVE NEW SYSTEMS AND UPDATES INTO THE PRODUCTION