2018 Annual Mcknight Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2020 Journal
2020 JOURNAL www.ntcumc.org 2 NORTH TEXAS CONFERENCE JOURNAL — 2020 TABLE OF CONTENTS PREFACE PHOTOGRAPHS OF BISHOP, CABINET, EXTENDED CABINET, ELDERS AND DEACON IN FULL CONNECTION, COMMISSIONED ELDERS AND DEACONS, AND RETIRING CLERGY ........................................................................................ 5-8 I. CONFERENCE HISTORY .......................................................................... 9 II. MINISTERS’ SERVICE RECORDS ......................................................... 10 III. APPOINTMENTS (Blue) .......................................................................... 42 IV. CONFERENCE PERSONNEL DIRECTORY (Password Protected)* V. CLERGY CHRONOLOGICAL ROLL .................................................... 143 VI. DIACONAL MINISTERS’ SERVICE RECORDS ................................. 149 VII. LAY MEMBERS OF ANNUAL CONFERENCE (Password Protected)* VIII. DAILY PROCEEDINGSDAILY PROCEEDINGS ................................. 176 2020 North Texas Annual Conference Photo Album .......................... 193 2020 AWARDS .................................................................................... 200 IX. LEGISLATIVE ACTIONS (Gray) ........................................................... 205 X. BUSINESS OF THE ANNUAL CONFERENCE .................................... 253 XI. STANDING RULES ................................................................................ 278 XII. ROSTER OF CONFERENCE AGENCIES (Green) ............................... 305 XIII. AGENCY REPORTS .............................................................................. -

The Spiritof Howard
WINTER 11 magazine SpiritThe f o Howard 001 C1 Cover.indd 1 2/15/11 2:34 PM Editor’s Letter Volume 19, Number 2 PRESIDENT Sidney A. Ribeau, Ph.D. EXECUTIVE DIRECTOR, COMMUNICATIONS AND MARKETING Thef Spirit o Howard Judi Moore Latta, Ph.D. EDITOR Raven Padgett Founders Library, named to the National Register of Historic Places in 2001, is such PUBLICATIONS SPECIALIST an iconic structure. While the clock tower that sits atop the library is one of the most LaShandra N. Gary recognizable physical symbols of Howard, the collection of history housed within CONTRIBUTING WRITERS the building may best represent the spirit of the University. Erin Evans, Sholnn Freeman, Damien T. The Moorland-Spingarn Research Center preserves centuries of African and Frierson, M.S.W., Fern Gillespie, African-American history. Snapshots of history archived in the center include docu- Kerry-Ann Hamilton, Ph.D., Ron Harris, ments, photographs and objects that help piece together an often fragmented story. Shayla Hart, Melanie Holmes, Otesa Middleton Miles, Andre Nicholson, Ashley FImagine reading firsthand the words of Olaudah Equiano, a former slave whose 1789 Travers, Grace I. Virtue, Ph.D. narrative is one of the earliest known examples of published writings by an African writer. Moorland-Spingarn holds at least one copy of the eight editions, including CONTRIBUTING PHOTOGRAPHERS a signed version. Other relics include 17th-century maps, 18th- and 19th-century Ceasar, Kerry-Ann Hamilton, Ph.D., masks, hundreds of periodicals and 30,000 bound volumes on the African Diaspora. Marvin T. Jones, Justin D. Knight This jewel on the yard is a unique structure that attracts scholars from all over the world, providing access to treasures that educate and enlighten. -
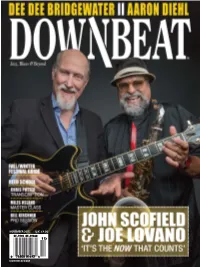
Downbeat.Com November 2015 U.K. £4.00
NOVEMBER 2015 2015 NOVEMBER U.K. £4.00 DOWNBEAT.COM DOWNBEAT JOHN SCOFIELD « DEE DEE BRIDGEWATER « AARON DIEHL « ERIK FRIEDLANDER « FALL/WINTER FESTIVAL GUIDE NOVEMBER 2015 NOVEMBER 2015 VOLUME 82 / NUMBER 11 President Kevin Maher Publisher Frank Alkyer Editor Bobby Reed Associate Editor Brian Zimmerman Contributing Editor Ed Enright Art Director LoriAnne Nelson Contributing Designer ĺDQHWDÎXQWRY£ Circulation Manager Kevin R. Maher Assistant to the Publisher Sue Mahal Bookkeeper Evelyn Oakes Bookkeeper Emeritus Margaret Stevens Editorial Assistant Stephen Hall Editorial Intern Baxter Barrowcliff ADVERTISING SALES Record Companies & Schools Jennifer Ruban-Gentile 630-941-2030 [email protected] Musical Instruments & East Coast Schools Ritche Deraney 201-445-6260 [email protected] Classified Advertising Sales Sam Horn 630-941-2030 [email protected] OFFICES 102 N. Haven Road, Elmhurst, IL 60126–2970 630-941-2030 / Fax: 630-941-3210 http://downbeat.com [email protected] CUSTOMER SERVICE 877-904-5299 / [email protected] CONTRIBUTORS Senior Contributors: Michael Bourne, Aaron Cohen, Howard Mandel, John McDonough Atlanta: Jon Ross; Austin: Kevin Whitehead; Boston: Fred Bouchard, Frank- John Hadley; Chicago: John Corbett, Alain Drouot, Michael Jackson, Peter Margasak, Bill Meyer, Mitch Myers, Paul Natkin, Howard Reich; Denver: Norman Provizer; Indiana: Mark Sheldon; Iowa: Will Smith; Los Angeles: Earl Gibson, Todd Jenkins, Kirk Silsbee, Chris Walker, Joe Woodard; Michigan: John Ephland; Minneapolis: Robin James; Nashville: Bob Doerschuk; -

26Th Rehoboth Beach Jazz Festival
Jz_001c.indd 1 10/1/15 3:56 PM IMPORTANT NOTE: Please review the proof thoroughly and submit all corrections together. Any requests after 2 revisions may incur additional design fees. Jz_002c.indd 1 10/1/15 4:12 PM October 2015 - Rehoboth Beach JAZZ FESTIVAL Page 3 After silence, that which comes closest to expressing the inexpressible is music. ~ ALDOUS HUXLEY ~ REHOBOTH MILLSBORO LEWES 246 Rehoboth Avenue 28442 DuPont Blvd. 1240 Kings Highway 227-3883 • 1-800-345-3469 934-3970 • 1-888-934-3970 645-2207 • 1-800-331-4241 JackLingo.com Page 4 October 2015 - Rehoboth Beach JAZZ FESTIVAL This program was created and published by the Cape Contents Gazette Special Sections Editor 8 Marc Antoine - Artist of Year Jen Ellingsworth Copy Editor Bob Yesbek 12 Jazz is special to Sam Calagione Page Design Deny Howeth 18 Van Williamson marks 25th fest Production Coordinator Norma Parks Advertising Sales Manager 20 Groove with BWB, Sax Pack Chris Rausch Advertising Representatives Cindy Bowlin 40 Al Jarreau shines Bettye LaVette will Kathy McGinty dazzle at a concert Amanda Neafie at 8:30 p.m. Andrew Thomas Saturday, Oct. 17. 53 Stanley Jordan is a must-see See page 64. Production Staff Kristin Sinnott Christopher D. Foster The Rehoboth Beach Jazz Festival is produced by the Delaware Celebration of Jazz. Dennis Santangini, president; Leon Galitzin, Edwin Krumm 58 Pieces of a Dream Come true vice president; Kas Naylor, head of hospitality; and Bing Crosby, Sherresha Powell webmaster. Cover artwork by Mike Massengale. Teresa Rodriguez Annual Christmas Joy! 365 * Silent Auction * Auction proceeds are used for Sat., Oct. -

REMEMBERING the MAN in the MIRROR By: David Walker Reactions from Fans Were Posted Across Little Michael on TV During the Jackson Ways Beyond Belief
ENTERTAINMENT 8 THE COMPASS - FALL 2009 REMEMBERING THE MAN IN THE MIRROR By: David Walker reactions from fans were posted across little Michael on TV during the Jackson ways beyond belief. Jackson contributed Michael Jackson, the King of Pop, their website. 5 era. Children can also be spotted with and gave back to the world more than the “Thriller fever”. was rushed to U.C.L.A. Medical Center Black Entertainment Television paid music; he gave back a spirit that will on June 25, 2009. Hours later the forever be remembered. The pop homage to the King of Pop and the With the fame and stardom comes the announcement of the world-renowned Jackson family during its annual Black price many must pay with it. culture has lost a pioneer but his lasting music icon death brought the world to affect on the world will last forever. Entertainment Television Award. Controversy surrounded Jackson a halt. Michael’s father, Joe Jackson, and throughout his lifetime. This included Jackson’s sudden death shocked his sister Janet Jackson were present at the the times of his father’s alleged millions of fans that Thursday. Often awards. Janet was the spokesperson for excessive abuse, demanding the best of imitated but always original, Jackson’s the entire family his children, and what some say was the style left a moon-walking footprints on The youngest of the Jackson worst that he did to his talented son, the music industry and society. daughters reminded the BET audience destroying his image of himself which Just before he could give the world that the Jackson family was hurting just most agree lead him to embark upon t'; another com eback the shocking 911 call like many o f them , and she thanked BET a number of plastic surgeries to create .• was dialed from the Jackson mansion. -

CHRISTOPHER STEVENS Trumpeter/Composer/Arranger
CHRISTOPHER STEVENS Trumpeter/Composer/Arranger (Founder/front man of Vertical Current & the co-owner of Signs Of Life Music LLC) ALBUMS (as a performer/horn arranger) • Tye Tribbett & Greater Anointing (GA): • Dave Patten- “On This Ledge” o “Life” • Kontraband 215- “My Time Is Now” o “Concepts and Ideas” • Michelle Bonilla- “Phenomenal” o “Victory” • J. Teddy Johnson- “Won’t Go Back” o “Standout” • Terrence Hundley- “Giving All Glory” • Tye Tribbett: • J.R.- “Life By Stereo” o “Fresh” • Alex Ingram & Friends- “His Mercy o “Greater Than” Endureth Forever” • Judith Christie-McAllister- “Sound The • Joe Leavell & St. Stephen Temple Choir- Trumpet” “God Is Able” • The Anointed Pace Sisters- “Access • Bethany Baptist Church (featuring Derrick Granted” Hodge)- “Bethany Live” • Earnest Pugh-“Earnest Pugh Live” • Ralph Moore: • Lowell Pye- “Finally” o “The Sound Of Christmas” • Virtue- “Testimony” o “A Call To Worship” • Amos Saint Jean- “Tell The World” • D-For: • Jeff Bradshaw– “Bone Appétit” o “The Gift” • Vivian Green– “Emotional Rollercoaster” o “Intersection” • Eric Roberson– “Left” • J S.O.U.L.- “Controversy” • Tess Henley- “Sneakers & High Heels” • Da Truth- “Open Book” • Mary J. Blige– “Best of my love” • Danielle Lewis- “Time 2 Praise” • Jean Baylor- “Light Up The World” • Lisa McClendon- “Christmas With You” • Jas Knight- “The Psalter” • Jason Nelson- “Shifting The Atmosphere” • World Harvest Church- “Catch The Fire” • Alex Holt- “Sing Loud” • Faith City- “A Very Special Christmas” • Eunice Wright- “Worth It All” • Jemi’Noel- “Jemi’Noel” -

PHONTE No News Is Good News RESTOCK COMING SOON CD NOW SHIPPING
PHONTE No News Is Good News RESTOCK COMING SOON CD NOW SHIPPING KEY SELLING POINTS • The sophomore solo album by Phonte (of Little Brother and The Foreign Exchange) • Features from Freddie Gibbs and Eric Roberson DESCRIPTION ARTIST: Phonte In 2011, when singer/rapper/songwriter Phonte of The Foreign Exchange TITLE: No News Is Good News (+FE) fame released the critically-acclaimed, Top 10 Rap/Hip Hop Album, CATALOG: L-FE012 Charity Starts at Home,it was an impactful reminder that Phonte was more than just the occasionally comical, often reflective crooner of +FE; LABEL: Foreign Exchange Music much more. As a rapper, Phonte had been the lynchpin of North Carolina’s GENRE: Hip-Hop/Rap globally respected four album, six mixtapes run of the now defunct Little BARCODE: 659123112017 Brother trio, whose “Lovin’ It” single from the 9th Wonder produced The FORMAT: 2XLP Minstrel Show is a bonafide cult classic. Audience members who came to know Phonte at the onset of The Foreign Exchange’s 2004 Connected HOME MARKET: North Carolina or over the last 14 years of near annual releases (whether outfit, duo, RELEASE: 8/31/2018 solo, live or remix) through Phonte and Nicolay’s Foreign Exchange LIST PRICE: $29.98 / CU Music label might have thought Phonte’s occasional bars throughout the years were the lighthearted play of a singer, not an extension of a strong CASE QTY: 35/1 Southern hip hop legacy several projects and nearly two decades deep. TRACKLISTING (Click Tracks In Blue To Preview Audio) Announced almost two years ago, No News Is Good News was in the incubator for some time, despite Phonte believing this project wouldn’t 1. -
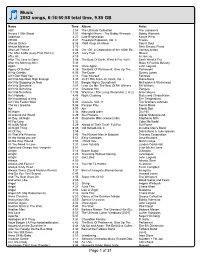
Tony's Itunes Library
Music 2053 songs, 6:16:50:58 total time, 9.85 GB Name Time Album Artist ABC 2:54 The Ultimate Collection The Jackson 5 Across 110th Street 3:51 Midnight Mover - The Bobby Womack ... Bobby Womack Addiction 4:27 Late Registration Kanye West AEIOU 8:41 Freestyle Explosion, Vol. 3 Freeze African Dance 6:08 1989 Keep On Movin' Soul II Soul African Mailman 3:10 Nina Simone Piano Afro Loft Theme 6:06 Om 100: A Celebration of the 100th Re... Various Artists The After 6 Mix (Juicy Fruit Part Ll) 3:25 Juicy Fruit Mtume After All 4:19 Al Jarreau After The Love Is Gone 3:58 The Best Of Earth, Wind & Fire Vol.II Earth Wind & Fire After the Morning After 5:33 Maze ft Frankie Beverly Again 5:02 Once Again John Legend Agony Of Defeet 4:28 The Best Of Parliament: Give Up The ... Parliament Ai No Corrida 6:26 The Dude Quincy Jones Ain't Gon' Beg You 4:14 Free Yourself Fantasia Ain't No Mountain High Enough 3:30 25 #1 Hits From 25 Years, Vol. I Diana Ross Ain't No Stopping Us Now 7:03 Boogie Nights Soundtrack McFadden & Whitehead Ain't No Sunshine 2:07 Lean On Me: The Best Of Bill Withers Bill Withers Ain't No Sunshine 3:44 Greatest Hits Dangelo Ain't No Sunshine 11:04 Wattstax - The Living Word (disc 2 of 2) Isaac Hayes Ain't Nobody 4:48 Night Clubbing Rufus and Chaka Kahn Ain't too proud to beg 2:32 The Temptations Ain't We Funkin' Now 5:36 Classics, Vol. -

The Nonce 1990
THE NONCE 1990 CD & CASSETTE BUMPED TO 5/11 KEY SELLING POINTS • Lost full-length album from the golden age of hip-hop • Previously unreleased material from 1990 • Legendary L.A. underground hip-hop duo, part of the Project Blowed collective • Audiophile quality mixing & mastering from the original multitrack sessions DESCRIPTION ARTIST: The Nonce The discovery and release of The Nonce 1990 is an important milestone TITLE: 1990 recorded during the Golden Age of Hip-Hop. Recognized as innovators CATALOG: L-FG-9000 of the LA Hip-Hop Underground, The Nonce was formed by two 17- year- LABEL: Family Groove Records olds; Nouka Basetype aka Sach and the late Yusef “Afloat” Mohammed. GENRE: Hip-Hop/Rap As The Nonce, the duo was part of the Project Blowed collective. BARCODE: 759478717148 FORMAT: 2XLP Just after high school graduation in 1990, the young duo was given the HOME MARKET: Los Angeles chance to go into a professional studio. Their dreams of a record deal RELEASE: 4/27/2018 were soon dashed after the production company raised objections to LIST PRICE: $24.98 / CT their artistic choices. Unwilling to meet the demands, The Nonce walked CASE QTY: 35 away from the project, leaving behind the masters of the very tracks that make up The Nonce 1990. TRACKLISTING (Click Tracks In Blue To Preview Audio) Daniel Borine, of the independent Family Groove label, discovered the 1. Chant This Hymn lost material for this album in 2017. Borine rescued the master tapes from 2. Stray Doves the studio where they were first recorded and subsequently misplaced, (but not forgotten), since 1990. -

Of Lil' John Roberts
Behind the Inside “The Heartbeat” of Lil’ John Roberts By Carlton Hargro Make no bones about it: The release of “The Heartbeat” — the brand- “I reached out to my crew of friends — the ones in the industry that beat new album by Lil’ John Roberts — is a really big deal. are my boys and girls. [For instance] reaching out to Musiq, that’s my little brother. I’ve been working with Musiq since 2000; I was And before you even have a chance to ask “why?” we’ll give you four his music director. So we’ve created a bond from so many years of reasons: 1.) “The Heartbeat” shines a spotlight on the jazz-meets- working together and being friends. Same thing with Stokely and Eric funk/soul/hip-hop+more style that Roberts — an acclaimed drummer, Roberson … we all know each other from way back. Anthony David: bandleader and one of the architects of Atlanta’s contemporary soul That’s the homie from when I moved to Atlanta. The relationships ‘ scene — has perfected over his decades-long career; 2.) the album that I’ve had through the years is what really prompted people to features heavyweight guest stars like Eric Roberson, Musiq Soulchild, get down with me and give back. Because a lot of them said: ‘John, Sa-Roc, James Poyser, Stokely Williams, Anthony David and more; 3.) you’ve done so much for all of us, we want to help you.’ And that’s a Mit’s actually his first-ever solo project; and 4.) it sounds damn good. -

GOAPELE Sat, Feb 10, 2018 | the Theatre at Ace Hotel East Side, West Side, All Around LA Welcome to the Center for the Art of Performance
CAP UCLA presents GOAPELE Sat, Feb 10, 2018 | The Theatre at Ace Hotel East Side, West Side, All Around LA Welcome to the Center for the Art of Performance The Center for the Art of Performance is not a place. It’s more of a state of mind that embraces experimentation, encourages a culture of the curious, champions disruptors and dreamers and supports the commitment and courage of artists. We promote Center for the Art of Performance presents rigor, craft and excellence in all facets of the performing arts. GOAPELE 2017–18 SEASON VENUES Royce Hall, UCLA Freud Playhouse, UCLA Sat, Feb 10 at 8pm | The Theatre at Ace Hotel The Theatre at Ace Hotel Little Theater, UCLA Running time: Approx. 90 mins. | No intermission Will Rogers State Historic Park Theo Rodrigues - Management / Creative Director UCLA’s Center for the Art of Performance (CAP UCLA) is dedicated to the advancement Ashley Raymond - Management of the contemporary performing arts in all disciplines—dance, music, spoken word Steven Baiocchi - Tour Manager and theater—as well as emerging digital, collaborative and cross-platforms utilized by Mike Aaberg - Musical Director today’s leading artists. Part of UCLA’s School of the Arts and Architecture, CAP UCLA Errol Cooney - Guitar curates and facilitates direct exposure to contemporary performance from around the James Richard - Bass globe, supporting artists who are creating extraordinary works of art and fostering a Corey Baugh - Drummer vibrant learning community both on and off the UCLA campus. The organization invests Toni Scruggs - Background Vocalist in the creative process by providing artists with financial backing and time to experiment DJ R-Tistic - DJ and expand their practices through strategic partnerships, residencies and collaborations. -
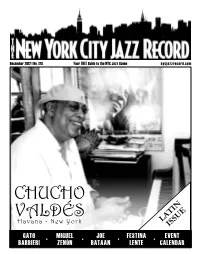
Latin Issue, We Would Like to Take 6 by Brad Farberman the Opportunity to Use the Term As a Starting Point for Discussion
December 2012 | No. 128 Your FREE Guide to the NYC Jazz Scene nycjazzrecord.com CHUCHO IN T E VALDÉS A U Havana - New York L S IS GATO • MIGUEL • JOE • FESTINA • EVENT BARBIERI ZENÓN BATAAN LENTE CALENDAR CASSANDRA WILSON GATO BARBIERI 11/29 - 12/2 12/3 & 4 DAVID SANBORN MEDESKI MARTIN & WOOD CHRIS BOTTI 12/5-9 W/ NELS CLINE (12/12), MARC RIBOT (12/13) ANNUAL RESIDENCY & BILL EVANS (12/14) 12/17 - 1/6 12/11-16 LATE NIGHT GROOVE SERIES: SUNDAY BRUNCH SERIES: THE Z THREE 12/1 SOPHISTAFUNK 12/15 NYU: BILLY DRUMMOND 12/2 SONUVO 12/7 RAY ANGRY 12/21 MARK GROSS & BLACKSIDE 12/9 THE FLOWDOWN 12/8 JEF LEE JOHNSON 12/22 AKIKO TSURUGA 12/16 INTERNATIONAL ORANGE 12/14 QUEEN AAMINAH 12/28 MARLENE VERPLANCK 12/23 SONY HOLLAND 12/30 TELECHARGE.COM TERMS, CONDITIONS AND RESTRICTIONS APPLY Much has been made about the term “jazz” throughout this music’s history; some find it to be an inclusive term, encompassing all stripes of styles and players while New York@Night others find it limiting, even demeaning. A topic not often discussed though is the 4 sub-genre “Latin jazz”. It is hard to believe that this term has existed as long as it Interview: Gato Barbieri has, trying ineffectually to cover dozens of cultures under its generic umbrella. For this The New York City Jazz Record’s first Latin issue, we would like to take 6 by Brad Farberman the opportunity to use the term as a starting point for discussion.