OJNA Journal Issue 6 Final.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Student Guide to Face Coverings
Student Guide to Face Coverings Face Coverings: A cloth or paper mask, scarf, bandana, gaiter or religious face covering that covers the mouth and nose. Whichever you choose, please ensure that there are two layers of fabric. If you are wearing a gaiter/ bandana with only one layer, please fold it over to create two layers. Gaiters/bandanas are not recommended. Face Shields: A clear face shield that extends below the chin in the front, to the ears on the sides and with no gap between the forehead and the headpiece may be used and only in certain specific circumstances. Face Covering Does Not Mean: Face Covering is Required: • Any mask or other item that includes a valve, hole, • Whenever I am indoors in all RPS buildings. gaps or openings to facilitate easier breathing, or is • On all RPS buses and vans. made of a mesh material. • Safety goggles that cover only the eyes or only the eyes and nose. • A face shield. Face Covering is Not Required: • When I am eating or drinking. • When I am outside. • When I am participating in indoor activities involving playing musical instruments (if the instrument cannot be played while wearing a face covering). • If I cannot tolerate a face covering due to a developmental, medical or behavioral health condition and a medical exemption has been approved for me. • If I have an IEP/504 and am receiving specialized instruction or service where wearing a face covering is problematic. • When I am participating in athletics competitions, I may temporarily remove my face covering during competitive game play. -
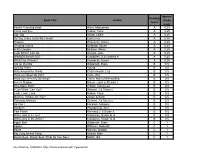
Book Title Author Reading Level Approx. Grade Level
Approx. Reading Book Title Author Grade Level Level Anno's Counting Book Anno, Mitsumasa A 0.25 Count and See Hoban, Tana A 0.25 Dig, Dig Wood, Leslie A 0.25 Do You Want To Be My Friend? Carle, Eric A 0.25 Flowers Hoenecke, Karen A 0.25 Growing Colors McMillan, Bruce A 0.25 In My Garden McLean, Moria A 0.25 Look What I Can Do Aruego, Jose A 0.25 What Do Insects Do? Canizares, S.& Chanko,P A 0.25 What Has Wheels? Hoenecke, Karen A 0.25 Cat on the Mat Wildsmith, Brain B 0.5 Getting There Young B 0.5 Hats Around the World Charlesworth, Liza B 0.5 Have you Seen My Cat? Carle, Eric B 0.5 Have you seen my Duckling? Tafuri, Nancy/Greenwillow B 0.5 Here's Skipper Salem, Llynn & Stewart,J B 0.5 How Many Fish? Cohen, Caron Lee B 0.5 I Can Write, Can You? Stewart, J & Salem,L B 0.5 Look, Look, Look Hoban, Tana B 0.5 Mommy, Where are You? Ziefert & Boon B 0.5 Runaway Monkey Stewart, J & Salem,L B 0.5 So Can I Facklam, Margery B 0.5 Sunburn Prokopchak, Ann B 0.5 Two Points Kennedy,J. & Eaton,A B 0.5 Who Lives in a Tree? Canizares, Susan et al B 0.5 Who Lives in the Arctic? Canizares, Susan et al B 0.5 Apple Bird Wildsmith, Brain C 1 Apples Williams, Deborah C 1 Bears Kalman, Bobbie C 1 Big Long Animal Song Artwell, Mike C 1 Brown Bear, Brown Bear What Do You See? Martin, Bill C 1 Found online, 7/20/2012, http://home.comcast.net/~ngiansante/ Approx. -

Students with Special Health Needs
Specialized Health Needs Interagency Collaboration COVID-19 PLANNING CONSIDERATIONS STUDENTS WITH SPECIAL HEALTH NEEDS Original 7/2020; Updated 8/13/2020, 2/15/2021 Preparing for staff and students to safely return to school during COVID-19 requires effective communication and planning. Children and youth with special health needs (CYSHN) may require additional considerations for the delivery of care in the educational setting related to their chronic condition, medical needs, or intellectual disability. Children with specialized healthcare needs comprise 25% of the student population and are at increased risk for COVID-19 complications (NASN, 2020). The purpose of this tool is to help the school nurse understand his/her role in supporting students with special health care needs and be a member of the school COVID-19 re-entry plan. 1. What is your school health staffing model? 2. What routine medications are administered? 3. What scheduled procedures occur in the health room? 4. How many students have an individualized healthcare plan and/or emergency care plan? 5. Where is your health room located? 6. Do you have an isolation area identified within your school or health room? 7. Have you considered a triage area for students entering health room? 8. How do teachers communicate with the school nurse about current student concerns during the day? 9. Are classrooms and teachers equipped to manage basic first-aid? 10. How does your local school system communicate and work with private duty nursing or aides in your school building? Review data on previous health room visits. Note scheduled medication(s), time, common PRN medication(s), and reasons for frequent sick visits. -

40Th Annual Service Auction
AIR STATION. • FAMILY FUN NIGHT. • HOMET INDS. • BICYCLE REP OWN SOCI E MAINTENA Y BL RE AR AR. • THERMAL AL T IBR N GE IMAGING CAMERA. • PICK (AKA . • IC L RK BL RANCE W PA PU A UNIFORMS. • BHS BAND RAI ENT HA Y W . • CITY HALL IT H Y UN . • Y STAINED GLASS WINDOW ALL, PL DA M OL LIBRAR RIBUTI L M PO . • BHS ORCKH. E• STR CONT ON). • A E Y). • PUBL CO T AR K RENOVATION (FINAL CIT QU BA N A Y P S PAR Y S E L O ES IT NOLD TRE & L T ID UN REY E FL CO UR L PROGRAMMM . • WITCH. • CONTINUING RENOV T S A U B S O IRS FER S ATION IG G R I • R C HA ANS OF N P T. C . TE ON L C TR SCO S. O • S K A ESCHOOL T O ND TIA • LE 4 A AR W R UR PO R A BICYCLE REPAIR S PAR R . T F P • D P B & TO LINDS. • TATION. K. EY • H E Y D. L . • RS RA RY B • FAM • R N SW O T IT N O G E E RA ILY E O F Y N U IN H N LIB S TEAM. • BER FU N L IM - U F AR T AC E IC ROBOTIC KLEY EDU N N OV D M J J MM P E E E Y G BL RINE CATIO IGH AT S I U A O I Y P BL C PU /SH N F T. -

Download DESIGN | MAKE | PROTECT
Authors The Community Impact Report is brought to you by Open Source Medical Supplies and Nation of Makers, with additional support and data from The Fab Foundation . Nation of Makers Nation of Makers supports the full range of organizations that impact makers by encouraging connections, broadly sharing resources, facilitating funding opportunities, engaging in policy development, and advocating for the maker movement. Open Source Medical Supplies Open Source Medical Supplies , a project of RESOLVE , informs and empowers makers, engineers, manufacturers, local organizers, experts, and institutions around the world working in their communities to meet medical supply challenges stemming from global crises. This report and the data it references were compiled, written, designed and edited by Gui Cavalcanti (OSMS); Claire Cocciole (NoM); Christina Cole (OSMS); Tobias Deml (OSMS); Katie Emerick (OSMS); Angela Forgues (OSMS); Victoria Jaqua (OSMS); Sophia Janowitz (OSMS); Dorothy Jones-Davis (NoM); Sabrina Merlo (OSMS); Kate Rowe (OSMS); Molly Wenig Rubenstein (OSMS). ©Copyright 2021 by Open Source Medical Supplies and Nation of Makers This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License . Please cite: Cavalcanti, Gui; Cocciole, Claire; Cole, Christina; Forgues, Angela; Jaqua, Victoria; Jones-Davis, Dorothy; Merlo, Sabrina (2021). “Design | Make | Protect: A report on the Open Source Maker and Manufacturer Response to the COVID-19 PPE Crisis.” Open Source Medical Supplies & Nation of Makers. DESIGN | MAKE | PROTECT 2 Acknowledgements We’d like to thank the following people and organizations, without whom this report would not have been possible. We would have had nothing to write without the willingness of individual responders to take the time to share their stories with us. -
Along the Path
TRAVEL / MEDITATION / BUDDHISM 2nd Edition The Meditator’s Companion to Pilgrimage in the Buddha’s India and Nepal Along the Path is a unique guidebook covering India and Nepal’s sacred sites; indispensable for the modern-day practitioner of the Buddha’s teachings. Along the Path: OFFERS a rich anthology of deeply inspiring stories relating to each of the pilgrimage sites connected to the Buddha’s life and teaching. PROVIDES detailed descriptions of each of the sites, including insider information on what to see and tips on transportation, accommodation and local cuisine. Kory Goldberg Goldberg Kory SUGGESTS excursions and activities in the vicinity of both ancient and modern sites. HIGHLIGHTS established Vipassana meditation centres that are best suited to accommodate visiting meditators. INCLUDES an in-depth travel section to help meditators prepare for a safe launch from home and cultivate & cultural sensibilities. Michelle Décary PRESENTS practical information with helpful maps, creative artwork and spirited narratives from experienced travellers. THE ESSENTIAL COMPANION FOR EVERY MEDITATOR VISITING INDIA AND NEPAL! Updates and resources: www.pilgrimage.pariyatti.org $21.95 US n o ti WWW.PARIYATTI.ORG Kory Goldberg & Michelle Décary di E d 2n This eBook is offered freely. If you wish, you may donate and help us continue offering our services. May you be happy! To make a donation, please visit: www.pariyatti.org PARIYATTI 867 Larmon Road Onalaska, Washington 98570 USA 360.978.4998 www.pariyatti.org Pariyatti is a nonprofit organization dedicated to enriching the world by: v Disseminating the words of the Buddha v Providing sustenance for the seeker’s journey v Illuminating the meditator’s path The Meditator's Companion to Pilgrimage in the Buddha s India and Nepal Kory Goldberg & Michelle Décary Pariyatti Press Kory Goldberg is a Humanities professor and Michelle Décary is a freelance writer, yoga teacher and organic gardener. -

Dealer Catalog.Indb
INDEX Symbols Coulter, 25 Wave 33 Coulter Blades 26–33 8 Wave Blades 34 Coulter Blades for Tool Bars 121 13 Wave Blades 31–32, 30–31 Coulter Hub Repair Parts 41, 23, 25, 35 25 Wave Blades 33 Coulter, Notched 32 Coulter, Ripple/Fluted 36 A Coulters, Plain Edge 34, 35 Acra Plant V-Shot Kit 117 Crary Air Reel Parts 191 Anhydrous Knives 122–123 Crary Gold n Cut Guards 187 Applicator Shanks 121 Crary Gold n Cut Hold Downs 189 Aprons, Manure Spreader 138–141 Crary Gold n Cut Sections 188 Arbor Bolts 24 Crary Gold n Cut Thunderbolt Sickles 190 Auger Finger 204, 206 Crustbuster Grain Drills 82, 84 Auger Liner 183 Culitivator Repair Parts 119–120 Augermate Power Unit 118 Cultivator/Soil Finisher Shank 12 Auger Straightener 180 D B Danish Sweeps 8–10 Baler Actuator 217 Danish Tine Shanks 11 Barn Scraper - UHMW 222 Disc Arbor Bolts 24 Battery Operated Grease Gun 226 Disc Blades 15–19, 16–20 Bean Windrower Teeth 216 Disc Spool 22 Bearing Flange Sets 128 DMI Side Dress Knife 123 Bearings 127–128 DMI Subsoiler Points 50, 51 Bearings for Cultivators 120 Double Cut II Repair Parts 197–198 Best Grain Drills 82 Double Cut II Sickle 198 Blades, Disc 16–22 Double Points for Field Cultivators 3 Blade, Soilsaver (fl at coulters) 42 Drag Chain Kit 87 Blades, Rotary Mower 132 Drill Parts 75–82 Blue Jet Subtiller 48 Dual Tillage Knives 121, 124, 125, 126 Bolt-on Tool for Sickles 211 Bolts 231–235 E Bulk Plow Bolts 233 Ear Savers 158 Bulk Poly Sheets 223 Easy Cut Sections 194 Elevator Chains 159–160 C Cast Iron Closing Wheels 105 F Chain, Elevator 159 Feather Sheets -

COVID Mask Effectiveness Webinar Questions and Answers
Tools & Resources Webinar: Effectiveness of Medical and Cloth Masks for COVID-19 Protection January 27, 2021 | Q&A Log 1. How can we assume any consistent perfect fitting by wearers of the masks? The majority of the testing was done on the same individuals to ensure consistency of facial characteristics. Each individual was assisted in fitting by an additional staff member. The team has done many hundreds of tests since March of 2020. 2. Are N95 masks effective and safe for wastewater workers regarding COVID-19 in wastewater? What about KN95 masks? Masks are given “N”, “R”, or “P” ratings based on their ability to repel oil https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/default.html Depending on what type of exposure is common for such workers, an elastomeric mask, typically worn in the construction and manufacturing may be more appropriate. These masks have a surface that can be cleaned and disinfected, with filter disks that are replaceable. Here is a link to a study of healthcare personnel and adapting these masks to their context with lower supply of traditional N95 masks available https://jamanetwork.com/journals/jama/fullarticle/2763841 KN95 or even procedure type (often called surgical) masks can offer protection, provided they fit well. Surgical masks that are FDA approved are frequently used in the healthcare field for their robustness to fluid exposure. However, although their inward filtration ability is adequate from a material standpoint, they are often lower values in real world testing due to loose/poor fit and gaps. These can be improved with a fit adjustment technique (“hack”, “fixthemask” brace, etc.). -

AW Face Covering Catalog 20021
FACE MASKS + ACCESSORIES FOR SCHOOLS CONTACT Al Vazquez [email protected] Visit us at ActiveWorldNYC.com O: 877.297.6583 / M: 917-862-2484 AW203-A012 Cotton 2 to 3 Layer Mask PRODUCT DESCRIPTION . 2 to 3 layer reusable face mask . Comfortable, washable, 100% Cotton . Full Fit or Flat Fit Full Fit Flat Fit . Ear Loops or Head Ties SIZING . Adult . Youth Ear Loops Head Ties COLORS . Black . White . Grey Heather . Navy - Binding can match or contrast mask color - Custom colors available Price, delivery and MOQ subject to change. Contact us for the most current information. CONTACT Al Vazquez [email protected] Visit us at ActiveWorldNYC.com O: 877.297.6583 / M: 917-862-2484 AW203-A019 Fully Sublimated 2 Layer Mask PRODUCT DESCRIPTION . 2 layer . Sublimated print premium athletic Polyester outer layer . Cotton inner layer with access for a filter insert Flat Fit . Breathable and comfortable, even during the summer . Black elastic only SIZING . One Size Ear Loops PricePrice, and delivery availablity and MOQ subject subject to changeto change. Contact us for themost most current current information information. CONTACT Al Vazquez [email protected] Visit us at ActiveWorldNYC.com O: 877.297.6583 / M: 917-862-2484 AW203-A013 Stretch Performance Gaiter PRODUCT DESCRIPTION . Solid, single layer, hemmed at top and bottom . 95% Polyester 5% Spandex . 9.5” wide (flat) x 19” high . Customization: heat transfer logo SIZING . One Size COLORS . Black . Charcoal . Deep Navy . Olive . Silver . True Royal . White Price, delivery and MOQ subject to change. Contact us for the most current information. CONTACT Al Vazquez [email protected] Visit us at ActiveWorldNYC.com O: 877.297.6583 / M: 917-862-2484 AW203-A014 Sublimated Tubular Headwear PRODUCT DESCRIPTION . -
The Magazine of the Reaud Honors College at Lamar University The
CADENZA TTHEHE MMAGAZINEAGAZINE OFOF TTHEHE RREAUDEAUD HHONOONORRSS CCOLLEGEOLLEGE AATT LLAAMMAARR UUNIVENIVERRSISITTYY ® VOL.VOL. 44 || SUMMERSUMMER 20202020 THANKMr. Reaud YOU The students of the Reaud Honors College would like to extend their gratitude to Mr. Wayne Reaud. Thanks to Mr. Reaud’s generosity, the Honors college has the support it needs to develop its future projects and plans. His donation has provided students with significant educational opportunities, enabling the Reaud Honors College to make an even greater impact on students’ lives. Thank you for helping to provide a quality education and college experience to hundreds of students every year. 100•60•10 LAMAR UNIVERSITY CENTENNIAL CELEBRATION Plans are under way to commemorate Lamar University’s 100th anniversary in 2023. The birthday celebration will be held during the 2023 calendar year from January to December. All colleges, departments, and organizations on campus are encouraged to participate in programming and projects. That year also marks the 60th anniversary of Honors education at the university (which makes it the oldest program in the Texas State University System) and the 10th anniversary of the establishment of the Reaud Honors College. Lamar University will celebrate with projects both on and off campus. Projects currently in progress include the Lamar 100 Project to collect Lamar memorabilia and a special Centennial book, a joint effort from the Center for History & Culture of Southeast Texas and the Upper Gulf Coast and Special Collections at the Mary and John Gray Library. The Reaud Honors College is currently developing plans to get in on the fun, so mark your calendars for that fall. -

Covid 19 Essentials Catalog (Pdf)
ASPIN-M-DM Disposable Face Masks Made of 3 layer non-woven polypropylene construction with an adjustable nose guard and elastic ear loops. These non-medical, non-sterile masks are intended for single-use only. Colors: White/Blue 100 500 1000 3000 5000 10000 0.69 0.69 0.60 0.60 0.60 0.60 Cotton Masks -Youth and Adult Sizes 3-layer face mask with two pleats. Its soft and comfortable, and made from 100% cotton fabric with antimicrobial finish and water resistant properties. Breathable material. Colors: White (Adult Only), Black 240 500 1000 5.25 5.15 4.60 SSPFM-003 Adult Protective Mask - USA Made Protect yourself and others with USA made face masks. Made from tight knit double-walled fabric. Washable & reusable. Covers your face, mouth and nose to reduce the spread of germs. 500 7.00 SSP-YPM Youth Protective Mask - USA Made This protective face mask is not to replace the N95 masks. It frees up the supply of the N95 masks for essential personnel that need them. 500 6.50 1 SSPWRAP-1FCDigital Multi Functional Seamless Wrap full color digital imprint - 2 Sides (100-499 qty) Polyester material with a full color digital imprint Approx 10" x 18.5" Multi-function head wrap is made of polyester microfiber fabric. 100 250 2.65 2.10 SSPWRAP-2 Sides Multi functional seamless rally wear - 2 Sided Imprint (500+ Qty) Multi-function head wrap is made of polyester microfiber fabric. Can be used as a bandana, beanie, wristband, headband, hair band, hair cover, head wrap, scrunchie, scarf, rally towel, face mask, sun Colors: Price includes 1 color, 2 sides, full wrap add .10 for each additional imprint color 500 1000 3000 5000 10000 1.50 1.25 1.10 0.95 0.90 TPG002 Face Mask Strap Hook & Earsaver Take the pressure off your ears! This Face Mask Strap Hook & Earsaver is ideal for helping give ears a rest from prolonged elastic band wear. -

Face Mask and Face Shield Manufacturing Directory
Face Mask and Face Shield Manufacturing Directory January 2021 Face Mask and Face Shield Manufacturing Directory To help meet increased demand for medical equipment and PPE due to the COVID-19 pandemic, the Victorian Government has worked with local industry to prepare a series of directories. This directory identifies local companies that manufacture masks or provide input materials such as fabrics. The directory includes four sections: 1. Reusable fabric mask suppliers 2. Surgical & respirator mask suppliers 3. Fabric suppliers 4. Face Shields Ethical Clothing Australia The directory states where a company is Ethical Clothing Australia accredited. Ethical Clothing Australia’s accreditation is focused on ensuring that local textile, clothing and footwear workers are being paid appropriately, receiving all the legal minimum entitlements and working in safe workplaces throughout the entire supply chain. The supply chain audit covers design, pattern making, cut, make, trim and dispatch, and all value adding services. In line with our policy, Victorian Government purchases of Uniforms and PPE can only be made from businesses that are ECA accredited. Disclaimer Whereas every effort has been made to verify the details in this directory, the Victorian Government accepts no responsibility to guarantee the delivery of products or services by the organisations listed in the directory nor does inclusion in the directory guarantee the placement of orders or contracts. It remains beholden on any user of the directory to conduct normal commercial due diligence. It is recommended that the TGA website is used to check current TGAregistration. For inclusion in future editions of this directory please contact [email protected].