Unscheduled Vaginal Bleeding with Progestin-Only Contraceptive Use Rachel E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) STANDARD PATENT (11) Application No. AU 2015336929 B2 (19) AUSTRALIAN PATENT OFFICE
(12) STANDARD PATENT (11) Application No. AU 2015336929 B2 (19) AUSTRALIAN PATENT OFFICE (54) Title Methods of reducing mammographic breast density and/or breast cancer risk (51) International Patent Classification(s) A61K 31/568 (2006.01) A61K 31/585 (2006.01) A61K 31/4196 (2006.01) A61P 35/00 (2006.01) A61K 31/5685 (2006.01) A61P 43/00 (2006.01) (21) Application No: 2015336929 (22) Date of Filing: 2015.10.22 (87) WIPO No: W016/061615 (30) Priority Data (31) Number (32) Date (33) Country 62/067,297 2014.10.22 US (43) Publication Date: 2016.04.28 (44) Accepted Journal Date: 2021.03.18 (71) Applicant(s) Havah Therapeutics Pty Ltd (72) Inventor(s) Birrell, Stephen Nigel (74) Agent / Attorney Adams Pluck, Suite 4, Level 3 20 George Street, Hornsby, NSW, 2077, AU (56) Related Art WO 2002/009721 Al MOUSA, N.A. et al. "Aromatase inhibitors and mammographic breast density in postmenopausal women receiving hormone therapy" Menopause: The Journal of The North American Menopause Society (2008) Vol.15 No.5, pages 875 to 884 WO 2009/036566 Al SMITH, J. et al. "A Pilot Study of Letrozole for One Year in Women at Enhanced Risk of Developing Breast Cancer: Effects on Mammographic Density" Anticancer Research (2012) Vol.32 No.4, pages 1327 to 1332 OUIMET-OLIVA, D. et al. Canadian Association of Radiologists Journal (1981) Vol.32 No.3, pages 159 to 161 (see online PubMed Abstract PMID: 7298699) (12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International -

Annex D to the Report of the Panel to Be Found in Document WT/DS320/R
WORLD TRADE WT/DS320/R/Add.4 31 March 2008 ORGANIZATION (08-0902) Original: English UNITED STATES – CONTINUED SUSPENSION OF OBLIGATIONS IN THE EC – HORMONES DISPUTE Report of the Panel Addendum This addendum contains Annex D to the Report of the Panel to be found in document WT/DS320/R. The other annexes can be found in the following addenda: – Annex A: Add.1 – Annex B: Add.2 – Annex C: Add.3 – Annex E: Add.5 – Annex F: Add.6 – Annex G: Add.7 WT/DS320/R/Add.4 Page D-1 ANNEX D REPLIES OF THE SCIENTIFIC EXPERTS TO QUESTIONS POSED BY THE PANEL A. GENERAL DEFINITIONS 1. Please provide brief and basic definitions for the six hormones at issue (oestradiol-17β, progesterone, testosterone, trenbolone acetate, zeranol, and melengestrol acetate), indicating the source of the definition where applicable. Dr. Boisseau 1. Oestradiol-17β is the most active of the oestrogens hormone produced mainly by the developing follicle of the ovary in adult mammalian females but also by the adrenals and the testis. This 18-carbon steroid hormone is mainly administered as such or as benzoate ester alone (24 or 45 mg for cattle) or in combination (20 mg) with testosterone propionate (200 mg for heifers), progesterone (200 mg for heifers and steers) and trenbolone (200 mg and 40 mg oestradiol-17β for steers) by a subcutaneous implant to the base of the ear to improve body weight and feed conversion in cattle. The ear is discarded at slaughter. 2. Progesterone is a hormone produced primarily by the corpus luteum in the ovary of adult mammalian females. -

Flufenamic Acid, Mefenamic Acid and Niflumic Acid Inhibit Single Nonselective Cation Channels in the Rat Exocrine Pancreas
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Volume 268, number 1, 79-82 FEBS 08679 July 1990 Flufenamic acid, mefenamic acid and niflumic acid inhibit single nonselective cation channels in the rat exocrine pancreas H. Gagelein*, D. Dahlem, H.C. Englert** and H.J. Lang** Max-Planck-Institutfir Biophysik, Kennedyallee 70, D-600 Frankfurt/Main 70, FRG Received 17 May 1990 The non-steroidal anti-inflammatory drugs, flufenamic acid, mefenamic acid and niflumic acid, block Ca2+-activated non-selective cation channels in inside-out patches from the basolateral membrane of rat exocrine pancreatic cells. Half-maximal inhibition was about 10 PM for flufenamic acid and mefenamic acid, whereas niflumic acid was less potent (IC,, about 50 PM). Indomethacin, aspirin, diltiazem and ibuprofen (100 /IM) had not effect. It is concluded that the inhibitory effect of flufenamate, mefenamate and niflumate is dependent on the specific structure, consisting of two phenyl rings linked by an amino bridge. Mefenamic acid; Flufenamic acid; Niflumic acid; Indomethacin; Non-selective cation channel; Rat exocrine pancreas 1. INTRODUCTION indomethacin, ibuprofen, diltiazem and acetylsalicylic acid (aspirin) were obtained from Sigma (Munich, FRG). The substances were dissolved in dimethylsulfoxide (DMSO, Merck, Darmstadt, FRG, Recently it was reported that the drug, 3 ’ ,5-dichloro- 0.1% of total volume) before addition to the measuring solution. diphenylamine-2-carboxylic acid (DCDPC), blocks DMSO alone had no effect on the single channel recordings. non-selective cation channels in the basolateral mem- 2.2. Methods brane of rat exocrine pancreatic cells [ 11. -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Case: Management Issues
Volume 9, Issue 1 (January 2013) This clinical e-newsletter from The North American Menopause Society (NAMS) presents questions and cases commonly seen in a menopause specialist’s practice. Recognized experts in the field provide their opinions and practical advice. Wen Shen, MD, MPH, the Editor of Menopause e-Consult, encourages your suggestions for future topics. Note that the opinions expressed in the commentaries are those of the authors and are not necessarily endorsed by NAMS or Dr. Shen. Case: products were used by women in 2003.2 A patient requests your advice about Presumably, this approach to the aging US testosterone from a compounding pharmacy to female population and the increasing 3 supplement her hormone therapy. How should prevalence of low sexual desire with age you advise her? Are there any guidelines for augments demand for testosterone products for 4,5 dosing testosterone ordered from these women. As demonstrated in these reviews, pharmacies? evidence documents that testosterone treatment (local/clitoral, vaginal, and systemic) increases Management issues by: sexual desire and genital sensitivity, and might improve the intensity of orgasm. Prospective, James A. Simon, MD, CCD, randomized, clinical trials of a testosterone NCMP, FACOG patch developed specifically for women Clinical Professor, Department demonstrated a statistically significant increase of Ob/Gyn George Washington University in the number of satisfying sexual events and School of Medicine improved desire, arousal, orgasm, pleasure, Women’s Health & Research ® responsiveness, and self-image—while Consultants Washington, DC decreasing sexual concerns and distress. These findings were consistent in surgically and naturally menopausal women already on The controversy over compounding rages on. -

Progestin-Based Contraceptive on the Same
PROGESTIN-BASED CONTRACEPTIVE ON THE SAME DAY AS MEDICAL ABORTION Jeanna Park, MD1, Nuriya Robinson, MD1, Ursula Wessels, MD2, James Turner, MD2, Stacie Geller, PhD1 1Department of Obstetrics and Gynecology, University of Illinois, Chicago, USA 2Department of Obstetrics and Gynecology, Lower Umfolozi District War Memorial Hospital, Empangeni, South Africa INTRODUCTION AND OBJECTIVES METHODS • Major cause of maternal mortality in South Africa = unsafe abortion Retrospective chart review in KwaZulu Natal, South Africa - Lower • New focus on family planning – providing immediate contraception with Umfolozi District War Memorial Hospital and Eshowe Hospital. etonogestrel implant or depot medroxyprogesterone acetate (DMPA) injection at the same time as medical abortion Inclusion criteria: • Historically, contraception offered at second follow-up visit after medical • Pregnant women aged 15-49 abortion complete – but many women lost to follow-up and never receive • Gestational age ≤ 63 days by ultrasound contraception (3) • Underwent medical abortion between August 2013 and July 2014 • Studies support when contraception is given at time of abortion, • Followed medical abortion protocol with oral mifepristone continuation rates high (4) and repeat abortion rates low (5) 200mg followed by sublingual misoprostol 800mcg 24 hours later • Theoretical risk - providing a progestin-based contraceptive (i.e. • Received either the etonogestrel implant or DMPA injection for etonogestrel or DMPA) at time of medical abortion may interfere with contraception -

21225 Mirena Clinical PREA
CLINICAL REVIEW Application Type NDA Application Number 21-225 (SE1- Applicant submission 027) Priority or Standard Priority Submit Date March 31, 2009 Received Date April 1, 2009 PDUFA Goal Date October 1, 2009 Division / Office Division of Reproductive and Urologic Products (DRUP) / Office of Drug Evaluation III (ODE III) Reviewer Name Gerald Willett M.D. Review Completion Date September 16, 2009 Established Name Levonorgestrel-releasing intrauterine system (LNG IUS) Trade Name Mirena® Therapeutic Class Progestin-containing intrauterine device Applicant Bayer HealthCare Pharmaceuticals Inc. Formulation Intrauterine device Dosing Regimen Insertion into the uterine cavity (5 year contraceptive efficacy) Indication Treatment of heavy menstrual bleeding for women who choose to use intrauterine contraception as their method of contraception Intended Population Women of childbearing age Template Version: March 6, 2009 Clinical Review Gerald Willett, M.D. NDA 21-225, SE1 Mirena® (levonorgestrel-releasing intrauterine system) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT....................................... 10 1.1 Recommendation on Regulatory Action ........................................................... 10 1.2 Risk Benefit Assessment.................................................................................. 10 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies . 13 1.4 Recommendations for Postmarket Requirements and Commitments .............. 13 2 INTRODUCTION AND REGULATORY BACKGROUND ..................................... -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -

Pharmacology/Therapeutics II Block III Lectures 2013-14
Pharmacology/Therapeutics II Block III Lectures 2013‐14 66. Hypothalamic/pituitary Hormones ‐ Rana 67. Estrogens and Progesterone I ‐ Rana 68. Estrogens and Progesterone II ‐ Rana 69. Androgens ‐ Rana 70. Thyroid/Anti‐Thyroid Drugs – Patel 71. Calcium Metabolism – Patel 72. Adrenocorticosterioids and Antagonists – Clipstone 73. Diabetes Drugs I – Clipstone 74. Diabetes Drugs II ‐ Clipstone Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones Date: Thursday, March 20, 2014-8:30 AM Reading Assignment: Katzung, Chapter 37 Key Concepts and Learning Objectives To review the physiology of neuroendocrine regulation To discuss the use neuroendocrine agents for the treatment of representative neuroendocrine disorders: growth hormone deficiency/excess, infertility, hyperprolactinemia Drugs discussed Growth Hormone Deficiency: . Recombinant hGH . Synthetic GHRH, Recombinant IGF-1 Growth Hormone Excess: . Somatostatin analogue . GH receptor antagonist . Dopamine receptor agonist Infertility and other endocrine related disorders: . Human menopausal and recombinant gonadotropins . GnRH agonists as activators . GnRH agonists as inhibitors . GnRH receptor antagonists Hyperprolactinemia: . Dopamine receptor agonists 1 Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. 1. Overview of Neuroendocrine Systems The neuroendocrine -

Safety and Efficacy of Testosterone for Women: a Systematic Review and Meta-Analysis of Randomised Controlled Trial Data
Articles Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data Rakibul M Islam, Robin J Bell, Sally Green, Matthew J Page, Susan R Davis Summary Background The benefits and risks of testosterone treatment for women with diminished sexual wellbeing remain Lancet Diabetes Endocrinol 2019 controversial. We did a systematic review and meta-analysis to assess potential benefits and risks of testosterone for Published Online women. July 25, 2019 http://dx.doi.org/10.1016/ S2213-8587(19)30189-5 Methods We searched MEDLINE, Embase, the Cochrane Central Register of Controlled Trials, and Web of Science for See Online/Comment blinded, randomised controlled trials of testosterone treatment of at least 12 weeks’ duration completed between http://dx.doi.org/10.1016/ Jan 1, 1990, and Dec 10, 2018. We also searched drug registration applications to the European Medicine Agency and S2213-8587(19)30251-7 the US Food and Drug Administration to identify any unpublished data. Primary outcomes were the effects of Women’s Health Research testosterone on sexual function, cardiometabolic variables, cognitive measures, and musculoskeletal health. This Program (R M Islam PhD, study is registered with the International Prospective Register of Systematic Reviews (PROSPERO), number Prof R J Bell MBBS, Prof S R Davis MBBS), School CRD42018104073. of Public Health and Preventive Medicine, Monash University, Findings Our search strategy retrieved 46 reports of 36 randomised controlled trials comprising -
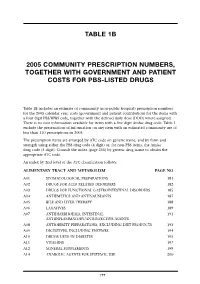
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine