PREVENT ANEMIA for BETTER HEALTH: Research Brief
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bardhaman Zilla Parishad Court Compound, Bardhaman-713101
Bardhaman Zilla Parishad Court Compound, Bardhaman-713101 Memo No ... .3.Q.~....../BZP/3rd SFC/ (1st lnst. 2014-15)/2016-17 Date ...~:?./..9.~.../2017 ORDER In pursuance of G.O. No. 230 (Sanction)-PN/P/II/1G-6/201O(Pt.-1) dated 06-01-2016 of the Joint Secretary. Panchayat & Rural Development. Govt. of West Bengal a total sum of Rs. 27,96,07,500/• (Rupees twenty seven crore ninety six lakh seven thousand five hundred) only have been transferred to the F.T. A/c of this Zilla Parishad as the 1st installment of the 3RD State Finance Commission Grant for the year 2014-15 of Bardhaman District. Out of the total amount of Rs. 27,96.07.500/-(Rupees twenty seven crore ninety six lakh seven thousand five hundred) only. Rs. 5,03,29,400/-(Rupees five crore three lakh twenty- nine thousand four hundred) only is the share of 31 nos. of Panchayat Samities as shown in Annexure-A. Now as per decision taken by the Bardhaman Zilla Parishad this fund being Rs. 5.03.29.400/-(Rupees five crore three lakh twenty- nine thousand four hundred) only is transferred to the FT A/Cs of 31 nos. of Panchayat Samities as shown in Annexure-A of this order. As soon as the amounts will be credited to the respective FT NCs of the Panchayat Samities. the Executive Officers. will withdraw the amounts from the FT A/Cs and deposit the same to the local funds accounts in the treasury for utilization as per the approved Annual Action Plan of G.O. -

E2767 V. 2 Public Disclosure Authorized ACCELERATED DEVELOPMENT of MINOR IRRIGATION (A.D.M.I) PROJECT in WEST BENGAL
E2767 v. 2 Public Disclosure Authorized ACCELERATED DEVELOPMENT OF MINOR IRRIGATION (A.D.M.I) PROJECT IN WEST BENGAL ENVIRONMENTAL ASSESSMENT Public Disclosure Authorized ANNEXURE (Part II) November 2010 Public Disclosure Authorized Public Disclosure Authorized Annexure - I - Map of West Bengal showing Environmental Features Annexure – II - Sample Blocks Annexure – III - Map of West Bengal Soils Annexure – IV - Ground Water Availability in Pilot Districts Annexure – V - Ground Water Availability in non-pilot districts Annexure – VI - Arsenic Contamination Maps of Districts Annexure – VII - Details of Wetlands more than 10 ha Annexure – VIII - Environmental Codes of Practice Annexure – IX - Terms of Reference for Limited EA Annexure – X - Environmental Survey Report of Sample Blocks Annexure – XI - Stakeholder Consultation Annexure – XII - Primary & Secondary Water Quality Data Annexure – XIII - Primary & Secondary Soil Quality Data Annexure – XIV - EMP Master Table ii Annexure II Sample Blocks for Environmental Assessment Agro- Hydrogeological No. of climatic Soil group District Block Status of the Block Samples zone Hill Zone Acid soils/sandy Jalpaiguri Mal Piedmont zone 1 loam Terai Acid soils/sandy Darjeeling Phansidewa Piedmont zone 1 Teesta loam Flood plain Acid soils/sandy Jalpaiguri Dhupguri Recent to sub-recent 1 loam alluvium Acid soils/sandy Coochbehar Tufangunge II Recent to sub-recent 1 loam alluvium Acid soils/sandy Coochbehar Sitai Recent to subrecent 1 loam alluvium Vindhyan Alluvial/sandy Dakshin Gangarampur( Older alluvium -
Department of Planning & Statistics
PURBA Bureau of Applied Economics & Statistics Department of Planning & Statistics. Government of West Bengal DISTRICT STATISTICAL HANDBOOK 2017 PURBA BARDHAMAN Bureau of Applied Economics & Statistics Department of Planning & Statistics . Government of West Bengal Contents Sl. Table Page Description No. No. No. RAINFALL, CLIMATE AND LOCATION 1 1.1 Geographical Location 1 2 1.2 Monthly Rainfall 1 3 1.3 Maximum and Minimum Temperature by month 2 4 1.4 Mean Maximum and Mean Minimum Temperature by month 2 AREA AND POPULATION 5 2.1 Administrative Units 3 6 2.1(a) Assembly and Parliamentary Constituencies 4 7 2.1(b) Number of Seats in Municipal Corporations, Municipalities and Panchayats 4 8 2.2 Area, Population and Density of Population 5 9 2.3 Growth of Population by sex 6 10 2.4(a) Distribution of Rural & Urban Population by sex, 2001 7 11 2.4(b) Distribution of Rural & Urban Population by sex, 2011 9 12 2.5(a) Distribution of Population by sex & by age group, 2001 11 13 2.5(b) Distribution of Population by sex & by age group, 2011 12 14 2.6 Distribution of Population by sex in different towns 13 15 2.7 Distribution of Population over different categories of workers and non-workers 15 16 2.8 Distribution of Population over different categories of workers and non-workers by sex 17 17 2.9 Scheduled Caste and Scheduled Tribe Population by sex 18 18 2.10 Population by religion 20 19 2.10(a) Population by religion & by sex 21 20 2.11 Disabled Persons by the type of disability & by sex 25 PUBLIC HEALTH 21 3.1 Medical Facilities 26 22 3.2 Family -

I Tender No. WTL/PAR/AC/19-20/006 Dated 07/06/2019
WEBEL TECHNOLOGY LIMITED CORRIGENDUM – I Tender No. WTL/PAR/AC/19-20/006 dated 07/06/2019 1. Date and time of Bid Submission has been extended up to 8th July 2019 at 12.00 hrs. 2. Date and time of Bid Opening has been extended up to 10th July 2019 at 12.00 hrs. 3. Date and time of EMD & Tender Fee submission has been extended up to 10th July 2019 at 11.00 hrs. WEBEL TECHNOLOGY LIMITED Contact Details of WBSWAN SL Mobile DHQ Contact Name Location DHQ POP No. Number Details Total Total Webel SL 1 Jadu Gopal Mondal 9051041622 DHQ Name Number of Number of Bhavan No. SDHQ BHQ Webel 2 Soma Dey 9831056289 1 Bankura 2 22 Bhavan Webel 3 Subrata Dutta 9830325404 2 Birbhum 2 19 Bhavan Mrinmoy Webel 4 9832250828 3 Coochbehar 4 13 Chattopadhaya Bhavan 5 Ambar Nath Banerjee SHQ 9836383806 4 Dakshin Dinajpur 1 8 Aniruddha 6 SHQ 9051377550 5 Darjeeling 3 12 Chakroborty 7 Anupam Ghosh SHQ 9051309988 6 East Medinipur 4 25 7 Hooghly 3 18 8 Biplab Dhar SHQ 9231815309 8 Howrah 1 14 9 Debasish Senapati SHQ 9903364334 9 Jalpaiguri 2 7 10 Hemanta Mondal SHQ 8013604600 10 Malda 1 16 11 Prasanta Ghosh SHQ 8621053778 11 Murshidabad 5 26 12 Pulakesh Das SHQ 9836368068 12 Nadia 4 17 North 24 13 Rahul Tripathi SHQ 9051345445 13 3 22 Parganas Ram Rajib Pashchim 14 SHQ 9830753488 14 2 8 Bhattacharjee Burdwan 15 Saikat Goswami SHQ 9051569955 15 Purba Burdwan 2 23 16 Sougata Polley SHQ 9432169916 16 Purulia 1 19 South 24 17 Sudip Kundu SHQ 9051073838 17 5 29 Parganas 18 Sumanendu Das SHQ 9836303300 18 Uttar Dinajpur 2 9 19 Suvodip Roy SHQ 9830244528 19 West Medinipur 2 21 20 Thakur Das Sur SHQ 9831660438 20 Alipurduar 0 6 21 Jhargram 0 8 WEBEL TECHNOLOGY LIMITED SOUTH 24 PARGANS SL. -

Name of the State : West Bengal Name of the District : Burdwan
Name of the State : West Bengal Name of the District : Burdwan Information on the Employees of Gram Panchayats Name of Name of the Gram Sl No. Name of the Employees Official Address Designation E-mail address Mobile No. Block Panchayat Office of the Billeswar Gram Panchayat, P.O.- [email protected] NS Billeswar, Dist.- om 1 Ketugram-II Billeswar Supriya Parui Bardhaman 9831652681 Office of the Billeswar Gram Panchayat, P.O.- [email protected] Secretary Billeswar, Dist.- om 2 Ketugram-II Billeswar Sanjay Barui Bardhaman 9800386986 Office of the Billeswar Gram Panchayat, P.O.- [email protected] Sahayak Billeswar, Dist.- om 3 Ketugram-II Billeswar Dilip Rakshit Bardhaman 9832715461 Office of the Billeswar Gram [email protected] Panchayat, P.O.‐ Billeswar, GP Karmee m Dist.‐ Bardhaman 4 Ketugram-II Billeswar Tirthankar Majumder 8001717433 Office of the Billeswar Gram [email protected] Panchayat, P.O.‐ Billeswar, GP Karmee m Dist.‐ Bardhaman 5 Ketugram-II Billeswar Uday Kr. Ghosh 9093240043 Office of the Billeswar Gram [email protected] Panchayat, P.O.‐ Billeswar, GRS m Dist.‐ Bardhaman 6 Ketugram-II Billeswar Palash Banerjee 9933980813 Office of the Billeswar Gram [email protected] Panchayat, P.O.‐ Billeswar, AGRS m Dist.‐ Bardhaman 7 Ketugram-II Billeswar Malay Kr. Ghosh 8016877814 Name of the State : West Bengal Name of the District : Burdwan Information on the Employees of Gram Panchayats Name of Name of the Gram Sl No. Name of the Employees Official Address Designation E-mail address Mobile No. Block Panchayat Office -
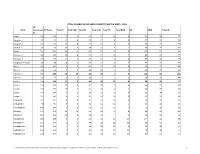
Total Number of Gp and Ps Constituency & Seats , 2013
TOTAL NUMBER OF GP AND PS CONSTITUENCY & SEATS , 2013 GP Block Constituenc GP Seats Total ST Total STW Total SC Total SCW Total BC Total BCW UR URW Total W ies Andal 146 146 7 3 49 24 16 6 74 39 72 Ausgram I 92 92 11 6 29 12 5 3 47 24 45 Ausgram II 113 113 15 8 40 18 0 0 58 29 55 Barabani 92 92 13 7 28 12 3 1 48 24 44 Bhatar 201 201 18 11 62 27 12 6 109 52 96 Burdwan I 162 162 10 6 51 21 15 9 86 43 79 Burdwan II 116 116 11 5 45 21 0 0 60 30 56 Durgapur-Faridpur 88 88 6 3 29 12 6 4 47 23 42 Galsi I 141 141 4 3 49 22 14 6 74 37 68 Galsi II 116 116 7 2 44 20 3 3 62 29 54 Jamalpur 205 206 28 15 65 29 7 3 106 53 100 Jamuria 93 93 8 5 28 11 7 3 50 25 44 Kalna I 154 155 17 5 43 24 17 6 78 42 77 Kalna II 124 124 20 9 40 20 0 0 64 31 60 Kanksa 132 132 13 9 47 20 4 2 68 33 64 Katwa I 129 129 2 0 43 19 16 9 68 34 62 Katwa II 101 101 0 0 30 14 19 8 52 27 49 Ketugram I 117 117 0 0 31 12 12 8 74 37 57 Ketugram II 90 90 0 0 32 14 11 5 47 24 43 Khandaghosh 143 143 1 0 54 25 13 7 75 36 68 Memari I 171 171 26 10 56 29 0 0 89 43 82 Memari II 115 115 21 8 28 14 7 3 59 31 56 Mongolkote 198 198 3 1 62 26 26 15 107 52 94 Monteswar 176 176 3 2 44 22 38 16 91 45 85 Pandabeswar 112 112 7 4 34 18 12 4 59 29 55 Purbasthali I 154 154 7 1 43 24 25 11 79 39 75 Purbasthali II 156 156 6 2 40 16 25 15 85 42 75 C:\Documents and Settings\User\Local Settings\Temp\Constituency Report & Comparison (Pradhan & Upa-Pradhan)_16DB91F\Block wise-GP Const 1 GP Block Constituenc GP Seats Total ST Total STW Total SC Total SCW Total BC Total BCW UR URW Total W ies Raina I 139 139 9 -

List of Covid Vaccination Session Sites on 30-07-2021
List of Covid Vaccination Session Sites on 30-07-2021 Type of Category of CVC Type of Vaccine Sl. CVC/WPCVC CVC (General (Covishield / District Name of Block / ULB Name of CVC / WPCVC No. ID (Govt. or CVC/Workplace Covaxin / Pvt.) CVC) Sputnik V) 1 Purba Bardhaman KALNA SDH W700637 KALNA SUB DIVISION HOSPITAL (HMT) GOVT. Workplace CVC COVAXIN 2 Purba Bardhaman KALNA SDH W700637 KALNA SUB DIVISION HOSPITAL (HMT) GOVT. Workplace CVC COVISHIELD 3 Purba Bardhaman KATWA SDH G547363 KATWA SDH GOVT. general CVC covishield 4 Purba Bardhaman KATWA SDH G588849 KATWA SDH GOVT. general CVC COVAXIN 5 Purba Bardhaman Ketugram-I G547341 Ramjibanpur BPHC Covishield Govt General CVC Covishield 6 Purba Bardhaman Ketugram-I G616686 PANDUGRAM PHC, Ramjibanpur Govt. General CVC Covishield 7 Purba Bardhaman Ketugram-I G628272 Ankhona PHC, Ramjibanpur Govt. General CVC Covishield 8 Purba Bardhaman Katwa-I G547333 Srikhanda BPHC GOVT General CVC COVISHIELD MEMARI RH COVISHIELD SECOND DOSE 9 Purba Bardhaman MEMARI MUNICIPALITY G588860 GOVT. General CVC COVISHIELD SESSION 10 Purba Bardhaman MEMARI MUNICIPALITY G547350 MEMARI RH COVAXIN SECOND DOSE SESSION GOVT. General CVC COVAXIN 11 Purba Bardhaman MONGOLKOTE G547331 MONGOLKOTE BPHC GOVT General CVC COVISHIELD 12 Purba Bardhaman MONGOLKOTE G547438 SINGOT RH GOVT General CVC COVISHIELD 13 Purba Bardhaman KHANDAGHOSH G547335 KHANDAGHOSH BPHC GOVT General CVC COVISHIELD 14 Purba Bardhaman KHANDAGHOSH G629195 GOPALBERA SC GOVT General CVC COVISHIELD 15 Purba Bardhaman Burdwan - I G547332 Kurmun BPHC Covishield GOVT General CVC COVISHIELD 16 Purba Bardhaman Burdwan - I W710842 BURDWAN-I PRIORITY GROUP GOVT. Workplace CVC COVISHIELD 17 Purba Bardhaman Burdwan - I W730415 Indane Priority (HCW Family Member Priority) GOVT. -

District Election Officer Purba Bardhaman
District Election Management Plan General Election to West Bengal Legislative Assembly - 2021 District Election Officer Purba Bardhaman Md. Enaur Rahman, WBCS (Exe.) District Magistrate & District Election Officer Purba Bardhaman, West Bengal, PIN – 713101 Phone No :- (Office) : 0342-2662428 (Residence) : 0342-2625700/2625702 Fax : 91-342-2625703 PBX : 2662408-412 Extn. 100 E-Mail ID :- [email protected] Foreword The process of General Election to WBLA-21 having started, this booklet on District Election Management Plan is being published keeping in mind the various facts of the works related to Election in the Purba Bardhaman District. This booklet not only contains the basic data of the district regarding Election but also focuses on the analysis of data, as well as the plans we have kept ready as we approach nearer to conduct of election. Many of the data being dynamic, and changes almost daily. The book also contains maps developed by NRDMS Section of this Office which will be helpful for locating the Polling Stations. This booklet is an amalgamation of summary of plans and preparedness of different Cells like EVM, Polling Personnel, Complaint Monitoring, Training, Expenditure Monitoring, MCC, IT, Postal Ballot (Absentee Voter) etc, each cell having their detail plans at their ends. Purba Bardhaman The 29th March, 2021. Md. Enaur Rahman, WBCS (Exe.) CONTENTS District the Purba Bardhaman ......................................................................................................5 Administrative Map ....................................................................................................................7 -

Purba Bardhaman District at a Glance
PURBA BARDHAMAN DISTRICT AT A GLANCE The name Burdwan is the anglicized form of Barddhaman. (also spelled as Burdwan or Burdhman) is a district in West Bengal. There are two schools of thoughts about the name Barddhaman. It might have been named after the 24th Jaina Tirthankar. According to Kalpasutra of the Jains, Mahavira spent sometime in Astikagram which was formerly known as Barddhaman. According to the second school, Barddhaman means prosperous growth centre. In the progress of Aryanisation from Upper Ganges valley, the frontier colony was called Barddhaman as a landmark of growth and prosperity. The name came to stay as the Aryans failed to consolidate their gains further east. District : Purba Bardhaman, State : West Bengal Social & Resource Map Showing River System of Purba Bardhaman District The main towns of the district is Burdwan, Kalna & Katwa Geography: Total Geographical Area: 5432.69 sq. km. The district extends from 22°56' to 23°53' N latitude and from 86°48' to 88°25' E longitudes. Lying within Burdwan Division, the district is bounded on the north by Birbhum and Murshidabad, on the east by Nadia, on the south by Hooghly, Bankura and Purulia and on the west by Paschim Bardhaman districts. RIVERS : The river system in Purba Barddhaman includes the Bhagirathi-Hooghly in the east, the Ajoy and its tributaries in the north and the Dwarakeswar, the Damodar and its branches in the south-west. Besides, there are innumerable Khals and old river beds all over the area. WATER RESOURCES : There are many tanks, wells, canals, swamps and bils are found all over the district. -

A Case Study of Barddhaman District, West Bengal, India Amit Bhattacharyya
World Academy of Science, Engineering and Technology International Journal of Environmental and Ecological Engineering Vol:13, No:8, 2019 Spatial Disparity in Education and Medical Facilities: A Case Study of Barddhaman District, West Bengal, India Amit Bhattacharyya 1 in a few centres. These centres grow so rapidly that it Abstract—The economic scenario of any region does not show accentuates the inequality within the areas as well as regions the real picture for the measurement of overall development. [8]. In the context of a high rate of growth of the development Therefore, economic development must be accompanied by social that goes side by side with rising inter-state as well as inter- development to be able to make an assessment to measure the level of development. The spatial variation with respect to social regional inequality, developmental facilities are distributed development has been discussed taking into account the quality of unequally leading to differential levels of development across functioning of a social system in a specific area. In this paper, an the regions. Such unchecked and uncontrolled process of attempt has been made to study the spatial distribution of social growth leads to regional disparities [9]. The balanced infrastructural facilities and analyze the magnitude of regional development can be achieved if selfless efforts are made by disparities at inter- block level in Barddhman district. It starts with the detailed account of the selection process of social infrastructure the local political parties, the government and policy makers. indicators and describes the methodology employed in the empirical analysis. Analyzing the block level data, this paper tries to identify II. -

Block Observers List
Block Observers List SL Official Name Present Designation Alloted Block District No. Contact No. South 24 1 Shri Paritosh Roy Special Secretary 9073387942 Bishnupur-I & Bishnupur-II Parganas 2 Shri Dipankar Chowdhury Special Secretary 9836460605 Alipurduar-II & Kumargram Alipurduar 3 Shri Tarun Kumar Mukhopadhyay Special Secretary 9007159923 Alipurduar-I & kalchini Alipurduar 7602029297 4 Shri Jyotishman Chattopadhyay Director of Local Bodies Mal Jalpaiguri 7431025231 5 Shri Subhas Chandra Mazumdar DCDC 9635692745 Mathabhanga-I & Mathabhanga-II Cooch Behar Special Secretary & Ex-Officio South 24 6 Smt.Namita Roy (Mallick) 9073387938 Budge Budge-I & Budge Budge-II Director of Culture Parganas South 24 7 Md Abdul Gani Special Secretary 9073389854 Magrahat-I & Magrahat-II Parganas Shri Ritendra Narayan Basu Roy 8 Special Secretary 6295655529 Matiali & Nagrakata Jalpaiguri Choudhury Dakshin 9 Shri Arup Sengupta Special Secretary 7479011573 Kushmandi & Banshihari Dinajpur South 24 10 Shri Siladitya Basuray Special Secretary 9073389812 Mandirbazar & Mathurapur-II Parganas 6295662192 11 Shri Debal Kumar Ghosh CEO,HIT Rajganj & Jalpaiguri Sadar Jalpaiguri 8145802742 12 Shri Krishnendu Sadhukhan Managing Director,WBMTD Ltd. 8017075920 Dinhata-I & Dinhata-II Cooch Behar Joint Commissioner, Food Safety 13 Smt. Sunita Mitra Deb 9434077557 Singur & Srirampur Uttarpara Hooghly & Security 14 Shri Debashis sarkar Dy. R.R.C. 9434240875 Neturia & Santuri Purulia South 24 15 Shri Mriganka Biswas MD & Joint Secretary 9073389683 Kulpi & Kakdwip Parganas Purba 16 Shri Sital Chandra Mondal Joint Secretary 9732267898 Ausgram-I & Ausgram-II Bardhaman Commissioner,Siliguri Municipal 17 Shri Sonam Wangdi Bhutia 8967296341 Goalpokhar-I & Goalpakhar-II Uttar Dinajpur corporation General Manager,WB Medical 18 Shri Atanu Kumar Roy 9474625753 Pandua & Balagarh Hooghly Service Corporation Ltd. -

List of Covid Vaccination Session Sites on 17-07-2021 Category of CVC Type of Vaccine Name of Block / Name of CVC / Type of CVC (General Sl
List of Covid Vaccination Session Sites on 17-07-2021 Category of CVC Type of Vaccine Name of Block / Name of CVC / Type of CVC (General Sl. No. District CVC/WPCVC ID (Covishield / ULB WPCVC (Govt. or Pvt.) CVC/Workplace Covaxin / Sputnik V) CVC) Purba 1 Memari-II G547330 PAHARHATI-BPHC GOVT General CVC COVISHIELD Bardhaman Purba 2 Memari-II G629476 BEGUNIA SC GOVT General CVC COVISHIELD Bardhaman Purba 3 Memari-II G629463 BOHAR PHC GOVT General CVC COVISHIELD Bardhaman Purba 4 Memari-II G617625 PAHARHATI-SC GOVT General CVC COVISHIELD Bardhaman Purba 5 Memari-II G630779 BIJUR SC GOVT General CVC COVISHIELD Bardhaman Purba 6 Memari-II G629468 MONDALGRAM SC GOVT General CVC COVISHIELD Bardhaman Purba 7 Memari-II G629467 KUCHUT SC GOVT General CVC COVISHIELD Bardhaman Purba BARAPALASON 8 Memari-II G615662 GOVT General CVC COVISHIELD Bardhaman PHC Purba PAHARHATI-BPHC 9 MEMARI-II W710974 GOVT. WORKPLACE CVC COVISHIELD Bardhaman PIORITY GROUP Purba Madhabdihi BPHC 10 Raina II G547347 Govt General CVC Covishield Bardhaman Covishield Purba Gotan PHC 11 Raina II G615768 Govt General CVC Covishield Bardhaman Covishield Purba Painta PHC 12 Raina II G629399 Govt General CVC Covishield Bardhaman Covishield Purba Binodpur PHC 13 Raina II G629344 Govt General CVC Covishield Bardhaman Covishield Purba Chhotobainan SC 14 Raina II G629413 Govt General CVC Covishield Bardhaman Covishield Purba Deno HWC 15 Raina II G629414 Govt General CVC Covishield Bardhaman Covishield KALNA SUB Purba 16 KALNA SDH W700637 DIVISION GOVT. Workplace CVC COVAXIN Bardhaman