S6 Ivermectin.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Comparative Efficacies of Commercially Available Benzimidazoles Against Pseudodactylogyrus Infestations in Eels
DISEASES OF AQUATIC ORGANISMS Published October 4 Dis. aquat. Org. l Comparative efficacies of commercially available benzimidazoles against Pseudodactylogyrus infestations in eels ' Department of Fish Diseases, Royal Veterinary and Agricultural University, 13 Biilowsvej, DK-1870 Frederiksberg C, Denmark Department of Pharmacy, Royal Veterinary and Agricultural University, 13 Biilowsvej. DK-1870 Frederiksberg C,Denmark ABSTRACT: The antiparasitic efficacies of 9 benzimidazoles in commercially avalable formulations were tested (water bath treatments) on small pigmented eels Anguilla anguilla, expenmentally infected by 30 to 140 specimens of Pseudodactylogyrus spp. (Monogenea).Exposure time was 24 h and eels were examined 4 to 5 d post treatment. Mebendazole (Vermox; 1 mg 1-') eradicated all parasites, whereas luxabendazole (pure substance) and albendazole (Valbazen) were 100 % effective only at a concen- tration of 10 mg I-'. Flubendazole (Flubenol), fenbendazole (Panacur) and oxibendazole (Lodltac) (10 mg l-') caused a reduction of the infection level to a larger extent than did triclabendazole (Fasinex) and parbendazole (Helmatac).Thiabendazole (Equizole), even at a concentration as high as 100 mg l-', was without effect on Pseudodactylogyrus spp. INTRODUCTION range of commercially available benzimidazole com- pounds. If drug resistance will develop under practical The broad spectrum anthelmintic drug mebendazoIe eel-farm conditions in the future, it is likely to be was reported as an efficacious compound against infes- recognized during treatments with commercially avail- tations of the European eel Anguilla anguilla with gill able drug formulations. Therefore this type of drug parasitic monogeneans of the genus Pseudodactylo- preparations were used in the present study. gyms (Szekely & Molnar 1987, Buchmann & Bjerre- gaard 1989, 1990, Mellergaard 1989). -

Baylisascariasis
Baylisascariasis Importance Baylisascaris procyonis, an intestinal nematode of raccoons, can cause severe neurological and ocular signs when its larvae migrate in humans, other mammals and birds. Although clinical cases seem to be rare in people, most reported cases have been Last Updated: December 2013 serious and difficult to treat. Severe disease has also been reported in other mammals and birds. Other species of Baylisascaris, particularly B. melis of European badgers and B. columnaris of skunks, can also cause neural and ocular larva migrans in animals, and are potential human pathogens. Etiology Baylisascariasis is caused by intestinal nematodes (family Ascarididae) in the genus Baylisascaris. The three most pathogenic species are Baylisascaris procyonis, B. melis and B. columnaris. The larvae of these three species can cause extensive damage in intermediate/paratenic hosts: they migrate extensively, continue to grow considerably within these hosts, and sometimes invade the CNS or the eye. Their larvae are very similar in appearance, which can make it very difficult to identify the causative agent in some clinical cases. Other species of Baylisascaris including B. transfuga, B. devos, B. schroeder and B. tasmaniensis may also cause larva migrans. In general, the latter organisms are smaller and tend to invade the muscles, intestines and mesentery; however, B. transfuga has been shown to cause ocular and neural larva migrans in some animals. Species Affected Raccoons (Procyon lotor) are usually the definitive hosts for B. procyonis. Other species known to serve as definitive hosts include dogs (which can be both definitive and intermediate hosts) and kinkajous. Coatimundis and ringtails, which are closely related to kinkajous, might also be able to harbor B. -

Expert Review 2
2021 Expert Committee on Selection and Use of Essential Medicines Application review I.1 Albendazole, mebendazole and praziquantel for the indication of treatment of (item number) taeniid cestode cysts Does the application adequately ☒ Yes address the issue of the public health ☐ need for the medicine? No ☐ Not applicable Comments: The larval stages of three taeniid cestode parasites, Echinococcus granulosus, Echinococcus multilocularis and Taenia solium, produce cysts in humans that are of medical relevance. The diseases caused by these parasitic cysts are called cystic echinococcosis (CE), alveolar echinococcosis (AE), and cysticercosis (being neurocysticercosis (NCC) the most common form) respectively, and they are recognised by WHO as neglected tropical diseases. NCC is mainly a disease of poverty that predominantly affects rural populations in Africa, Asia and Latin America. Access to diagnostic and treatment, to better manage epilepsy and other NCC is a challenge for the people affected in these communities due to the availability and costs of specialised diagnostic and care. Stigma and social discrimination also mean that many people try to “hide” the disease. Briefly summarize the role of the The only real options for treatment of CE are albendazole (ALB) and Mebendazole proposed medicine(s) relative to other (MEB). ALB is the drug of choice as it has better bioavailability. ALB is also preferred to therapeutic agents currently included in MEB, because MEB requires a higher dose and a higher pill burden, for example, an the Model List, or available in the adult patient would require 8 tablets/day of MEB compared with 2 tablets/day ALB. market. ALB and praziquantel ( PZQ) are the only drugs used for the antiparasitic treatment of NCC. -
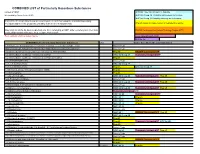
COMBINED LIST of Particularly Hazardous Substances
COMBINED LIST of Particularly Hazardous Substances revised 2/4/2021 IARC list 1 are Carcinogenic to humans list compiled by Hector Acuna, UCSB IARC list Group 2A Probably carcinogenic to humans IARC list Group 2B Possibly carcinogenic to humans If any of the chemicals listed below are used in your research then complete a Standard Operating Procedure (SOP) for the product as described in the Chemical Hygiene Plan. Prop 65 known to cause cancer or reproductive toxicity Material(s) not on the list does not preclude one from completing an SOP. Other extremely toxic chemicals KNOWN Carcinogens from National Toxicology Program (NTP) or other high hazards will require the development of an SOP. Red= added in 2020 or status change Reasonably Anticipated NTP EPA Haz list COMBINED LIST of Particularly Hazardous Substances CAS Source from where the material is listed. 6,9-Methano-2,4,3-benzodioxathiepin, 6,7,8,9,10,10- hexachloro-1,5,5a,6,9,9a-hexahydro-, 3-oxide Acutely Toxic Methanimidamide, N,N-dimethyl-N'-[2-methyl-4-[[(methylamino)carbonyl]oxy]phenyl]- Acutely Toxic 1-(2-Chloroethyl)-3-(4-methylcyclohexyl)-1-nitrosourea (Methyl-CCNU) Prop 65 KNOWN Carcinogens NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) IARC list Group 2A Reasonably Anticipated NTP 1-(2-Chloroethyl)-3-cyclohexyl-1-nitrosourea (CCNU) (Lomustine) Prop 65 1-(o-Chlorophenyl)thiourea Acutely Toxic 1,1,1,2-Tetrachloroethane IARC list Group 2B 1,1,2,2-Tetrachloroethane Prop 65 IARC list Group 2B 1,1-Dichloro-2,2-bis(p -chloropheny)ethylene (DDE) Prop 65 1,1-Dichloroethane -
Mebendazole 1
The European Agency for the Evaluation of Medicinal Products Veterinary Medicines Evaluation Unit EMEA/MRL/625/99-FINAL July 1999 COMMITTEE FOR VETERINARY MEDICINAL PRODUCTS MEBENDAZOLE SUMMARY REPORT (1) 1. Mebendazole is a benzimidazole anthelmintic which is used in both human and veterinary medicine. In veterinary medicine, it is administered orally to horses, at a target dose of 8.8 mg/kg bw and to sheep and goats at a target dose of 15 mg/kg bw. Mebendazole has also been used in game birds, pigs, deer, poultry and cattle, including lactating animals and laying birds, but these uses were not supported with regard to the establishment of MRLs. Mebendazole is authorised in a range of mono-preparations including premixes for medicated feed, pastes, tablets, liquids, granules, drenches and suspensions for oral administration. Mebendazole is also used in combination products additionally containing either metrifonate, closantel or minerals (selenium, cobalt). 2. The pharmacokinetics of mebendazole was studied in rats, mice, dogs, humans and several target species. In rats given oral doses in the range of 0.06 to 10 mg/kg bw 14C-mebendazole, most of the radioactivity was recovered from the organs of the gastrointestinal tract and consisted mostly of unmetabolised mebendazole. Less than 1% of the administered radioactivity was detected in blood. Excretion was predominantly via the faeces, with 70 to 90% of the faecal radioactivity consisting of unmetabolised mebendazole. In rat liver, 1 hour after administration, 15% of the radioactivity consisted of unmetabolised mebendazole. Four hours after administration, the percentage of mebendazole had declined to 1%. Absorption in humans was increased when the same dose was given with a meal. -
Summary of Product Characteristics 1. Name Of
Revised: November 2020 AN: 01025/2020 SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE VETERINARY MEDICINAL PRODUCT Droncit Tablets 50 mg 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 2.1 Active Constituents mg per tablet Praziquantel 50 For full list of excipients, see section 6.1 3. PHARMACEUTICAL FORM Tablet White tablets 4. CLINICAL PARTICULARS 4.1 Target species Dogs and cats. 4.2 Indications for use, specifying the target species For the treatment of adult tapeworms of dogs and cats. The tablets are effective against both immature and mature forms of adult tapeworms in both dogs and cats. The product is a highly effective treatment against all the common species of tapeworm infecting dogs and cats in the United Kingdom and Ireland including Echinococcus granulosus, Taenia ovis, Taenia pisiformis, Taenia multiceps, Taenia hydatigena, Taenia taeniaeformis, and Dipylidium caninum. Droncit is also effective against Echinococcus multilocularis (see 4.4) 4.3 Contraindications Do not administer to dogs weighing less than 2.5 kg Do not administer to unweaned puppies and kittens, as such animals are rarely infected with tapeworms. Page 1 of 5 Revised: November 2020 AN: 01025/2020 4.4 Special warnings for each target species Fleas serve as intermediate hosts for one common type of tapeworm - Dipylidium caninum. To avoid reinfection with this parasite, flea control of the animal and its housing should be carried out at the same time. Unless flea control is complete an infected flea population may survive: i.e. re-treatment of the animal may be necessary. As a precautionary measure to prevent the establishment of Echinococcus multilocularis in the UK and Ireland, it is recommended that all dogs and cats entering the country be treated with praziquantel. -
ALBENDAZOLE (Extrapolation to All Ruminants)
European Medicines Agency Veterinary Medicines and Inspections EMEA/MRL/865/03-FINAL June 2004 COMMITTEE FOR MEDICINAL PRODUCTS FOR VETERINARY USE ALBENDAZOLE (Extrapolation to all ruminants) SUMMARY REPORT (3) 1. Albendazole is a benzimidazole carbamate, used for the treatment of gastrointestinal infestations with roundworms, lungworms and tapeworms and adult flukes of Fasciola hepatica. Albendazole is currently entered into Annex I of Council Regulation (EEC) No. 2377/90 in accordance with the following table: Pharmacologically Marker residue Animal MRLs Target Other active substance(s) species tissues provisions Albendazole Sum of albendazole Bovine, 100 µg/kg Muscle sulphoxide, ovine 100 µg/kg Fat albendazole sulphone 1000 µg/kg Liver and albendazole 2- 500 µg/kg Kidney amino sulphone 100 µg/kg Milk expressed as albendazole 2. In reviewing the availability of endo- and ectoparasiticides for sheep and goats, albendazole was considered for extrapolation from bovine and ovine species to all ruminants. The considerations and criteria leading to the identification of albendazole are described in the Position Paper Regarding Availability of Veterinary Medicines – Extrapolation of MRLs (EMEA/CVMP/457/03-FINAL). 3. The scientific justification for this extrapolation was assessed in accordance with the Notes for Guidance on Risk Analysis Approach for Residues of Veterinary Medicinal Products in Food of Animal Origin (EMEA/CVMP/187/00-FINAL) and on the Establishment of Maximum Residue Limits for Minor Animal Species (EMEA/CVMP/153a/97-FINAL). 4. In setting the ADI in the original assessment of albendazole, the data summarised on the paragraphs below were considered. 5. The mode of action of albendazole is by binding strongly with the tubulin in the cells of nematodes. -

Efficacy and Tolerability of Quinacrine Monotherapy and Albendazole Plus Chloroquine Combination Therapy in Nitroimidazole-Refractory Giardiasis: a Tropnet Study
Klinik für Infektiologie & Spitalhygiene Efficacy and tolerability of quinacrine monotherapy and albendazole plus chloroquine combination therapy in nitroimidazole-refractory giardiasis: a TropNet study Andreas Neumayr, Mirjam Schunk, Caroline Theunissen, Marjan Van Esbroeck, Matthieu Mechain, Manuel Jesús Soriano Pérez, Kristine Mørch, Peter Sothmann, Esther Künzli, Camilla Rothe, Emmanuel Bottieau Journal Club 01.03.21 Andreas Neumayr Background on giardia treatment: • 1st-line treatment: 5-nitroimidazoles: metronidazole (1957), tinidazole, ornidazole, secnidazole • cure rate of 5NIs in 1st-line treatment: ~90% • in the last decade, an increase of 5NI-refractory giardia cases has been observed in travel medicine clinics across Europe: Hospital for Tropical Diseases, London: 2008: 15% --> 2013: 40% 70% of 5NI-refractory cases imported from India • 2nd-line treatment: effectiveness of a 2nd round with a 5NI: ~17% alternative drugs: albendazole, mebendazole, nitazoxanide, quinacrine, furazolidone, chloroquine, paromomycin 2012 TropNet member survey: 53 centres use 39 different treatment regimens, consisting of 7 different drugs in mono- or combination-therapy in various dosages and durations JC 01.03.21 Nabarro LE et al. Clin Microbiol Infect. 2015;21:791-6. • by 2013, there were only 13 reports of 2nd-line therapy for giardiasis (8 case series, 5 individual case reports): n=110 Cure rates Albendazole 6/32 18.7% Paromomycin 5/17 29.4% Nitazoxanide 2/5 40.0% Albendazole + 5-NI 42/53 79.2% Quinacrine 19/21 90.5% Quinacrine + 5-NI 14/14 100% Quinacrine + Paromomycin 2/2 100% • 2013: TropNet "GiardiaREF" study kick-off: Study on efficacy and tolerability of two 2nd-line regimens in nitroimidazole-refractory giardiasis: Quinacrine JC 01.03.21 Meltzer E et al. -

Equimax & Eraquell Oral Gel for Horses
Equimax & Eraquell Oral Gel for Horses Annual Wormer Pack [active ingredients: Ivermectin & Praziquantel] (POM-VPS) Revised AN Equimax Oral Gel for Horses January 2013 01009/2012 Eraquell Oral Gel for Horses December 2015 01163/2015 Page 1 of 15 SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE VETERINARY MEDICINAL PRODUCT Equimax Oral Gel for Horses 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each gram of Equimax contains Active substances Ivermectin ........................................................ 18.7 mg Praziquantel ..................................................... 140.3 mg Excipients Titanium dioxide (E171) ................................... 20 mg Propylene glycol ............................................... 731 mg For a full list of excipents, see section 6.1 3. PHARMACEUTICAL FORM Oral gel. 4. CLINICAL PARTICULARS 4.1 Target species Horses. 4.2 Indications for use, specifying the target species For the treatment of mixed cestode and nematode or arthropod infestations, due to adult and immature roundworms, lungworms, bots and tapeworms in horses: Nematodes Large-strongyle: Strongylus vulgaris (adult and arterial larvae) Strongylus edentatus (adult and L4 tissue larval stages) Strongylus equinus (adult) Triodontophorus spp. (adult) Small-strongyle: Cyathostomum: Cylicocyclus spp., Cylicostephanus spp., Cylicodontophorus spp., Gyalocephalus spp. (adult and non-inhibited mucosal larvae). Parascaris: Parascaris equorum (adult and larvae). Page 2 of 15 Oxyuris: Oxyuris equi (larvae). Trichostrongylus:Trichostrongylus -

Chemotherapy of Gastrointestinal Helminths
Chemotherapy of Gastrointestinal Helminths Contributors J. H. Arundel • J. H. Boersema • C. F. A. Bruyning • J. H. Cross A. Davis • A. De Muynck • P. G. Janssens • W. S. Kammerer IF. Michel • M.H. Mirck • M.D. Rickard F. Rochette M. M. H. Sewell • H. Vanden Bossche Editors H. Vanden Bossche • D.Thienpont • P.G. Janssens UNIVERSITATS- BlfiUOTHElC Springer-Verlag Berlin Heidelberg New York Tokyo Contents CHAPTER 1 Introduction. A. DAVIS A. Pathogenic Mechanisms in Man 1 B. Modes of Transmission 2 C. Clinical Sequelae of Infection 3 D. Epidemiological Considerations 3 E. Chemotherapy 4 F. Conclusion 5 References 5 CHAPTER 2 Epidemiology of Gastrointestinal Helminths in Human Populations C. F. A. BRUYNING A. Introduction 7 B. Epidemiological or "Mathematical" Models and Control 8 C. Nematodes 11 I. Angiostrongylus costaricensis 11 II. Anisakis marina 12 III. Ascaris lumbricoides 14 IV. Capillaria philippinensis 21 V. Enterobius vermicularis 23 VI. Gnathostoma spinigerum 25 VII. Hookworms: Ancylostoma duodenale and Necator americanus . 26 VIII. Oesophagostoma spp 32 IX. Strongyloides stercoralis 33 X. Ternidens deminutus 34 XI. Trichinella spiralis 35 XII. Trichostrongylus spp 38 XIII. Trichuris trichiura 39 D. Trematodes 41 I. Echinostoma spp 41 II. Fasciolopsis buski 42 III. Gastrodiscoides hominis 44 IV. Heterophyes heterophyes 44 V. Metagonimus yokogawai 46 X Contents E. Cestodes 47 I. Diphyllobothrium latum 47 II. Dipylidium caninum 50 III. Hymenolepis diminuta 51 IV. Hymenolepis nana 52 V. Taenia saginata 54 VI. Taenia solium 57 VII. Cysticercosis cellulosae 58 References 60 CHAPTER 3 Epidemiology and Control of Gastrointestinal Helminths in Domestic Animals J. F. MICHEL. With 20 Figures A. Introduction 67 I. -
Study Assessing Prices, Availability and Affordability of Children's
Study assessing prices, availability and affordability of children’s medicine in Chhattisgarh, India Part of the Better Medicine for Children project Authors Dr Antony KR Virendra Jain Puni Kokho Dr Kamlesh Jain The salient findings and views expressed in this report are solely those of the authors. Please direct correspondence to the authors: ([email protected], [email protected] [email protected], [email protected]). This publication does not necessarily represent the decisions or policies of the World Health Organization. ii Contents Acknowledgements ........................................................................................... v Abbreviations ................................................................................................... vi Executive summary ......................................................................................... vii Medicine availability .............................................................................................vii Medicine costs ................................................................................................... viii Affordability of standard treatment regimens ........................................................... ix Price components survey ...................................................................................... ix Conclusion .......................................................................................................... x 1. Introduction ................................................................................................. -

WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/148799 Al 1 November 2012 (01.11.2012) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/107 (2006.01) A61K 9/00 (2006.01) kind of national protection available): AE, AG, AL, AM, A 61 47/10 (2006.0V) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, PCT/US2012/034361 HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (22) International Filing Date: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, 20 April 2012 (20.04.2012) MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/480,259 28 April 201 1 (28.04.201 1) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (71) Applicant (for all designated States except US): BOARD UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, OF REGENTS, THE UNIVERSITY OF TEXAS SYS¬ TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, TEM [US/US]; 201 West 7th St., Austin, TX 78701 (US).