Geographic Accessibility Analysis for Emergency Obstetric Care Services in Malawi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rp13110rp0v10p06b0afr0rp
Public Disclosure Authorized Government of Malawi World Bank Irrigation, Rural Livelihoods and Agriculture Development Project Public Disclosure Authorized Public Disclosure Authorized Resettlement Policy Framework Volume 1: Social Impact Assessment Final Report March 2005 Public Disclosure Authorized Ministry of Agriculture Capital City, Lilongwe 3 Irrigation, Rural Livelihoods and Agriculture Development Project Resettlement Policy Framework Volume 1: Social Impact Assessment Final Report Proponent: The Principal Secretary Ministry of Agriculture P.O. Box 30134 Capital City Lilongwe 3 Tel: (265) 1789033 (265) 1789252 Fax: (265) 1789218 (265) 1788738 Consultant: Kempton Consultancy Services Plot No. 4/354D Shire Limited Building P.O. Box 1048 Lilongwe. Malawi. Mobile: (265) 9958136 ii Table of Contents Table of Contents----------------------------------------------------------------------------------------------------------------- iii EXECUTIVE SUMMARY------------------------------------------------------------------------------------------------------- vi ACKNOWLEDGEMENTS ---------------------------------------------------------------------------------------------------- x LIST OF ACRONYMS ----------------------------------------------------------------------------------------------------------xi LIST OF TABLES ---------------------------------------------------------------------------------------------------------------xii 1.0 Introduction ------------------------------------------------------------------------------------------------------------- -
Study on Effect of Interactive Radio Instruction in Improving Ecd
STUDY ON EFFECT OF INTERACTIVE RADIO INSTRUCTION IN IMPROVING ECD 2017-FINAL REPORT (SEPT 2015 – SEPT 2017) SOF. 38000339 Table of Contents LIST OF ACRONYMS ................................................................................................................................... 2 List of Figures ............................................................................................................................................. 3 GLOSSARY ................................................................................................................................................... 4 Executive Summary ................................................................................................................................... 5 Summary of Results in the two Years .................................................................................................... 6 Conclusion ................................................................................................................................................... 7 Recommendations ..................................................................................................................................... 7 1.0 Background............................................................................................................................................ 8 2.0 Study Design ....................................................................................................................................... 10 2.1 Treatment Group ................................................................................................................................ -
Summary Report 2017
Malawi Country Oice Summary Report 2017 UNFPA in Malawi aims to promote universal access to sexual and reproductive health, realize reproductive rights, and reduce maternal mortality to accelerate progress on the agenda of the Programme of Action of the International Conference on Population and Development, to improve the lives of women, adolescents and youth, enabled by population dynamics, human rights and gender equality. Malawi Country Office Summary Report 2017 UNFPA supports programmes in thematic areas of: Sexual and Reproductive Health and Rights including Family Planning, Maternal Health, HIV and AIDS, and Fistula Population and Development Humanitarian Emergencies Gender Equality and GBV including Ending Child Marriages These are delivered by working with the Ministry of Health and Population; Ministry of Finance, Economic Planning and Development; Ministry of Labour, Youth and Manpower Development; Ministry of Gender, Children, Disability and Social Welfare among other government institutions and non-state actors. While the Government Ministries implement some of the strategic activities on policy and guidelines, most of the community and facility based interventions at the service delivery level are implemented by District Councils and local non-governmental organizations. 1 UNFPA Malawi strategically supports seven districts of Chiradzulu, Salima, Mangochi, Mchinji, Dedza, Chikhwawa and Nkhata-bay. Nkhata Bay Northern Region Central Region Southern Region Salima Mchinji Mangochi Dedza Chikhwawa Chiradzulu Impact districts -

We Will Still Live: Confronting Stigma and Discrimination
Leitner Center for International Law and Justice We Will Still Live Fordham Law School Confronting Stigma and Discrimination Against 33 West 60th Street Second Floor New York, NY 10023 Women Living with HIV/AIDS in Malawi 212.636.6862 REPORT MALAWI www.leitnercenter.org THE LEITNER CENTER We Will Still Live Confronting Stigma and Discrimination Against Women Living with HIV/AIDS in Malawi Chi Mgbako Jeanmarie Fenrich Tracy E. Higgins Associate Clinical Professor of Executive Director, Leitner Center Leitner Family Professor of Law, Fordham Law School for International Law and Justice International Human Rights, Fordham Law School Supervisor, Walter Leitner Fordham Law School International Human Rights Clinic Co-Director, Leitner Center for J.D. Fordham Law School 1998 International Law and Justice J.D. Harvard Law School 2005 J.D. Harvard Law School 1990 B.A. Columbia University 2001 B.A. Princeton University 1986 Contents Introduction 2 Acknowledgments 5 Part I Background 6 Malawi’s Obligations Under International and Domestic Law 6 International Law 6 Domestic Law 8 Women’s Vulnerability to HIV/AIDS in Malawi 8 Condoms and Negotiating Power 8 Economic Dependency 10 Violence Against Women 11 Harmful Traditional Practices 12 Commercial Sex Workers 14 Girls and Young Women 16 Male Sexuality and Denial 16 Part II Stigma and Discrimination Against Women Living with HIV/AIDS in Malawi 18 Community-Level Stigma 18 Verbal Attacks 18 Social Exclusion and Fear of Casual Transmission 19 AIDS, Sex, Morality, and Death 20 Fear of Stigma as an Impediment -

Malawi 2018-19 Draft Financial Statement
Budget Document No. 3 Government of Malawi DRAFT 2018/19 FINANCIAL STATEMENT Ministry of Finance, Economic Planning and Development P.O. Box 30049 Lilongwe ii 2018-19 Financial Statement DRAFT 2018/19 FINANCIAL STATEMENT iii 2018-19 Financial Statement iv 2018-19 Financial Statement Table of Contents Abbreviations and Acronyms .......................................................................................................................... viii 1. INTRODUCTION .......................................................................................................................................... 9 2. THE 2016/17 FISCAL YEAR PERFORMANCE.............................................................................................. 10 2.1 Revenue and Grants ......................................................................................................................... 12 2.1.1 Domestic Revenue ................................................................................................................... 12 2.1.2 Grants ....................................................................................................................................... 13 2.2 Expenditure and Net Lending .......................................................................................................... 14 2.2.1 Recurrent Expenditure ............................................................................................................. 15 2.2.2 Development Expenditures ..................................................................................................... -

Public Expenditure Review of the WASH Sector in Malawi
PUBLIC EXPENDITURE REVIEW OF THE Water, Sanitation, and Hygiene Sector of Malawi February 2020 WATER, SANITATION AND HYGIENE SECTOR MALAWI FEBRUARY 2020 i PUBLIC EXPENDITURE REVIEW © UNICEF/2016/Sebastian Rich © UNICEF/2016/Sebastian ACKNOWLEDGEMENTS Appreciation goes to all individuals and institutions that Muchabaiwa, Patrick Okuni, Nkandu David Chilombo, Alessandro contributed to the development of this PER. The Government Ramella Pezza, Kelvin Tapiwa Mutambirwa and Chimwemwe would like to thank staff from several Ministries, Departments Nyimba for the technical and logistical support. and Agencies (MDAs) who were involved in this PER. Specifically, appreciation goes to staff from the M&E Division under the The Government would also like to deeply thank the Oxford Economic Planning and Development (EP&D) of the Ministry of Policy Management (OPM) consultancy team – comprising of Finance; the Water Supplies Department under the Ministry of Nick Hall (team leader), Zach White (project manager), Tuntufye Agriculture, Irrigation and Water Development (MoAIWD); and Mwalyambwire, and Tim Cammack for providing technical the Environmental Health Department under the Ministry of support that enabled the production of this PER. Also the OPM Health and Population (MoHP). staff that worked in the background to make this exercise a success are appreciated. Sincere gratitude goes to the following Government staff – Sophie Kang’oma, Victoria Geresomo, Richard Jack Kajombo, Gringoster The analysis in this PER draws on scores of interviews with Kajomba and Stevier Kaiyatsa from the EP&D; Emma Mbalame, district staff, with a list of those interviewed or consulted Bibo Charles Yatina and Gertrude Makuti Botomani from the provided in Annex I. The Government is extremely thankful to all MoAIWD; Allone Ganizani, Holystone Kafanikhale, Samuel district for their inputs. -
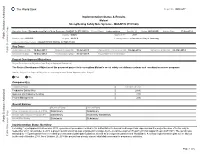
Implementation Status & Results
The World Bank Report No: ISR16677 Implementation Status & Results Malawi Strengthening Safety Nets Systems - MASAF IV (P133620) Operation Name: Strengthening Safety Nets Systems - MASAF IV (P133620) Project Stage: Implementation Seq.No: 2 Status: ARCHIVED Archive Date: 17-Nov-2014 Country: Malawi Approval FY: 2014 Public Disclosure Authorized Product Line:IBRD/IDA Region: AFRICA Lending Instrument: Investment Project Financing Implementing Agency(ies): MALAWI THIRD SOCIAL ACTION FUND Key Dates Board Approval Date 18-Dec-2013 Original Closing Date 30-Jun-2018 Planned Mid Term Review Date 30-Apr-2016 Last Archived ISR Date 03-Mar-2014 Public Disclosure Copy Effectiveness Date 16-Sep-2014 Revised Closing Date 30-Jun-2018 Actual Mid Term Review Date Project Development Objectives Project Development Objective (from Project Appraisal Document) The Project Development Objective of the proposed project is to strengthen Malawi’s social safety net delivery systems and coordination across programs. Has the Project Development Objective been changed since Board Approval of the Project? Yes No Public Disclosure Authorized Component(s) Component Name Component Cost Productive Safety Nets 28.80 Systems and Capacity Building 2.00 Project Management 2.00 Overall Ratings Previous Rating Current Rating Progress towards achievement of PDO Satisfactory Satisfactory Overall Implementation Progress (IP) Satisfactory Moderately Satisfactory Overall Risk Rating Substantial Substantial Public Disclosure Authorized Implementation Status Overview Following Project approval in December 2013, government procedures related to the authorization to borrow took longer than expected and the project became effective only in September 2014. On October 6, 2014 a project launch workshop was organized in Lilongwe by the Local Development Fund-Technical Support Team (LDF-TST). -
Malawi Newborn Health Program Final Evaluation Report
Malawi Newborn Health Program Final Evaluation Report National Level - Expanded Impact Project (with learning activities in the districts of Chitipa, Dowa, Thyolo, Mzimba, Mchinji) Cooperative Agreement No.: GHS-A-00-06-00016-00 30 September 2006 – 30 September 2011 Submitted to USAID/GH/HIDN/NUT/CSHGP December 31, 2011 by: Save the Children Federation, Inc. 54 Wilton Road, Westport, CT 06880 Telephone: (203) 221-4000 - Fax: (203) 221-4056 Contact Persons: Eric A. Swedberg, Senior Director, Child Health and Nutrition Carmen Weder, Associate Director, Department of Health & Nutrition Principal writers and editors: John Murray, External Team Leader; Karen Z. Waltensperger, Senior Advisor, Health-Africa Region; Nathalie Gamache, Associate Director, Country Support & Coordination, Saving Newborn Lives; Evelyn Zimba, Malawi Newborn Health Program Manager; Joby George, Senior Health Program Manager; Sharon Lake-Post, Editorial Consultant This report is made possible by the generous support of the American people through the United States Agency for International Development USAID). The contents are the responsibility of Save the Children and do not necessarily reflect the views of USAID or the United States Government. Page Acronyms 3 A. PRELIMINARY INFORMATION 5 B. OVERVIEW OF THE PROJECT STRUCTURE AND IMPLEMENTATION 9 C. EVALUATION ASSESSMENT METHODOLOGY AND LIMITATIONS 13 D. DATA QUALITY AND USE 14 E. PRESENTATION OF PROJECT RESULTS 17 F. DISCUSSION OF THE RESULTS 20 G. DISCUSSION OF POTENTIAL FOR SUSTAINED OUTCOMES, CONTRIBUTION TO SCALE, -

Nyau Masks, Ritual and Performance Among the Chewa of Central Malawi
Inscribing the Mask: Nyau Masks, Ritual and Performance Among the Chewa of Central Malawi Laurel Birch de Aguilar Thesis submitted for the degree of Doctor of Philosophy SCHOOL OF ORIENTAL AND AFRICAN STUDIES UNIVERSITY OF LONDON 1996 ProQuest Number: 11010550 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 11010550 Published by ProQuest LLC(2018). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 2 ABSTRACT This thesis presents an interpretation of nyau masks of the Chewa people in the central region of Malawi. Theoretically, ethnography in the thesis is informed by text interpretation as in the writings of Paul Ricoeur (1979). Texts in the thesis include the inscription of a performance, narratives of ritual events, oral discourse, and the masks themselves. Masks as texts include form, color, imagery, portraiture, construction and materials used, naming, roles, and movement; and the discourse about these. In the thesis masks are inscribed in their various roles as they are performed in funerals, initiations into the nyau society, and funeral remembrance dances. Each Chapter develops one context of masks and masking, ending with an interpretation of that context. -

Map District Site Balaka Balaka District Hospital Balaka Balaka Opd
Map District Site Balaka Balaka District Hospital Balaka Balaka Opd Health Centre Balaka Chiendausiku Health Centre Balaka Kalembo Health Centre Balaka Kankao Health Centre Balaka Kwitanda Health Centre Balaka Mbera Health Centre Balaka Namanolo Health Centre Balaka Namdumbo Health Centre Balaka Phalula Health Centre Balaka Phimbi Health Centre Balaka Utale 1 Health Centre Balaka Utale 2 Health Centre Blantyre Bangwe Health Centre Blantyre Blantyre Adventist Hospital Blantyre Blantyre City Assembly Clinic Blantyre Chavala Health Centre Blantyre Chichiri Prison Clinic Blantyre Chikowa Health Centre Blantyre Chileka Health Centre Blantyre Blantyre Chilomoni Health Centre Blantyre Chimembe Health Centre Blantyre Chirimba Health Centre Blantyre Dziwe Health Centre Blantyre Kadidi Health Centre Blantyre Limbe Health Centre Blantyre Lirangwe Health Centre Blantyre Lundu Health Centre Blantyre Macro Blantyre Blantyre Madziabango Health Centre Blantyre Makata Health Centre Lunzu Blantyre Makhetha Clinic Blantyre Masm Medi Clinic Limbe Blantyre Mdeka Health Centre Blantyre Mlambe Mission Hospital Blantyre Mpemba Health Centre Blantyre Ndirande Health Centre Blantyre Queen Elizabeth Central Hospital Blantyre South Lunzu Health Centre Blantyre Zingwangwa Health Centre Chikwawa Chapananga Health Centre Chikwawa Chikwawa District Hospital Chikwawa Chipwaila Health Centre Chikwawa Dolo Health Centre Chikwawa Kakoma Health Centre Map District Site Chikwawa Kalulu Health Centre, Chikwawa Chikwawa Makhwira Health Centre Chikwawa Mapelera Health Centre -

Master Plan Study on Rural Electrification in Malawi Final Report
No. JAPAN INTERNATIONAL COOPERATION AGENCY (JICA) MINISTRY OF NATURAL RESOURCES AND ENVIRONMENTAL AFFAIRS (MONREA) DEPARTMENT OF ENERGY AFFAIRS (DOE) REPUBLIC OF MALAWI MASTER PLAN STUDY ON RURAL ELECTRIFICATION IN MALAWI FINAL REPORT MAIN REPORT MARCH 2003 TOKYO ELECTRIC POWER SERVICES CO., LTD. MPN NOMURA RESEARCH INSTITUTE, LTD. JR 03-023 Contents 0 Executive Summary .................................................................................................................... 1 1 Background and Objectives ........................................................................................................ 4 1.1 Background ......................................................................................................................... 4 1.2 Objectives............................................................................................................................ 8 2 Process of Master Plan................................................................................................................ 9 2.1 Basic guidelines .................................................................................................................. 9 2.2 Identification of electrification sites ................................................................................. 10 2.3 Data and information collection........................................................................................ 10 2.4 Prioritization of electrification sites................................................................................. -
Inception Report
b Adapting to Climate Change Through Integrated Risk Management Strategies and Enhanced Market Opportunities for Resilient Food Security and Livelihoods Inception Report September 2020 Table of Contents List of acronyms....................................................................................................................................... ii 1. Introduction ....................................................................................................................................... 1 1.1 Purpose of the report .............................................................................................................. 1 1.2 Background to the project ..................................................................................................... 1 1.3 Target areas identification ..................................................................................................... 2 1.4 Project Objectives .................................................................................................................... 3 2. Inception Workshop Methodology and Process ..................................................................... 4 2.1 Inception workshop objectives and agenda ..................................................................... 4 2.2 Methodology and Approaches ............................................................................................. 5 3. Inception Workshop Outcomes .................................................................................................... 8 3.1