1 Drugs Are the Solution Not the Problem
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

African Journal of Drug & Alcohol Studies, 14(1), 2015 Copyright
African Journal of Drug & Alcohol Studies, 14(1), 2015 Copyright © 2015, CRISA Publications iDentifYing the coMPoSition of Street Drug NYAOPE usINg TwO Different MASS SPectroMeter MethoDS aye a. khine1, kebogile E. Mokwena2, Mempedi Huma2, lucy Fernandes2 1Department of Chemical Pathology, Medunsa/University of Limpopo, South Africa 2Department of Public Health, Medunsa/University of Limpopo, South Africa ABStrAct Criminalizaton of trading and using of street drug Nyaope has had challenges in South Africa due to controversies about its compositon. The high cost and complexity of its analysis using conventonal chromatography methods also limit the testng availability in most routne laboratories. A state of the Art method with simple specimen processing and faster turnaround tme at an afordable cost is urgently needed. To compare the ability of a new Time-of-Flight Mass Spectrometry with direct sample analysis (TOF-DSA MS) and Gas Chromatography Mass Spectrometry (GC-MS) methods in detectng the consttuents of Nyaope against turnaround tme and cost, in order to recommend a beter system for routne use. Cross-sectonal, qualitatve and descriptve pilot study on samples purchased from various sources of 12 townships in Northern Gauteng Province. The consttuents consistently detected in all samples were cafeine, drugs of abuse such as opiates, codeine, morphine, methyl-dioxy amphetamine (MDA) and heroin. Some samples contained antbiotcs (citrofex) and antretroviral drugs (zidovudine). Central nervous system (CNS) depressants such as phenobarbitone and benzodiazepines, benzitramide, moramide intermediates and thiofentanyl and stmulants such as Pipradol, and fenethyline were detected by the TOF-MS system. The usefulness of TOF-DSA MS was beter as a screening method while GC-MS provides specifcity and confrmatory detecton. -

An Exploration of the Association Between the Whoonga/Nyaope Drug And
An Exploration of the Association between the Whoonga/Nyaope Drug and Criminality through the Eyes of Convicted Drug Offenders in Three Metropolitan Cities of the Republic of South Africa by Siyanda Brightman Ngcobo Submitted in fulfilment of the requirements for the degree DOCTOR OF PHILOSOPHY IN CRIMINOLOGY AND FORENSIC STUDIES in the Discipline of Criminology and Forensic Studies School of Applied Human Sciences College of Humanities UNIVERSITY OF KWAZULU-NATAL (UKZN) Supervisor: Professor Jéan Steyn January 2019 DECLARATION I, Siyanda Brightman Ngcobo, declare that 1. The research reported in this thesis, except where otherwise indicated, and is my original research. 2. This thesis has not been submitted for any degree or examination at any other university. 3. This thesis does not contain any other persons’ data, pictures, graphs or other information, unless specifically acknowledged as being sourced from other persons. 4. This thesis does not contain any other persons’ writing, unless specifically acknowledged as being sourced from other researchers. Where other written sources have been quoted, then: a. Their words have been re-written but the general information attributed to them was referenced. b. Where their exact words have been used, then their writing has been placed in italics and inside quotation marks, and referenced. 5. This thesis does not contain text, graphics or tables copied and pasted from the Internet, unless specifically acknowledged and the source being detailed in the thesis and in the References sections. ----------------------------------------------- Siyanda Brightman Ngcobo On the 18th day of March 2019 i DEDICATION I dedicate this research project to all the Police Officers in the world; the men and women who put their lives on the line so that others may live. -

Call for a Harm-Reduction Approach to Drug-Use Disorders in South Africa
Safe treatment and treatment of safety: call for a harm-reduction approach to 19 drug-use disorders in South Africa Authors: Andrew Scheibei,ii Shaun Shellyi,iii Anna Versfeldi Simon Howelliv Monique Marksii he complex political, structural and socio-economic factors that influence drug Regulation of drug use use and corresponding responses have contributed to the increasing drug- has largely relied on the T related burden of disease in South Africa. As a result, the country’s healthcare system is called on to manage the consequences of a public-health problem that has criminal-justice system and no ‘good solutions’. the view that people who Internationally, regulation of drug use has largely relied on the criminal-justice system use drugs are ‘the problem’, and the view that people who use drugs are ‘the problem’, deserving of punishment or ‘rehabilitation’. Over the past 30 years, a number of well-resourced democratic deserving of punishment governments have acknowledged the failure of such methods. This has resulted in a or ‘rehabilitation’. Over more medicalised approach to dealing with drug use, one that views habitual drug use as a chronic disease in need of treatment. Some recent South African policy the past 30 years, a documents have called for such an approach. In practice, however, enforcement and number of well-resourced punishment remain the dominant response, with the country only paying lip service democratic governments have to the provision of harm-reduction programmes. In addition, little attention has been given to the socio-economic context that encompasses and contributes to drug use, acknowledged the failure of this despite evidence that the existing policy and practice framework has created such methods. -
DBA Inteliigence Publications Titles with Fol Exemptions Second
DBA IntelIigence Publications Titles with FOl Exemptions Second Section 1997 - 2015 As of july 25. 2015 Prod- No. Title Year 01005 (b)(7')(A) Coca Cultivation & Cocaine Base Production 2001 01015 Cultivio de Coca y Producción 2001 studies in (b)(7)(A) | 02036 2002 NPMP-142 (b)(7)(A) Marijuana Routes 2003 NPMP-142 Money Laundering Routes 2003 NPMP-142 Methamphetamine Routes 2003 NPMP-142 Pharmaceutical Routes 2003 04039 Methamphetamine and Chemical Diverson Situation! (b)7)(A) | 2004 05007 (b)(7)(A) Technical Notes, First Edition 2005 05019 |(b)(7 )Coca Yields 2005 06002 Technical Motes 2006 06019 Opium Poppy Cultivation and Heroin Production inf (b)(7)(A) 2006 NPMP-102 (b)(7)(A) | Cocaine Routes 2006 (b)(7)(A) | Cocaine Base Processing m the| (b)(7)(A) | 07022 2007 DIB-004-07 |an^ (b)(7)(A) Traffickers Expand Ties in the Methamphetamine Trade 2007 DIB-005-07 (b)(7)(A) The New Front Line in the Battle for the Border 2007 Jo t (b)(7)(A) |5tudy to Estimate Coca Leaf Yields in the| (b)(r)(A) Region of (b)(7)(A) 08014 in 2008 08024 Drug Related Deaths (b)(''HA) |Aiea of Responsibility (Unclassified) 2008 08027 (b)(7)(A) Studies to Estimate Coca Leaf Yields in the (b)(7)(A) Growing Regions of Arauca and Vichada 2008 08029 Dictionary 2008 Joint (b)(7)(A) Study to Estimate Coca Leaf Yields in he (b)(7)(A) of (b)(7)(A) 08041 t 2008 09005 (b)( 7 )(A) Study to Estimate Coca Leaf YieIds i n the (b)(7)( | Regio ns of (b)(7)(A) ] 2009 09010 Study to Estimate Coca Leaf Yields in the) (b)(7)(A) |Regian of| (b)(7)(A) | 2009 09014 (b)(7) |Heroin Assessment -
WHAT IS WHOONGA? Frequently Asked Questions?
WHAT IS WHOONGA? Whoonga, is sold as a powder that is usually mixed with dagga and smoked. It is predomi- nantly sold in Umlazi, Inanda and in areas along the North and South Coast is also known by its trade name of “Sugars” in Chatsworth, Phoenix and Wentworth. The drug Whoonga is made up of a mixture of low grade heroine and other additives like rat poison. Whoonga is highly addictive and a user can become addicted even after only using it once. The withdrawal symptoms of this drug are severe body pains, which include severe headaches, stomach pains and muscle spasms. This leads to users taking more of the drug because the heroin provides temporary ‘relief’ from the pain. Hence, users become trapped in a vicious cycle where the Whoonga both causes and (temporarily) ‘relieves’ the agonising pain. Demystifying Myths around ARV’s - Many believe that Whoonga contains anti-retroviral drugs (ARVs). This has not been conclusively proven since laboratory results have con- cluded that the active chemicals in Whoonga or “sugars” are low grade/residual heroine; cocaine and strychnine. If ARV’s are used it is merely to bulk up the product, just like the drug dealers would use vim (household cleaners); asbestos or any other available chemical or drug. Frequently Asked Questions? Question: What is substance abuse? Answer: Substance abuse is the use of a mood or behavior-altering substance resulting in significant impairment or distress. It includes the misuse of medications, alcohol or other illegal substances. This abuse can affect a person’s physical health and personal or social functioning. -
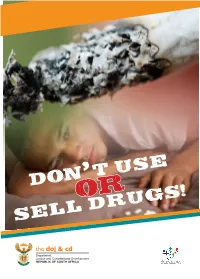
Don'''''''''''' T''''''''''''''''''' Use Sell Drugs!
, DON’’’’’’’’’’’’ T’’’’’’’’’’’’’’’’’’’ USE ]OR SELL DRUGS! 2 o not get involved in drugs. If you believe that someone else As part of the Department of cannot make choices for you, why Justice and Constitutional would you let drugs do it? DDevelopment’s work we give you information to help you NOT to buy, use, sell or deal in drugs. DRUGS OR ILLEGAL READ THIS: SUBSTANCES WILL DESTROY YOU: 1. Think about what you read here. After your first taste, you may become enslaved to drugs or 2. Speak to your friends about the become ill. information in this booklet. • YOU MAY BECOME 3. Be proud of yourself. ADDICTED. • LOSE ANY POSSIBILITY OF A VALUABLE LIFE OR ASK YOURSELF: FUTURE. 1. Do I like being FREE? • BE A BURDEN TO YOUR FAMILY, COMMUNITY AND 2. Do I enjoy the POWER to make TO YOURSELF my own decisions and decide my own future? • LOSE YOUR MIND. 3. Or do I want to be TOLD WHAT • AND YOU MAY POSSIBLY TO DO and letting others make DIE. life choices for me? Along the way you may become Well, doing drugs is like having a thief and may sell your valuable someone else make your choices possessions; become a gang for you and not checking with you if member or a habitual criminal, be you are ok with this! convicted and imprisoned. 3 YOU WILL ALSO LOSE OUT ON EDUCATION. WHAT ARE DRUGS? Drugs are any chemical substances that cause a physical, mental, emotional, or behavioural change in a person. WHAT IS DRUG ABUSE? It is the regular use of any legal or illegal chemical substance that results in physical, mental, emotional, or behavioural change in a person. -

The Effects of Whoonga on the Learning of Affected Youth in Kwa-Dabeka Township
THE EFFECTS OF WHOONGA ON THE LEARNING OF AFFECTED YOUTH IN KWA-DABEKA TOWNSHIP BY ZAMAKHOSI THINA SHEMBE Submitted in accordance with the requirements for the degree MASTER OF EDUCATION (SOCIO-EDUCATION) At the UNIVERSITY OF SOUTH AFRICA SUPERVISOR: DR VA NKONYANE SEPTEMBER 2013 i DECLARATION OF ORIGINALITY STUDENT NUMBER: 06384870 I declare that The effects of whoonga on the learning of affected youth in Kwa-Dabeka Township is my own work and that all the sources that I have used or quoted have been indicated and acknowledged by means of complete references. …………………………………… ………………………. Signature Date Zamakhosi Thina Shembe ii DEDICATION I dedicate this work to my beloved and late father, J.G. Shembe, who valued education so much, and who I know would have been so proud of me for this postgraduate degree. iii ACKNOWLEDGEMENTS I would like to extend a sincere word of gratitude to the following people for their contribution in making this study a success: My supervisor, Dr VA Nkonyane, whose invaluable guidelines took me step by step through this academic journey. He has always been encouraging, supportive and patient from the beginning to the end of this difficult and bumpy journey. Without your support and understanding, I could not have been able to complete this degree. I have learnt so much about academic writing from your clear and unambiguous guidance and mentorship. Dr. Anwar Jeewa of Minds Alive, who gave me invaluable information with regard to the composition of whoonga, affording me much needed clarity. The KZN Department of Education for allowing me to conduct my research in their school. -

Drug Use Among Youth and Adults in a Population-Based Survey in South Africa
South African Journal of Psychiatry ISSN: (Online) 2078-6786, (Print) 1608-9685 Page 1 of 6 Original Research Drug use among youth and adults in a population-based survey in South Africa Authors: Objective: Illicit drug use is a growing public health problem. The aim of the study was to 1,2 Karl Peltzer assess the prevalence of drug use and the sociodemographic and health characteristics that Nancy Phaswana-Mafuya1,3 influence it among young and adult South Africans. Affiliations: Methods: Data based on the South African national population-based survey in 2012 for 26 453 1HIV/AIDS/STIs and TB Research Programme, Human individuals (52.0% women and 48.0% men) aged 15 years and older were analysed. Past Sciences Research Council, 3-month drug use was assessed with the ‘Alcohol, Smoking and Substance use Involvement South Africa Screening Test (ASSIST)’. Bivariate and multivariable logistic regression was conducted to assess the association between sociodemographic factors, health variables and any past 2Department of Research Innovation and Development, 3-month drug use. University of Limpopo, South Results: Overall, any past 3-month drug use was 4.4%, 7.9% among men and 1.3% among Africa women. The proportion of past 3-month cannabis use was 4.0%, followed by sedatives or 3Deputy Vice Chancellor sleeping pills 0.4%, amphetamine-type stimulants 0.3%, cocaine 0.3%, opiates 0.3%, inhalants Research and Innovation 0.2% and hallucinogens 0.1%. Among the nine South African provinces, any past 3-month Office, North West University, drug use was the highest in the Western Cape (7.1%), followed by the Free State (6.3%) and South Africa Northern Cape (5.2%). -

Addiction and Dependence
ISSN:2471-061X Peter A. Clark, S.J (2019) J Addict Depend 5(1): 1-18 DOI: 10.15436/2471-061X.19.2638 Journal of Volume 5 | Issue 1 OPEN ACCESS ResearchAddiction Article and Dependence Is Medical Marijuana a Viable Option for Opioid Replacement Therapy? Peter A. Clark, S.J.*, Gabriella Mamo*, Samuel Schadt, Sonul Gulati, Arun Minupuri, John Dubensky, Archen Krupadev, Rushabh Shah, Shengnan Zheng, Jesus Salas Noain, Cameron Fick, Olivia Nguyen, Patrick Laird, Rishi Gulati, Michael Fontana, Priscilla Rodriguez, Graham Clifford, Sean McDermott, Haley Patrick, Justin Stout, Jordan Davis Institute of Clinical Bioethics, Saint Joseph’s University, 5600 City Avenue, Philadelphia, Pennsylvania, USA *Corresponding author: Peter A. Clark S.J, Director, Institute of Clinical Bioethics, Saint Joseph’s University, 5600 City Avenue, Philadel- phia, Pennsylvania, USA 19131, Tel: 610-660-3425, E-mail: [email protected] Gabriella Mamo, Philadelphia College of Osteopathic Medicine, 4170 City Avenue, Philadelphia, Pennsylvania, USA 19131; E-mail: gm270930@ pcom.edu Abstract The opioid epidemic has become one of the most serious health crises in the United States. Current replacement ther- apies for opioid use disorder, such as methadone, buprenorphine, and naltrexone, are not sufficient enough to treat recovering opioid users due to disadvantages such as inadequate availability and potential side effects. As a result, new alternatives to these drugs must be addressed. This article addresses the permissibility of using medical marijuana as a potential replacement therapy for Opioid Use Disorder and opioid withdrawal from the pharmacological, medical, legal, and ethical perspectives. Pharmacologically, current replacement therapies are used to decrease the symptoms of with- drawal and lower the risk of overdose but have several limitations. -

At What Cost? the Futility of the War on Drugs in South Africa
At what cost? The futility of the war on drugs in South Africa Quintin van Kerken, Anti Drug Alliance SA Quintin van Kerken, Anti Drug Alliance SA At what cost? The futility of the war on drugs in South Africa Introduction In February 2011, an article by Dr. JP van Niekerk in the South African Medical Journal spoke of the legalisation of drugs. Dr. Van Niekerk wrote: “The war on drugs has failed! Humans have always taken psychoactive substances and prohibition has never kept them from doing so. The international evidence suggests that drug policy has very limited impact on the overall level of drug use. Making people criminals for taking psychoactive substances is in itself criminal, for one is dealing with, at worst, a vice but not a crime.” (February 2011, Vol. 101, No. 2 SAMJ, Page 2) The article hit a nerve. Up until that stage, legalisation had only been spoken of by fringe groups, and their argument always took the religious (Rastafarianism) approach, or was an uneducated and biased approach to legalisation. This was one of the first articles of its kind by a well-respected, well-known and well educated South African gentleman, who spoke from a completely scientific point of view. However, my position as Chief Executive Officer of the Anti Drug Alliance of South Africa made it difficult to accept the article. After all, we (the Anti Drug Alliance) took a firm stand against drugs and addiction, and the name of the organisation clearly spelt out our purpose. Yet it was the science behind the thought process that made sense. -

Guidelines for the Management of Psychoactive Substance Intoxication
Guidelines for the Management of Psychoactive Substance Intoxication & Withdrawal in Kwa Zulu Natal Table of Contents 1. General Information 2. Where & by whom should intoxication and withdrawal be damaged 3. Guidelines for outpatients/community withdrawals 4. Screening for substance abuse/ dependence 5. Recommended Interventions 6. Brief interventions 7. What if the client refuses help? 8. General Principals for detoxification 9. Flow diagram of referral pathways 10. How to manage Clients with Alcohol problems 11. How to manage Cannabis problems 12. How to manage Mandrax problems 13. How to manage Opioid problems 14. How to manage Stimulant problems - Cocaine - Amphetamines (including Tik) 15. How to manage Ecstasy problems 16. How to manage Hallucinogen problems 17. How to manage Volatile Substance (inhalant) 18. How to manage Benzodiazepine problems Detoxification protocols for children and adolescents with substance use disorders 19. Alcohol 20. Cannabis/ Cannabis & Mandrax 21. Opioids 22. Benzodiazepines 23. Hallucinogens 24. Volatile solvents 25. Nicotine 26. Useful phone numbers Page 2 MANAGEMENT OF SUBSTANCE USE DISORDERS (SUD): General information: The treatment of SUD begins with the medical stabilisation of the patient (dealing with intoxication, withdrawal and medical complications). Medical stabilisation is however not a sufficient intervention to ensure future sobriety. It needs to be followed by an intervention to prevent relapse back to substance use. Brief interventions may be used in cases of misuse or abuse. (See brief interventions below) Patients who fulfil criteria for dependence need a referral to a specialist addiction treatment service. This does not “cure” the patient, but provide tools and the support necessary to maintain sobriety. Relapses and lapses (short periods of relapse) may still happen and should be viewed as a learning opportunity. -

Efavirenz As a Psychotropic Drug
European Review for Medical and Pharmacological Sciences 2020; 24: 10729-10735 Efavirenz as a psychotropic drug N. ZAREIFOPOULOS1, M. LAGADINOU1, A. KARELA1, F. POULIASI1, I. ECONOMOU1, A. TSIGKOU2, D. VELISSARIS1,3 1Emergency Department, University Hospital of Patras, Patras, Greece 2Department of Architecture, University of Patras, Patras, Greece 3Department of Internal Medicine, University of Patras School of Medicine, Patras, Greece Abstract. – OBJECTIVE: Antiretroviral drugs Introduction are the mainstay of treatment for human immu- nodeficiency virus (HIV) infection. Lifelong high- Neuropsychiatric adverse effects are a common ly active antiretroviral therapy (HAART) is in- occurrence in daily clinical practice, and they are dicated to prevent disease progression to ac- quired immunodeficiency syndrome (AIDS). Efa- frequently observed even during treatment with virenz was a first-line component of HAART drugs that would not be expected to affect the ner- across the world for many years. The purpose vous system. Antimicrobial agents have been asso- of this article is to review the psychotropic prop- ciated with neuropsychiatric adverse effects which erties of efavirenz, which are the most import- may be severe, but this rarely affects prescribing ant adverse events associated with the drug and practices and guidelines1. This is to be expected as commonly result in treatment discontinuation. MATERIALS AND METHODS: A PubMed infectious diseases are life-threatening, whereas search was conducted using efavirenz as a the typically reversible psychotropic side effects search term, which returned 4655 results. Titles of antimicrobial agents are not; and the drugs in- and abstracts of articles were screened for rele- dicated are extremely effective, perhaps more so vance, and all relevant articles published in En- than any other class of drugs for its specific indi- glish were included in the narrative review.