Blood Glucose Self-Monitoring in Type 1 and Type 2 Diabetes: Reaching a Multidisciplinary Consensus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Continuous Glucose Monitoring on Hypoglycemia in Type 1 Diabetes
Clinical Care/Education/Nutrition/Psychosocial Research ORIGINALDiabetes ARTICLE Care Publish Ahead of Print, published online February 19, 2011 Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes 1 2 TADEJ BATTELINO, MD, PHD REVITAL NIMRI, MD especially useful in patients with hypogly- 2 3 MOSHE PHILLIP, MD PER OSKARSSON, MD, PHD 1 3 cemia unawareness and/or frequent epi- NATASA BRATINA, MD, PHD JAN BOLINDER, MD, PHD sodes of hypoglycemia (18). However, the hypoglycemia preventive effect of con- tinuous glucose monitoring has not been — OBJECTIVE To assess the impact of continuous glucose monitoring on hypoglycemia in established. Therefore, we designed a ran- people with type 1 diabetes. domized, controlled, multicenter clinical RESEARCH DESIGN AND METHODS—In this randomized, controlled, multicenter trial to evaluate the effect of continuous study, 120 children and adults on intensive therapy for type 1 diabetes and a screening level of glucose monitoring on hypoglycemia in glycated HbA1c ,7.5% were randomly assigned to a control group performing conventional children and adults with type 1 diabetes. home monitoring with a blood glucose meter and wearing a masked continuous glucose monitor every second week for five days or to a group with real-time continuous glucose monitoring. The primary outcome was the time spent in hypoglycemia (interstitial glucose concentration ,63 RESEARCH DESIGN AND mg/dL) over a period of 26 weeks. Analysis was by intention to treat for all randomized patients. METHODS RESULTS—The time per day spent in hypoglycemia was significantly shorter in the contin- uous monitoring group than in the control group (mean 6 SD 0.48 6 0.57 and 0.97 6 1.55 Patients Patients aged between 10 and 65 years h/day, respectively; ratio of means 0.49; 95% CI 0.26–0.76; P = 0.03). -

Blood Glucose Monitoring in Type 1 Diabetes (Adults)
FACTSHEET | JUNE 2021 Blood Glucose Monitoring in type 1 diabetes (adults) RSS Diabetes Service Blood glucose goes up and down during the day depending on carbohydrate intake, physical activity, insulin doses, wellbeing and stressors. Blood glucose results tend to be lower before meals and higher after meals. Blood glucose monitoring guides your self-care. The first step in blood glucose monitoring is knowing your blood glucose target ranges. What are the recommended blood glucose (BG) targets For most people with type 1 diabetes, it is recommended that blood glucose be as close to normal as possible to reduce the risk of long term complications. In general, recommended blood glucose targets are: Time Target BG Fasting and before meals 4.0 – 8.0mmol/L 2 hours after meals 4.0 – 10.0mmol/L However, for some people (e.g. infants and young children, the aged, those with impaired hypoglycaemia awareness or other health conditions), blood glucose targets will need to be set higher. If you are pregnant or trying to get pregnant, your blood glucose targets will be set lower. When should I test my blood glucose (BG)? Your blood glucose levels will indicate if your diabetes is well managed or if changes are needed. Blood glucose results overnight or before breakfast tell you how well your diabetes is controlled overnight by the basal insulin. Blood glucose results before lunch, before the evening meal and at bedtime tell you if your meal time rapid acting insulin doses are correct. Extra tests are recommended if you: • feel unwell, as part of your sick day action plan • are planning some physical activity, during and after physical activity • are using machinery • are about to drive • are concerned about unstable, unexpected or unexplainable results. -

Blood Glucose Monitoring
Blood Glucose Monitoring Many people are frightened to check their blood sugar levels because they do not want to see levels that are higher or lower than their target range. However, checking your blood sugars puts you in control of your diabetes. Remember, your blood sugar levels are what they are whether you know about them or not but when you know what they are; you can make adjustments, if needed. Monitoring your blood sugar levels is the most accurate way of you seeing the effectiveness of your lifestyle changes and medications. Monitoring provides you with the ability to identify possible causes of blood sugar fluctuations. Tips for Monitoring • Wash your hands with soap in warm water before checking your blood sugar • Ensure your test strips have not expired • Remember to calibrate your meter (if your meter requires this) • Use the sides of your fingers and remember to use different fingers o Do not use alternate site testing if you think your blood sugar is very high or low – finger checks give you the most accurate result • Discuss the with your healthcare team the best times to check your blood sugar level – which may include: o Prior to your meal and / or 2 hours after the meal o Overnight o If you feel unwell • Record your results in a logbook; this will help you to identify patterns in your levels and make the required changes to get your blood sugar back to your target range; bring your blood sugar records and meter(s) to your healthcare visit - it will help you and your healthcare team to determine your diabetes management needs. -

Flash Glucose Monitoring
Flash Glucose Monitoring Flash glucose monitoring is a method of glucose testing that measures, displays, and continuously stores glucose readings that are recorded automatically. It can be used by adults to make diabetes treatment decisions, including insulin dosing, without obtaining a blood sample from the fingertip (finger prick). This has the potential to improve blood sugar control and quality of life for people with type 1 or type 2 diabetes, resulting in physical, social, and emotional benefits. A flash glucose monitoring system uses an externally- touchscreen reader device, it transmits the real- worn glucose sensor with a small filament inserted time glucose reading and information on the most under the skin of a person’s upper arm. When recent 8-hour trend to the reader. If the person with the sensor is “flashed” or scanned with a separate diabetes performs at least 3 sensor scans per day diabetes.ca 1-800-BANTING (226-8464) at approximately 8-hour intervals, the flash glucose monitor can record 24-hour glucose profiles. A sensor can be worn continuously for up to 14 days. Blood glucose monitoring gives people living with diabetes a more complete picture of their glucose control, which can lead to better short and long-term treatment decisions and health outcomes. It can help them identify when their blood sugar is trending down, which allows for appropriate and timely action to be taken to avoid hypoglycemia (low blood sugar). It can also provide early indication of hyperglycemia (high blood sugar) over the course of the day and prompt adjustments to medications, activity, and food intake to help achieve blood sugar targets. -
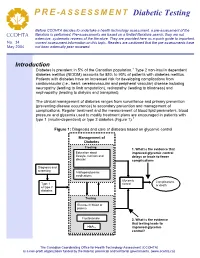
Diabetic Testing
PRE -ASSESSMENT Diabetic Testing Before CCOHTA decides to undertake a health technology assessment, a pre-assessment of the literature is performed. Pre-assessments are based on a limited literature search; they are not CCOHTA extensive, systematic reviews of the literature. They are provided here as a quick guide to important, No. 34 current assessment information on this topic. Readers are cautioned that the pre-assessments have May 2004 not been externally peer reviewed. Introduction Diabetes is prevalent in 5% of the Canadian population.1 Type 2 non-insulin dependent diabetes mellitus (NIDDM) accounts for 85% to 90% of patients with diabetes mellitus. Patients with diabetes have an increased risk for developing complications from cardiovascular (i.e., heart, cerebrovascular and peripheral vascular) disease including neuropathy (leading to limb amputation), retinopathy (leading to blindness) and nephropathy (leading to dialysis and transplant). The clinical management of diabetes ranges from surveillance and primary prevention (preventing disease occurrence) to secondary prevention and management of complications. Regular treatment and the measurement of blood lipid parameters, blood pressure and glycemia used to modify treatment plans are encouraged in patients with type 1 (insulin-dependent) or type 2 diabetes (Figure 1).1 Figure 1: Diagnosis and care of diabetes based on glycemic control Management of Diabetes Treating:Treating 1. What is the evidence that LifestyleEducation –about physical improved glycemic control nutritional,lifestyle, nutrition and and delays or leads to fewer disease knowledge complications education Diagnosis and and screening screening AntihyperglycemicAntihyperglycemic medications Glycemic Complications Type 1 control Type 1 or death or typetype 2 2 diabetes diabetes Testing:Testing GlucoseFasting in bloodplasma or plasmaglucose Fructosamine 2. -

Clinical Usefulness of the Measurement of Serum Fructosamine in Childhood Diabetes Mellitus
Original article http://dx.doi.org/10.6065/apem.2015.20.1.21 Ann Pediatr Endocrinol Metab 2015;20:21-26 Clinical usefulness of the measurement of serum fructosamine in childhood diabetes mellitus Dong Soo Kang, MD1, Purpose: Glycosylated hemoglobin (HbA1c) is often used as an indicator of glucose Jiyun Park, MD1, control. It usually reflects the average glucose levels over two to three months, and Jae Kyung Kim, PhD2, is correlated with the development of long-term diabetic complications. However, Jeesuk Yu, MD, PhD1 it can vary in cases of hemoglobinopathy or an altered red blood cell lifespan. The serum fructosamine levels reflect the mean glucose levels over two to three weeks. 1 This study was designed to determine the clinical usefulness of the combined Departments of Pediatrics and 2Laboratory Medicine, Dankook measurement of serum fructosamine and HbA1c in the management of childhood University Hospital, Dankook diabetes mellitus and the correlation between them. University College of Medicine, Methods: Clinical data on 74 Korean children and adolescents with diabetes Cheonan, Korea mellitus who were under management at the Department of Pediatrics of Dankook University Hospital were evaluated. Their fructosamine and HbA1c levels were reviewed based on clinical information, and analyzed using IBM SPSS Statistics ver. 21. Results: Their HbA1c levels showed a strong correlation with their fructosamine levels (r=0.868, P<0.001). The fructosamine level was useful for the prompt evaluation of the recent therapeutic efficacy after the change in therapeutic modality. It was also profitable in determining the initial therapeutics and for the estimation of the onset of the disease, such as fulminant diabetes. -
Continuous Glucose Monitoring and Insulin Delivery for Managing Diabetes
UnitedHealthcare® Commercial Medical Policy Continuous Glucose Monitoring and Insulin Delivery for Managing Diabetes Policy Number: 2021T0347GG Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policy Coverage Rationale ....................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Documentation Requirements ...................................................... 2 Supplies and Repairs/Replacements Applicable Codes .......................................................................... 2 Description of Services ................................................................. 6 Community Plan Policy Benefit Considerations .................................................................. 7 • Continuous Glucose Monitoring and Insulin Delivery for Managing Diabetes Clinical Evidence ........................................................................... 7 U.S. Food and Drug Administration ........................................... 13 Medicare Advantage Coverage Summary References ................................................................................... 14 • Diabetes Management, Equipment and Supplies Policy History/Revision Information ........................................... 16 Instructions for Use ..................................................................... 16 Coverage Rationale See Benefit Considerations Insulin Delivery External insulin pumps that deliver insulin by continuous subcutaneous infusion are -

Type 2 Diabetes Screening and Treatment Guideline | Kaiser
Type 2 Diabetes Screening and Treatment Guideline Interim Update September 2021 .................................................................................................................. 2 Changes as of March 2021 .......................................................................................................................... 2 Prevention .................................................................................................................................................... 2 Screening and Tests .................................................................................................................................... 2 Diagnosis...................................................................................................................................................... 3 Treatment ..................................................................................................................................................... 4 Risk-reduction goals ................................................................................................................................ 4 Lifestyle modifications and non-pharmacologic options ......................................................................... 4 Bariatric surgery ...................................................................................................................................... 5 Pharmacologic options for glucose control ............................................................................................ -

(Hba1c) in the Diagnosis of Diabetes Mellitus
WHO/NMH/CHP/CPM/11.1 Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus Abbreviated Report of a WHO Consultation © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected] ). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected] ). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

Frequency of Blood Glucose Monitoring in Relation to Glycemic Control in Patients with Type 2 Diabetes
Clinical Care/Education/Nutrition ORIGINAL ARTICLE Frequency of Blood Glucose Monitoring in Relation to Glycemic Control in Patients With Type 2 Diabetes MAUREEN I. HARRIS, PHD, MPH glucose level, measured as HbA1c, and the frequency of self-monitoring in a nation- wide sample of patients with type 2 dia- betes. OBJECTIVE — The aim of the study was to investigate the relationship between blood glu- RESEARCH DESIGN AND cose level, measured as HbA1c, and frequency of self-monitoring in patients with type 2 diabetes. METHODS — Data were analyzed Daily self-monitoring is believed to be important for patients treated with insulin or oral agents from the third National Health and Nutri- to detect asymptomatic hypoglycemia and to guide patient and provider behavior toward reach- tion Examination Survey (NHANES III), ing blood glucose goals. in which questionnaire, clinical, and lab- RESEARCH DESIGN AND METHODS — A national sample of patients with type 2 oratory data were obtained for a repre- diabetes was studied in the third National Health and Nutrition Examination Survey. Data on sentative sample of adults with type 2 therapy for diabetes, frequency of self-monitoring of blood glucose, and HbA1c values were diabetes. NHANES III was conducted obtained by structured questionnaires and by clinical and laboratory assessments. from September 1988 to October 1994 and included a stratified probability sam- RESULTS — According to the data, 29% of patients treated with insulin, 65% treated with ple of the civilian noninstitutionalized oral agents, and 80% treated with diet alone had never monitored their blood glucose or U.S. population (2). Participants were in- monitored it less than once per month. -

Forecasting of Glucose Levels and Hypoglycemic Events
sensors Article Forecasting of Glucose Levels and Hypoglycemic Events: Head-to-Head Comparison of Linear and Nonlinear Data-Driven Algorithms Based on Continuous Glucose Monitoring Data Only Francesco Prendin, Simone Del Favero * , Martina Vettoretti, Giovanni Sparacino and Andrea Facchinetti Department of Information Engineering, University of Padova, 35131 Padova, Italy; [email protected] (F.P.); [email protected] (M.V.); [email protected] (G.S.); [email protected] (A.F.) * Correspondence: [email protected] Abstract: In type 1 diabetes management, the availability of algorithms capable of accurately forecasting future blood glucose (BG) concentrations and hypoglycemic episodes could enable proactive therapeutic actions, e.g., the consumption of carbohydrates to mitigate, or even avoid, an impending critical event. The only input of this kind of algorithm is often continuous glucose monitoring (CGM) sensor data, because other signals (such as injected insulin, ingested carbs, and physical activity) are frequently unavailable. Several predictive algorithms fed by CGM data only have been proposed in the literature, but they were assessed using datasets originated by different Citation: Prendin, F.; Del Favero, S.; experimental protocols, making a comparison of their relative merits difficult. The aim of the Vettoretti, M.; Sparacino, G.; present work was to perform a head-to-head comparison of thirty different linear and nonlinear Facchinetti, A. Forecasting of Glucose predictive algorithms using the same dataset, given -

Continuous Glucose Monitoring Roadmap for 21St Century Diabetes Therapy
Reviews/Commentaries/ADA Statements REVIEW ARTICLE Continuous Glucose Monitoring Roadmap for 21st century diabetes therapy DAVID C. KLONOFF, MD, FACP toring System Gold (CGMS Gold; Medtronic MiniMed, Northridge, CA) (1), the GlucoWatch G2 Biographer (GW2B; Cygnus, Redwood City, CA) (2), ontinuous glucose monitoring pro- era, on the other hand, takes multiple, the Guardian Telemetered Glucose Mon- vides maximal information about poorly focused frames; displays a sequen- itoring System (Medtronic MiniMed) (3), C shifting blood glucose levels tial array of frames whose trend predicts the GlucoDay (A. Menarini Diagnostics, throughout the day and facilitates the the future; produces too much informa- Florence, Italy) (4), and the Pendra (Pen- making of optimal treatment decisions for tion for each frame to be studied carefully; dragon Medical, Zurich, Switzerland) (5). the diabetic patient. This report discusses and operates automatically after it is A sixth monitor, whose premarket ap- continuous glucose monitoring in terms turned on. The two types of blood glucose proval application has been submitted to of its purposes, technologies, target pop- monitors differ in much the same way: 1) the FDA, is the FreeStyle Navigator Con- ulations, accuracy, clinical indications, an intermittent blood glucose monitor tinuous Glucose Monitor (Abbott Labora- outcomes, and problems. In this context, measures discrete glucose levels ex- tories, Alameda, CA) (6). the medical literature on continuous glu- tremely accurately, whereas a continuous The currently