Comparison of the Effects of Telmisartan and Olmesartan On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Stimulatory Action of Telmisartan, an Antagonist of Angiotensin II Receptor, on Voltage-Gated Na+ Current: Experimental and Theoretical Studies
Chinese Journal of Physiology 61(1): 1-13, 2018 1 DOI: 10.4077/CJP.2018.BAG516 Stimulatory Action of Telmisartan, an Antagonist of Angiotensin II Receptor, on Voltage-Gated Na+ Current: Experimental and Theoretical Studies Tzu-Tung Chang, Chia-Jung Yang, Yu-Chi Lee, and Sheng-Nan Wu Department of Physiology, National Cheng Kung University Medical College, Tainan 70101, Taiwan, Republic of China Abstract Telmisartan (Tel) is recognized as a non-peptide blocker of AT1R. Whether this agent has any direct effects on ion currents remains unexplored. In whole-cell current recordings, addition of Tel + increased the peak amplitude of voltage-gated Na (NaV) current (INa) accompanied by the increased time constant of INa inactivation in differentiated NSC-34 motor neuron-like cells. Tel-stimulated INa in these cells is unlinked to either blockade of AT1R or activation of peroxisome proliferator-activated receptor gamma (PPAR-γ). In order to explore how this compound affects the amplitude and kinetics of INa in neurons, a Hodgkin-Huxley-based (HH-based) model designed to mimic effect of Tel on the functional activities of neurons was computationally created in this study. In this framework, the parameter for h inactivation gating variable, which was changed in a stepwise fashion, was implemented + + to predict changes in membrane potentials (V) as a function of maximal Na (GNa), K conductance (GK), or both. As inactivation time course of INa was increased, the bifurcation point of V versus GNa became lower, and the range between subcritical and supercritical values at the bifurcation of V versus GK correspondingly became larger. -

BENICAR HCT Tablets
® BENICAR HCT Tablets (OLMESARTAN MEDOXOMIL-HYDROCHLOROTHIAZIDE) WARNING: FETAL TOXICITY When pregnancy is detected, discontinue Benicar HCT as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. See Warnings: Fetal Toxicity DESCRIPTION BENICAR HCT® (olmesartan medoxomil-hydrochlorothiazide) is a combination of an angiotensin II receptor antagonist (AT1 subtype), olmesartan medoxomil, and a thiazide diuretic, hydrochlorothiazide (HCTZ). Olmesartan medoxomil, a prodrug, is hydrolyzed to olmesartan during absorption from the gastrointestinal tract. Olmesartan medoxomil is 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2 propyl-1-[p-(o-1H-tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3 carbonate. Its empirical formula is C29H30N6O6 and its structural formula is: Olmesartan medoxomil is a white to light yellowish-white powder or crystalline powder with a molecular weight of 558.6. It is practically insoluble in water and sparingly soluble in methanol. Hydrochlorothiazide is 6-chloro-3,4-dihydro-2H-1,2,4-benzo-thiadiazine-7-sulfonamide 1,1-dioxide. Its empirical formula is C7H8ClN3O4S2 and its structural formula is: 1 Reference ID: 3227549 Hydrochlorothiazide is a white, or practically white, crystalline powder with a molecular weight of 297.7. Hydrochlorothiazide is slightly soluble in water but freely soluble in sodium hydroxide solution. BENICAR HCT® is available for oral administration in tablets containing 20 mg or 40 mg of olmesartan medoxomil combined with 12.5 mg of hydrochlorothiazide, or 40 mg of olmesartan medoxomil combined with 25 mg of hydrochlorothiazide. Inactive ingredients include: hydroxypropylcellulose, hypromellose, lactose, low-substituted hydroxypropylcellulose, magnesium stearate, microcrystalline cellulose, red iron oxide, talc, titanium dioxide and yellow iron oxide. -

Effects of Olmesartan Vs Irbesartan on Metabolic Parameters and Visfatin in Hypertensive Obese Women
European Review for Medical and Pharmacological Sciences 2010; 14: 759-763 Effects of olmesartan vs irbesartan on metabolic parameters and visfatin in hypertensive obese women D.A. DE LUIS, R. CONDE, M. GONZALEZ SAGRADO, R. ALLER, O. IZAOLA, J.L. PEREZ CASTRILLON, E. ROMERO, M.J. CASTRO Institute of Endocrinology and Nutrition, Medicine School and Unit of Investigation. Hospital Rio Hortega. RD-056/0013 RETICEF. University of Valladolid. Valladolid (Spain) Abstract. – Background: Angiotensin II reg- dence of this rising tide of obesity and associated ulates the production of adipokines. The objective pathologies has led, in the last years, to a dramat- was to study the effect of treatment with irbesartan versus olmesartan in obese hypertensive women. ic increase of researches on the role of adipose Subjects: A sample of 34 obese hypertensive tissue as an active participant in controlling the women was analyzed in a prospective way with a body’s physiology2. randomized trial. Patients were randomized to irbe- Visfatin was recently identified as a protein sartan (300 mg/day) or olmesartan (40 mg/day) for preferentially expressed in visceral adipose tis- 3 months. Weight, body mass index, blood pres- sue, compared with subcutaneous adipose tis- sure, basal glucose, insulin, total cholesterol, LDL- sue3. It can be found in skeletal muscle, liver, cholesterol, HDL-cholesterol, triglycerides, HOMA and visfatin were determined at basal time and af- bone marrow and lymphocytes, where it was ter 3 months of treatment. initially identified as pre-B-cell colony-enhanc- Results: Thirty four patients gave informed con- ing factor (PBEF). Fukuhara et al4 clearly sug- sent and were enrolled in the study. -

TWYNSTA (Telmisartan/Amlodipine) Tablets Are Indicated for the Treatment of Hypertension, Alone Or with Other Antihypertensive Agents
HIGHLIGHTS OF PRESCRIBING INFORMATION ---------------------DOSAGE FORMS AND STRENGTHS---------------------- These highlights do not include all the information needed to use • Tablets: 40/5 mg, 40/10 mg, 80/5 mg, 80/10 mg (3) TWYNSTA safely and effectively. See full prescribing information for TWYNSTA. -------------------------------CONTRAINDICATIONS------------------------------ • None TWYNSTA® (telmisartan/amlodipine) Tablets Initial U.S. Approval: 2009 -----------------------WARNINGS AND PRECAUTIONS------------------------ • Avoid fetal or neonatal exposure (5.1) WARNING: AVOID USE IN PREGNANCY • Hypotension: Correct any volume or salt depletion before initiating See full prescribing information for complete boxed warning. therapy. Observe for signs and symptoms of hypotension. (5.2) When pregnancy is detected, discontinue TWYNSTA as soon as possible. • Titrate slowly in patients with hepatic (5.4) or severe renal impairment Drugs that act directly on the renin-angiotensin system can cause injury (5.5) and even death to the developing fetus (5.1) • Heart failure: Monitor for worsening (5.8) • Avoid concomitant use of an ACE inhibitor and angiotensin receptor ----------------------------INDICATIONS AND USAGE--------------------------- blocker (5.6) • TWYNSTA is an angiotensin II receptor blocker (ARB) and a • Myocardial infarction: Uncommonly, initiating a CCB in patients with dihydropyridine calcium channel blocker (DHP-CCB) combination severe obstructive coronary artery disease may precipitate myocardial product indicated for the treatment -
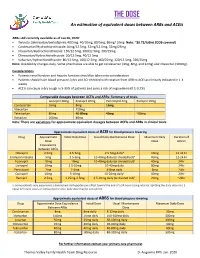
THE DOSE an Estimation of Equivalent Doses Between Arbs and Aceis
THE DOSE An estimation of equivalent doses between ARBs and ACEIs ARBs still currently available as of Jan 26, 2020: Twynsta (telmisartan/amlodipine): 40/5mg. 40/10mg, 80/5mg, 80mg/ 10mg Note: ~$0.73/tablet (ODB covered) Candesartan/Hydrochlorothiazide:16mg/12.5mg, 32mg/12.5mg, 32mg/25mg Irbesartan/Hydrochlorothiazide: 150/12.5mg, 300/12.5mg, 300/25mg Olmesartan/Hydrochlorothiaizde: 20/12.5mg, 40/12.5mg Valsartan/Hydrochlorothiazide: 80/12.5mg, 160/12.5mg, 160/25mg, 320/12.5mg, 320/25mg Note: Availability changes daily. Some pharmacies are able to get candesartan (4mg, 8mg, and 32mg) and irbesartan (300mg). Considerations Patients renal function and hepatic function should be taken into consideration Patients should have blood pressure, lytes and SCr checked with rotation from ARB to ACEI as clinically indicated in 1-4 weeks ACEIs can cause a dry cough in 5-35% of patients and carry a risk of angioedema (0.1-0.2%) Comparable dosages between ACEIs and ARBs- Summary of trials Lisinopril 20mg Enalapril 20mg Perindopril 4mg Ramipril 10mg Candesartan 16mg 8mg 16mg Irbesartan 150mg Telmisartan 80mg 40-80mg 40mg ~80mg Valsartan 160mg 80mg Note: There are variations for approximate equivalent dosages between ACEIs and ARBs in clinical trials. Approximate equivalent doses of ACEI for blood pressure lowering Drug Approximate Initial Daily Dose Usual Daily Maintenance Dose Maximum Daily Duration of Dose Dose Action Equivalence Between ACEIs Cilazapril 2.5mg 2.5-5mg 2.5-5mg dailya 10mg 12-24 hr Enalapril maleate 5mg 2.5-5mg 10-40mg daily (or divided bid)a 40mg 12-24 hr Fosinopril 10mg 10mg 10-40mg daily (or divided bid)a 40mg 24hr Lisinopril 10mg 2.5-10mg 10-40mg daily 80mg 24hr Perindopril 2mg 2-4mg 4-8mg daily 8mg 24hr Quinapril 10mg 5-10mg 10-20mg dailya 40mg 24hr Ramipril 2.5mg 1.25mg-2.5mg 2.5-10mg daily (or divided bid)a 20mg ~24hr a: Some patients may experience a diminished antihypertensive effect toward the end of a 24-hour dosing interval. -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

Importance of Hepatic Transporters, Including Basolateral Efflux Proteins, in Drug Disposition: Impact of Phospholipidosis and Non-Alcoholic Steatohepatitis
IMPORTANCE OF HEPATIC TRANSPORTERS, INCLUDING BASOLATERAL EFFLUX PROTEINS, IN DRUG DISPOSITION: IMPACT OF PHOSPHOLIPIDOSIS AND NON-ALCOHOLIC STEATOHEPATITIS Brian C. Ferslew A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Pharmaceutical Sciences in the UNC Eshelman School of Pharmacy Chapel Hill 2014 Approved by: Dhiren Thakker Mary F. Paine A. Sidney Barritt Kim L.R. Brouwer Jo Ellen Rodgers Wei Jia ©2014 Brian C. Ferslew ALL RIGHTS RESERVED ii ABSTRACT Brian C. Ferslew: Importance of Hepatic Transporters, Including Basolateral Efflux Proteins, in Drug Disposition: Impact of Phospholipidosis and Non-Alcoholic Steatohepatitis (Under the direction of Kim L.R. Brouwer) The objective of this dissertation project was to develop preclinical and clinical tools to assess the impact of liver pathology on transporter-mediated systemic and hepatic exposure to medications. A translational approach utilizing established pre-clinical hepatic transport systems, mathematical modeling, and a pivotal in vivo human study was employed. A novel application of rat sandwich-cultured hepatocytes (SCH) was developed to evaluate the impact of drug-induced phospholipidosis on the vectorial transport of probe substrates for hepatic basolateral and canalicular transport proteins. Results indicated that rat SCH treated with prototypical hepatic phospholipidosis inducers are a sensitive and selective model for drug-induced phospholipidosis; both organic anion transporting polypeptide-mediated uptake and bile salt export pump-mediated biliary excretion were reduced after the onset of phospholipidosis. Enalapril currently is being investigated for its anti-fibrotic effects in the treatment of patients with non-alcoholic steatohepatitis (NASH). -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -

Telmisartan Teva, INN-Telmisartan
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Telmisartan Teva 20 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 20 mg telmisartan Excipients: Each tablet contains 21.4 mg sorbitol (E420) For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet White to off white, oval shaped tablet; one side of the tablet is debossed with the number "93". The other side of the tablet is debossed with the number "7458". 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of essential hypertension in adults. 4.2 Posology and method of administration The usually effective dose is 40 mg once daily. Some patients may already benefit at a daily dose of 20 mg. In cases where the target blood pressure is not achieved, the dose of telmisartan can be increased to a maximum of 80 mg once daily. Alternatively, telmisartan may be used in combination with thiazide-type diuretics such as hydrochlorothiazide, which has been shown to have an additive blood pressure lowering effect with telmisartan. When considering raising the dose, it must be borne in mind that the maximum antihypertensive effect is generally attained four to eight weeks after the start of treatment (see section 5.1). Telmisartan may be taken with or without food. Renal impairment No posology adjustment is required for patients with mild to moderate renal impairment. Limited experience is available in patients with severe renal impairment or haemodialysis. A lower starting dose of 20 mg is recommended in these patients (see section 4.4). Hepatic impairment In patients with mild to moderate hepatic impairment, the posology should not exceed 40 mg once daily (see section 4.4). -

Olmesartan Medoxomil 10 Mg Film-Coated Tablets Olmesartan Medoxomil 20 Mg Film-Coated Tablets Olmesartan Medoxomil 40 Mg Film-Coated Tablets Olmesartan Medoxomil
Package leaflet: Information for the user Olmesartan medoxomil 10 mg Film-coated Tablets Olmesartan medoxomil 20 mg Film-coated Tablets Olmesartan medoxomil 40 mg Film-coated Tablets olmesartan medoxomil Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Olmesartan medoxomil is and what it is used for 2. What you need to know before you take Olmesartan medoxomil 3. How to take Olmesartan medoxomil 4. Possible side effects 5. How to store Olmesartan medoxomil 6. Contents of the pack and other information 1. What Olmesartan medoxomil is and what it is used for Olmesartan medoxomil belongs to a group of medicines called angiotensin-II receptor antagonists. They lower blood pressure by relaxing the blood vessels. This medicine is used for the treatment of high blood pressure (also known as ‘hypertension’) in adults and in children and adolescents aged 6 to less than 18 years. High blood pressure can damage blood vessels in organs such as the heart, kidneys, brain and eyes. In some cases this may lead to a heart attack, heart or kidney failure, stroke or blindness. -

Consumer Directed Healthcare (CDH) Preventive Medicine List
Consumer Directed Healthcare (CDH) Preventive Medicine List This list provides examples of commonly prescribed preventive medicines. It is not an all-inclusive list; only examples of medicines in each category are listed. This list does not indicate coverage. Please check with your plan administrator and/or benefit information materials if you have questions on coverage. Your cost share will be determined by your plan’s drug coverage and formulary plan. Coverage prior to the deductible being met may not be provided for every dosage form of a listed medicine. Please note: When feasible, brand names are shown in capitals in each category. If generic is available, it is listed in lowercase next to the brand name. If only generics are available (for example, brands are no longer available), they will only be listed in lowercase. BONE DISEASE AND FRACTURES HEART DISEASE AND STROKE OTHER AGENTS ACTONEL, ATELVIA (risedronate) COLESTID (colestipol) BLOOD THINNER MEDICINES BONIVA (ibandronate) ezetimibe DUAVEE aspirin, 81 mg & 325 mg* ezetimibe/simvastatin EVISTA (raloxifene) AGGRENOX LOPID (gemfibrozil) FOSAMAX, FOSAMAX D, BINOSTO (aspirin/dipyridamole ER) NIASPAN (niacin) (alendronate) BRILINTA PREVALITE, QUESTRAN RECLAST (zoledronic acid) clopidogrel (cholestyramine) COUMADIN (warfarin) REPATHA CAVITIES DURLAZA ER TRICOR, ANTARA (fenofibrate) CLINPRO EFFIENT TRILIPIX DR (fenofibric acid) GEL-KAM ELIQUIS WELCHOL PHOS-FLUR PERSANTINE (dipyridamole) PREVIDENT PRADAXA HIGH BLOOD PRESSURE Sodium fluoride rinse, gel, SAVAYSA ACE INHIBITORS cream, -

Cjpp-2016-0090.Pdf
Canadian Journal of Physiology and Pharmacology Effects of Telmisartan and Pioglitazone on High Fructose Induced Metabolic Syndrome in Rats Journal: Canadian Journal of Physiology and Pharmacology Manuscript ID cjpp-2016-0090.R1 Manuscript Type: Article Date Submitted by the Author: 14-Mar-2016 Complete List of Authors: Shahataa, Mary; Beni Suef University Faculty of Medicine Mostafa-Hedeab, Gomaa; Beni Suef University Faculty of Medicine; Faculty of medicine Al jouf University Ali, Esam; DraftCairo University Kasr Alainy Faculty of Medicine Mahdi, Emad; Beni Suef University Faculty of Veterinary Medicine Mahmoud, Fatma; Cairo University Kasr Alainy Faculty of Medicine Keyword: https://mc06.manuscriptcentral.com/cjpp-pubs Page 1 of 54 Canadian Journal of Physiology and Pharmacology Effects of Telmisartan and Pioglitazone on High Fructose Induced Metabolic Syndrome in Rats Mary Girgis Shahataa 1, Gomaa Mostafa-Hedeab 1, 2 , Esam Fouaad Ali 3, Emad ahmed Mahdi 4, Fatma Abd Elhaleem Mahmoud 3 1Pharmacology department - Faculty of Medicine- Beni Suef University - Egypt 2 pharmacology department – faculty of medicine – Al Jouf University – Saudia Arabia 3Pharmacology department - Faculty of Medicine- Cairo University – Egypt 4 pathology department – faculty of veterinary medicine - Beni SuefDraft University - Egypt Corresponding author: Dr Gomaa Mostafa-Hedeab - Address : Pharmacology department - Faculty of Medicine- Beni Suef University – Egypt - Telephone:+201124225264 - Postal code: 62511 - Fax: +20 (82) 233 3367 • Email: [email protected]