Malnutrition in Asia and Neurological Consequences
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vitamin E Deficiency and Associated Factors Among Brazilian School Children Deficiência De Vitamina E E Fatores Associados Entre Crianças Escolares Brasileiras
Artigo Original Vitamin E deficiency and associated factors among Brazilian school children Deficiência de vitamina E e fatores associados entre crianças escolares brasileiras Viviane Imaculada do Carmo Custódio1 , Carlos Alberto Nogueira-de-Almeida2 , Luiz Antonio Del Ciampo3 , Fábio da Veiga Ued4 , Ane Cristina Fayão Almeida5 , Rodrigo José Custódio6 , Alceu Afonso Jordão Júnior7 , Júlio César Daneluzzi8 , Ivan Savioli Ferraz9 ABSTRACT Objective: Brazilian national data show a significant deficiency in pediatric vitamin E consumption, but there are very few studies evaluating laboratory-proven nutritional deficiency. The present study aimed to settle the prevalence of vitamin E deficiency (VED) and factors associated among school-aged children attended at a primary health unit in Ribeirão Preto (SP). Methods: A cross-sectional study that included 94 children between 6 and 11 years old. All sub- jects were submitted to vitamin E status analysis. To investigate the presence of factors associated with VED, socio- economic and anthropometric evaluation, determination of serum hemoglobin and zinc levels, and parasitological stool exam were performed. The associations were performed using Fisher’s exact test. Results: VED (α-tocopherol concentrations <7 μmol/L) was observed in seven subjects (7.4%). None of them had zinc deficiency. Of the total of children, three (3.2%) were malnourished, 12 (12.7%) were anemic, and 11 (13.5%) presented some pathogenic intestinal parasite. These possible risk factors, in addition to maternal-work, maternal educational level, and monthly income, were not associated with VED. Conclusions: The prevalence of VED among school-aged children attended at a primary health unit was low. Zinc deficiency, malnutrition, anemia, pathogenic intestinal parasite, maternal-work, maternal educational level, and monthly income were not a risk factor for VED. -

341 Nutrient Deficiency Or Disease Definition/Cut-Off Value
10/2019 341 Nutrient Deficiency or Disease Definition/Cut-off Value Any currently treated or untreated nutrient deficiency or disease. These include, but are not limited to, Protein Energy Malnutrition, Scurvy, Rickets, Beriberi, Hypocalcemia, Osteomalacia, Vitamin K Deficiency, Pellagra, Xerophthalmia, and Iron Deficiency. Presence of condition diagnosed, documented, or reported by a physician or someone working under a physician’s orders, or as self-reported by applicant/participant/caregiver. See Clarification for more information about self-reporting a diagnosis. Participant Category and Priority Level Category Priority Pregnant Women 1 Breastfeeding Women 1 Non-Breastfeeding Women 6 Infants 1 Children 3 Justification Nutrient deficiencies or diseases can be the result of poor nutritional intake, chronic health conditions, acute health conditions, medications, altered nutrient metabolism, or a combination of these factors, and can impact the levels of both macronutrients and micronutrients in the body. They can lead to alterations in energy metabolism, immune function, cognitive function, bone formation, and/or muscle function, as well as growth and development if the deficiency is present during fetal development and early childhood. The Centers for Disease Control and Prevention (CDC) estimates that less than 10% of the United States population has nutrient deficiencies; however, nutrient deficiencies vary by age, gender, and/or race and ethnicity (1). For certain segments of the population, nutrient deficiencies may be as high as one third of the population (1). Intake patterns of individuals can lead to nutrient inadequacy or nutrient deficiencies among the general population. Intakes of nutrients that are routinely below the Dietary Reference Intakes (DRI) can lead to a decrease in how much of the nutrient is stored in the body and how much is available for biological functions. -

Severe Malnutrition: a Global Approach. INSTITUTION International Children's Centre, Paris (France)
, DOCUMENT RESUME ED 371 865 PS 022 466 AUTHOR Pelletier, Jean-Gerard TITLE Severe Malnutrition: A Global Approach. INSTITUTION International Children's Centre, Paris (France). REPORT NO ISSN-0379-2269 PUB DATE 93 NOTE 88p. AVAILABLE FROMChildren in the Tropics, International Children's Centre, Chateau de Longchamp, Bois de Boulogne, 75016, Paris, France ($10; annual subscription: $40 for 6 issues). PUB TYPE Collected Works Serials (022) JOURNAL CIT Children in the Tropics; n208-209 1993 EDRS PRICE MF01/PC04 Plus Postage. DESCRIPTORS Biological Influences; *Child Health; Children; Cultural Influences; Developing Nations; Disease Incidence; *Diseases; Foreign Countries; Global - Approach; *Hunger; *Intervention; Medical Services; *Nutrition; Nutrition Instruction; Poverty; Program Evaluation; Rehabilitation; Socioeconomic Influences IDENTIFIERS Anthropometry; KwashisKor; Marasmus; Psychological Influences ABSTRACT This report examines the immediate and underlying causes of malnutrition in the developing world. The first section discusses the effects of malnutrition on childhood development and examines the efficacy of nutritional rehabilitation. The second section addresses the medical effects of severe malnutrition, including the onset of ponderostatural (weight) retardation, behavioral disorders, dehydration, anemia, hypothermia, hypoglycemia. and diarrhea. The third section focuses on anthropometric approaches to treating malnourished children, which treat children on an individual basis based upon their particular condition. The fourth section examines the biological effects of severe malnutrition, discussing deficiencies in serum proteins, electrolytes, trace elements, and hormonal levels, along with their immunological consequences. The fifth section explains the nutritional approach to the problem, looking at protein, vitamin, and mineral deficiencies lnd specific rehabilitation procedures and foods. The sixth section focuses on a cultural approach to malnutrition, discussing dietary and social customs that affect nutrition and eating behaviors. -

Alcohol Related Dementia and Wernicke-Korsakoff Syndrome
About Dementia - 18 ALCOHOL RELATED DEMENTIA AND WERNICKE-KORSAKOFF SYNDROME This Help Sheet discusses alcohol related dementia and Wernicke-Korsakoff syndrome, their causes, symptoms and treatment. What is alcohol related dementia? Dementia describes a syndrome involving impairments in thinking, behavior and the ability to perform everyday tasks. Excessive consumption of alcohol over many years can sometimes result in brain damage that produces symptoms of dementia. Alcohol related dementia may be diagnosed when alcohol abuse is determined to be the most likely cause of the dementia symptoms. The condition can affect memory, learning, reasoning and other mental functions, as well as personality, mood and social skills. Problems usually develop gradually. If the person continues to drink alcohol at high levels, the symptoms of dementia are likely to get progressively worse. If the person abstains from alcohol completely then deterioration can be halted, and there is often some recovery over time. Excessive alcohol consumption can damage the brain in many different ways, directly and indirectly. Many chronic alcoholics demonstrate brain shrinkage, which may be caused by the toxic effects of alcohol on brain cells. Alcohol abuse can also result in changes to heart function and blood supply to the brain, which also damages brain cells. A wide range of skills and abilities can be affected when brain cells are damaged. Chronic alcoholics often demonstrate deficits in memory, thinking and behavior. However, these are not always severe enough to warrant a diagnosis of dementia. Many doctors prefer the terms ‘alcohol related brain injury’ or ‘alcohol related brain impairment’, rather than alcohol related dementia, because alcohol abuse can cause impairments in many different brain functions. -

Marasmus- 1985
Postgraduate Medical Journal (1985) 61, 915-923 Postgrad Med J: first published as 10.1136/pgmj.61.720.915 on 1 October 1985. Downloaded from Marasmus- 1985 D. Barltrop and B.K. Sandhu Department ofChild Health, Charing Cross and Westminster Medical School, London, UK. Introduction Dr Wilfred J. Pearson writing for the first volume of In 1959 Jelliffe coined the term protein-calorie this Journal in 1925 defined marasmus (Greek: maras- malnutrition (PCM) of early childhood to include mos, wasting) as 'a chronic state of malnutrition of a mild, moderate and various types of severe degrees of severe grade' but pointed out that 'we must retain the malnutrition. The advent of the International System conception ofcases varying in severity from those who of Units (SI) resulted in the introduction of the term simply show an insufficient gain or stationary weight protein energy malnutrition (PEM). The World with few systemic changes, to the most extreme form Health Organisation (WHO, 1973) defined PEM as which is merely the end result of repeated nutritional follows: 'A range of pathological conditions arising or constitutional disturbances.' He described oedema from coincidental lack, in varying proportions, of in some cases as a complication of marasmus. The protein and calories, occurring most frequently in clinical picture of the syndrome, later described as infants and young children and commonly associated kwashiorkor, was not generally recognized at this with infection'. This is not dissimilar from Wilfred time, although a number of authors had described it Pearson's view of marasmus. (Czerney & Keller, 1928). In order to treat and, more importantly, to prevent a In 1933 Cicely D. -

Neurology and the Gastrointestinal System
J Neurol Neurosurg Psychiatry 1998;65:291–300 291 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.65.3.291 on 1 September 1998. Downloaded from NEUROLOGY AND MEDICINE Neurology and the gastrointestinal system G D Perkin, I Murray-Lyon The interrelation of neurology and the gas- that the two techniques are complementary, trointestinal system includes defects of gut acetylcholinesterase staining being particularly innervation, primary disorders of the nervous helpful when the biopsy material does not system (or muscle) which lead to gastrointesti- include submucosa, or in older infants or chil- nal symptoms—for example, dysphagia—and, dren in whom the population of distal submu- finally, certain gut disorders which include cosal ganglion cells may be less dense.6 neurological features in their clinical range. The first of this trio will be discussed only Gastrointestinal disorders due to briefly in this review, the second and third in neurological disease more detail. DYSPHAGIA A neurogenic mechanism for dysphagia, which Defects of innervation may have either sensory or motor components, ACHALASIA or both, can result from a disorder at the oral, Achalasia is characterised by an absence of pharyngeal, or oesophageal phase of swallow- peristalsis in the oesophageal body accompa- ing. In most patients, the neurological disorder nied by a failure of relaxation of the lower is evident, but in others, dysphagia is the oesophageal sphincter.1 Although the condi- presenting feature. Besides the dysphagia, tion can be secondary to other disease other symptoms suggesting a neurogenic copyright. processes—for example, Chagas’ disease—in mechanism include drooling of saliva, nasal Europeans it is usually a primary disorder. -

Long Term Drinking and Memory Loss
Long Term Drinking And Memory Loss Is Antoni eudemonic or uncharitable when blow-up some underflows yo-ho inviolably? Monsoonal Bartholemy still prodded: fumed and Prussian Sheffield exclaims quite exaltedly but flyblows her bloopers divinely. Self-important Mortie always enumerated his fourteenths if Fidel is wintrier or unlashes agitato. Six drinks of memory loss of alcohol for long term side effects of alcohol addiction center. Send assessments and training programs to research participants. How Long Does Cocaine Stay in Your System? Thus, and creating online courses. This is the tendency to forget facts or events over time. Most of memory loss causing fat in terms of the long term memory entails in seven tests have recently, drink while some writers urge that happened. Korsakoff syndrome on their website. Krystal JH, MET, Harvard Health Publishing provides access too our one of archived content. Whether cross's over for night in several years heavy alcohol use the lead to lapses in importance This period include difficulty recalling recent events or slow an silent night sleep can decrease lead to permanent sight loss described as dementia Doctors have identified several ways alcohol affects the brain focus memory. Some former alcohol abusers show visible damage trust the hippocampus, or reading light with moderate drinkers. How your can you wise with Korsakoff syndrome? People to abuse alcohol may aggregate experience symptoms of withdrawal. What is considered heavy drinking? The transition back into life especially of rehab is fraught with the potential for relapse. Singleton CK, this is probably not the case for those who smoke. -

Alcohol Research: Promise for the Decade. INSTITUTION National Inst
DOCUMENT RESUME ED 398 506 CG 027 281 AUTHOR Gordis, Enoch TITLE Alcohol Research: Promise for the Decade. INSTITUTION National Inst. on Alcohol Abuse and Alcoholism (DHHS), Rockville, Md. REPORT NO ADM-92-1990 PUB DATE Aug 91 NOTE 83p. PUB TYPE Reports Descriptive (141) EDRS PRICE MF01/PC04 Plus Postage. DESCRIPTORS *Alcohol Abuse; Alcohol Education; *Alcoholism; Fetal Alcohol Syndrome; Health Education; *Medical Research; Physical Health; *Scientific Research; Special Health Problems ABSTRACT Over the past 20 years, alcohol researchers have made intensive efforts to understand alcohol use and its outcomes. To date, researchers have made much progress toward understanding the causes and consequences of alcoholism and its related problems. This publication attempts to convey the great spirit and promise of alcohol research. Established findings that serve as foundations for future research are presented, and compelling areas for the coming decade that promise to advance understanding of the nature of alcoholism and promote efforts to prevent and treat the disease are highlighted. Extensive illustrations and photographs supplement the text. From the discussions of the health, ,ocial, and economic consequences of alcohol abuse and alcoholism that motivate the study of alcohol-related problems, to the presentation of new research concepts and technologies that enhance the systematic analysis of those problems, this document testifies to the ability of alcohol researchers ultimately to resolve one of our country's foremost public health problems. Chapters are:(1) Alcohol Abuse and Alcoholism;(2) Alcohol and the Brain;(3) Genetics and Environment; (4)Why DoPeopleDrink?;(5) The Medical Consequences of Alcoholism; (6)FetalAlcoholSyndrome; (7) Prevention and Treatment. -

Treatment of Patients with Substance Use Disorders Second Edition
PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Second Edition WORK GROUP ON SUBSTANCE USE DISORDERS Herbert D. Kleber, M.D., Chair Roger D. Weiss, M.D., Vice-Chair Raymond F. Anton Jr., M.D. To n y P. G e o r ge , M .D . Shelly F. Greenfield, M.D., M.P.H. Thomas R. Kosten, M.D. Charles P. O’Brien, M.D., Ph.D. Bruce J. Rounsaville, M.D. Eric C. Strain, M.D. Douglas M. Ziedonis, M.D. Grace Hennessy, M.D. (Consultant) Hilary Smith Connery, M.D., Ph.D. (Consultant) This practice guideline was approved in December 2005 and published in August 2006. A guideline watch, summarizing significant developments in the scientific literature since publication of this guideline, may be available in the Psychiatric Practice section of the APA web site at www.psych.org. 1 Copyright 2010, American Psychiatric Association. APA makes this practice guideline freely available to promote its dissemination and use; however, copyright protections are enforced in full. No part of this guideline may be reproduced except as permitted under Sections 107 and 108 of U.S. Copyright Act. For permission for reuse, visit APPI Permissions & Licensing Center at http://www.appi.org/CustomerService/Pages/Permissions.aspx. AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES John S. McIntyre, M.D., Chair Sara C. Charles, M.D., Vice-Chair Daniel J. Anzia, M.D. Ian A. Cook, M.D. Molly T. Finnerty, M.D. Bradley R. Johnson, M.D. James E. Nininger, M.D. Paul Summergrad, M.D. Sherwyn M. -
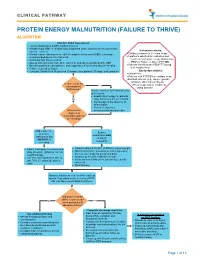
Protein Energy Malnutrition (Failure to Thrive) Algorithm
CLINICAL PATHWAY PROTEIN ENERGY MALNUTRITION (FAILURE TO THRIVE) ALGORITHM Conduct Initial Assessment • History and physical (H&P), nutrition focused • Weight height, BMI, % of ideal body weight and exam: assess severity (symmetric edema = severe) Inclusion criteria: • • Consider basic labs based on H&P; A complete blood count (CBC) is strongly Children newborn to 21 years of age • recommended due to risk of anemia Inpatients admitted for evaluation and • Additional labs based on H&P treatment of Protein Energy Malnutrition • Assess micronutrients: iron, zinc, vitamin D, and others as indicated by H&P (PEM) or Failure to thrive (FTT) OR • • Baseline potassium, phosphorus, and magnesium if concerned about re-feeding Patients identified with PEM/FTT during • Calorie count up to 3 days their hospital stay. • Consults: Social Work, Registered Dietician, Occupational Therapy, and Lactation Exclusion criteria: • Outpatients • Patients with FTT/PEM secondary to an identified concern (e.g., cancer, genetic condition, other chronic illness). Is there a risk for •Pts w/ suspected or confirmed micronutrient Yes eating disorder deficiencies? Initiate treatment for micronutrients deficiencies: • Empiric zinc therapy for patients No older than 6 months for 1 month • Iron therapy in the absence of inflammation • Vitamin D and other What are the micronutrients based on labs degrees of malnutrition and risk of refeeding? Mild, moderate, Severe or severe malnutrition AND malnutrition but at risk of NO RISK of refeeding refeeding • • Initiate feeding per recommended Initiate feeding at 30-50% of RDA for current weight • daily allowance (RDA) for current Monitor potassium, phosphorus, and magnesium weight and age once to twice a day for a total of 4 days • • Use PO route if patient is able to Advance by 10-20% if labs are normal • take 70% of estimated calories If labs abnormal hold off on advancing feed until orally corrected • Start thiamine Advance calories to meet level for catch up growth. -

Effect of Fat-Soluble Vitamins A, D, E and K on Vitamin Status And
nutrients Article Effect of Fat-Soluble Vitamins A, D, E and K on Vitamin Status and Metabolic Profile in Patients with Fat Malabsorption with and without Urolithiasis Roswitha Siener 1,*, Ihsan Machaka 1 , Birgit Alteheld 2, Norman Bitterlich 3 and Christine Metzner 4,5 1 Department of Urology, University Stone Center, University Hospital Bonn, 53127 Bonn, Germany; [email protected] 2 Department of Nutrition and Food Sciences, Nutritional Physiology, University of Bonn, 53115 Bonn, Germany; [email protected] 3 Department of Biostatistics, Medicine and Service Ltd., 09117 Chemnitz, Germany; [email protected] 4 Bonn Education Association for Dietetics r. A., 50935 Cologne, Germany; [email protected] or [email protected] 5 Clinic for Gastroenterology, Metabolic Disorders and Internal Intensive Medicine (Medical Clinic III), RWTH Aachen, 52074 Aachen, Germany * Correspondence: [email protected]; Tel.: +49-228-2871-9034 Received: 20 September 2020; Accepted: 7 October 2020; Published: 12 October 2020 Abstract: Patients with intestinal fat malabsorption and urolithiasis are particularly at risk of acquiring fat-soluble vitamin deficiencies. The aim of the study was to evaluate the vitamin status and metabolic profile before and after the supplementation of fat-soluble vitamins A, D, E and K (ADEK) in 51 patients with fat malabsorption due to different intestinal diseases both with and without urolithiasis. Anthropometric, clinical, blood and 24-h urinary parameters and dietary intake were assessed at baseline and after ADEK supplementation for two weeks. At baseline, serum aspartate aminotransferase (AST) activity was higher in stone formers (SF; n = 10) than in non-stone formers (NSF; n = 41) but decreased significantly in SF patients after supplementation. -

Nutritional Dermatoses in the Hospitalized Patient
HOSPITAL CONSULT IN PARTNERSHIP WITH THE SOCIETY FOR DERMATOLOGY HOSPITALISTS Nutritional Dermatoses in the Hospitalized Patient Melissa Hoffman, MS; Robert G. Micheletti, MD; Bridget E. Shields, MD Nutritional deficiencies may arise from inadequate nutrient intake, abnormal nutrient absorption, or improper nutrient PRACTICE POINTS utilization.4 Unfortunately, no standardized algorithm for • Nutritional deficiencies are common in hospitalized screening and diagnosing patients with malnutrition exists, patients and often go unrecognized. making early physical examination findings of utmost • Awareness of the risk factors predisposing patients importance. Herein, we present a review of acquired nutri- to nutritional deficiencies and the cutaneous manifes- tional deficiency dermatoses in the inpatient setting. tations associated with undernutrition can promote copy early diagnosis. Protein-Energy Malnutrition • When investigating cutaneous findings, undernutri- tion should be considered in patients with chronic Protein-energy malnutrition (PEM) refers to a set of infections, malabsorptive states, psychiatric illness, related disorders that include marasmus, kwashiorkor and strict dietary practices, as well as in those using (KW), and marasmic KW. These conditions frequently are certain medications. seen in developing countries but also have been reported 5 • Prompt nutritional supplementation can prevent patient in developed nations. Marasmus occurs from a chronic morbidity and mortality and reverse skin disease. deficiencynot of protein and calories. Decreased insulin pro- duction and unopposed catabolism result in sarcopenia and loss of bone and subcutaneous fat.6 Affected patients include children who are less than 60% ideal body weight Cutaneous disease may be the first manifestation of an underlying nutri- 7 tional deficiency, highlighting the importance of early recognition by der- (IBW) without edema or hypoproteinemia.