Encapsulation of Vitamin D3 in Gum Arabic to Improve Application in Beverages and Enhance Bioavailability
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Does Dietary Fiber Affect the Levels of Nutritional Components After Feed Formulation?
fibers Article Does Dietary Fiber Affect the Levels of Nutritional Components after Feed Formulation? Seidu Adams 1 ID , Cornelius Tlotliso Sello 2, Gui-Xin Qin 1,3,4, Dongsheng Che 1,3,4,* and Rui Han 1,3,4 1 College of Animal Science and Technology, Jilin Agricultural University, Changchun 130118, China; [email protected] (S.A.); [email protected] (G.-X.Q.); [email protected] (R.H.) 2 College of Animal Science and Technology, Department of Animal Genetics, Breeding and Reproduction, Jilin Agricultural University, Changchun 130118, China; [email protected] 3 Key Laboratory of Animal Production, Product Quality and Security, Jilin Agricultural University, Ministry of Education, Changchun 130118, China 4 Jilin Provincial Key Laboratory of Animal Nutrition and Feed Science, Jilin Agricultural University, Changchun 130118, China * Correspondence: [email protected]; Tel.: +86-136-4431-9554 Received: 12 January 2018; Accepted: 25 April 2018; Published: 7 May 2018 Abstract: Studies on dietary fiber and nutrient bioavailability have gained an increasing interest in both human and animal nutrition. Questions are increasingly being asked regarding the faith of nutrient components such as proteins, minerals, vitamins, and lipids after feed formulation. The aim of this review is to evaluate the evidence with the perspective of fiber usage in feed formulation. The consumption of dietary fiber may affect the absorption of nutrients in different ways. The physicochemical factors of dietary fiber, such as fermentation, bulking ability, binding ability, viscosity and gel formation, water-holding capacity and solubility affect nutrient absorption. The dietary fiber intake influences the different methods in which nutrients are absorbed. -

Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Analysis of Phenolic and Cyclic Compounds in Plants Using Derivatization Techniques in Combination with GC-MS-Based Metabolite Profiling
Molecules 2015, 20, 3431-3462; doi:10.3390/molecules20023431 OPEN ACCESS molecules ISSN 1420-3049 www.mdpi.com/journal/molecules Review Analysis of Phenolic and Cyclic Compounds in Plants Using Derivatization Techniques in Combination with GC-MS-Based Metabolite Profiling Jens Rohloff Department of Biology, Norwegian University of Science and Technology, Trondheim 7491, Norway; E-Mail: [email protected]; Tel.: +47-7359-6093; Fax: +47-7359-6100 Academic Editor: Derek J. McPhee Received: 18 December 2014 / Accepted: 10 February 2015 / Published: 17 February 2015 Abstract: Metabolite profiling has been established as a modern technology platform for the description of complex chemical matrices and compound identification in biological samples. Gas chromatography coupled with mass spectrometry (GC-MS) in particular is a fast and accurate method widely applied in diagnostics, functional genomics and for screening purposes. Following solvent extraction and derivatization, hundreds of metabolites from different chemical groups can be characterized in one analytical run. Besides sugars, acids, and polyols, diverse phenolic and other cyclic metabolites can be efficiently detected by metabolite profiling. The review describes own results from plant research to exemplify the applicability of GC-MS profiling and concurrent detection and identification of phenolics and other cyclic structures. Keywords: derivatization; food chemistry; gas chromatography; mass spectrometry; phenols; phenolic acids 1. Introduction Chromatographic techniques for the detection and identification of metabolites in plant material have undergone major changes in recent years due to improvements of analysis time, detection limit and separation characteristics. Depending on the biological question, one might distinguish between targeted and non-targeted strategies. Gas chromatography (GC) in particular is characterized by sensitivity and reliability of separations and detection of complex sample mixtures. -

Vitamin A, E, & D Unit Change
Vitamin A, E, & D Unit Change Agenda The following provides an overview of the updated units that NQAC Dublin will be using to adhere to FDA guideline changes regarding Nutrition and Supplement Facts labels. This presentation will review: • FDA Guidelines • Methods Affected • Unit Changes by Vitamin • Conversions In August of 2019, the FDA updated its guideline requirements for Nutrition and Supplement Facts labels regarding vitamin A, vitamin D, and vitamin E. The following link can be used to access the FDA guidelines directly: www.fda.gov/regulatory-information Which methods are affected by this change? • LI-00.608 –Multi Fat • LI-03.701 –Fat Soluble Vitamin Determination in Premixes • LI-00.683- Carotene • GOP-756-1001- Total Vitamin A by Calculation (will be obsoleted) FDA Provided Unit Conversion Table: Vitamin A The previous RDI for vitamin A was expressed in International Units (IU), a measurement based on the biological activity or effect, where one IU of vitamin A activity had been defined as equal to 0.30 mcg of all-trans-retinol or 0.60 mcg of all-trans-β-carotene The new unit of measure, RAE, considers the vitamin A activity of β-carotene in supplements to be half the activity of pre-formed retinol, and the vitamin A activity of dietary β-carotene to be one- sixth of the β-carotene in supplements Furthermore, carotenoids, such as β-carotene, added to food is assumed to have the same bioconversion as those naturally occurring in foods (12:1). For the other dietary provitamin A carotenoids, β-cryptoxanthin and α-carotene, the RAE is set at 24 based on a vitamin A activity approximately half of that for β-carotene. -

A Clinical Update on Vitamin D Deficiency and Secondary
References 1. Mehrotra R, Kermah D, Budoff M, et al. Hypovitaminosis D in chronic 17. Ennis JL, Worcester EM, Coe FL, Sprague SM. Current recommended 32. Thimachai P, Supasyndh O, Chaiprasert A, Satirapoj B. Efficacy of High 38. Kramer H, Berns JS, Choi MJ, et al. 25-Hydroxyvitamin D testing and kidney disease. Clin J Am Soc Nephrol. 2008;3:1144-1151. 25-hydroxyvitamin D targets for chronic kidney disease management vs. Conventional Ergocalciferol Dose for Increasing 25-Hydroxyvitamin supplementation in CKD: an NKF-KDOQI controversies report. Am J may be too low. J Nephrol. 2016;29:63-70. D and Suppressing Parathyroid Hormone Levels in Stage III-IV CKD Kidney Dis. 2014;64:499-509. 2. Hollick MF. Vitamin D: importance in the prevention of cancers, type 1 with Vitamin D Deficiency/Insufficiency: A Randomized Controlled Trial. diabetes, heart disease, and osteoporosis. Am J Clin Nutr 18. OPKO. OPKO diagnostics point-of-care system. Available at: http:// J Med Assoc Thai. 2015;98:643-648. 39. Jetter A, Egli A, Dawson-Hughes B, et al. Pharmacokinetics of oral 2004;79:362-371. www.opko.com/products/point-of-care-diagnostics/. Accessed vitamin D(3) and calcifediol. Bone. 2014;59:14-19. September 2 2015. 33. Kovesdy CP, Lu JL, Malakauskas SM, et al. Paricalcitol versus 3. Giovannucci E, Liu Y, Rimm EB, et al. Prospective study of predictors ergocalciferol for secondary hyperparathyroidism in CKD stages 3 and 40. Petkovich M, Melnick J, White J, et al. Modified-release oral calcifediol of vitamin D status and cancer incidence and mortality in men. -

Structure & Function: Lipids and Membranes
Structure & Function: Lipids and Membranes Lipids vironment of the body requires special struc- Lipids are a diverse group of molecules tures. Other, amphipathic lipids, such as that all share the characteristic that glycerophospholipids and sphin- at least a portion of them is hy- YouTube Lectures golipids spontaneously organize drophobic. Lipids play many by Kevin themselves into lipid bilayers HERE & HERE roles in cells, including serving as when placed in water. Interest- energy storage (fats/oils), constitu- ingly, major parts of many lipids can ents of membranes (glycerophospholipids, be derived from acetyl-CoA. sphingolipids, cholesterol), hormones (steroids), vitamins (fat soluble), oxygen/ Fatty acids electron carriers (heme), among others. For The most ubiquitous lipids in cells are the lipids that are very hydrophobic, such as fats/ fatty acids. Found in fats, glycerophos- oils, movement and storage in the aqueous en- pholipids, sphingolipids and serving as as 220 Figure 2.190 - Saturated fatty acid Figure 2.191 - Arachidonic acid - A (stearic acid) and unsaturated fatty acid polyunsaturated fatty acid (oleic acid) Wikipedia membrane anchors for proteins and other biomolecules, fatty acids are important for en- ergy storage, membrane structure, and as pre- cursors of most classes of lipids. Fatty acids, as can be seen from Figure 2.190 are charac- terized by a polar head group and a long hy- drocarbon tail. Fatty acids with hydrocarbon tails that lack any double bonds are described as saturated, while those with one or more double bonds in their tails are known as un- saturated fatty acids. The effect of double bonds on the fatty acid tail is to introduce a kink, or bend, in the tail, as shown for oleic acid. -

Dietary Supplements Compendium Volume 1
2015 Dietary Supplements Compendium DSC Volume 1 General Notices and Requirements USP–NF General Chapters USP–NF Dietary Supplement Monographs USP–NF Excipient Monographs FCC General Provisions FCC Monographs FCC Identity Standards FCC Appendices Reagents, Indicators, and Solutions Reference Tables DSC217M_DSCVol1_Title_2015-01_V3.indd 1 2/2/15 12:18 PM 2 Notice and Warning Concerning U.S. Patent or Trademark Rights The inclusion in the USP Dietary Supplements Compendium of a monograph on any dietary supplement in respect to which patent or trademark rights may exist shall not be deemed, and is not intended as, a grant of, or authority to exercise, any right or privilege protected by such patent or trademark. All such rights and privileges are vested in the patent or trademark owner, and no other person may exercise the same without express permission, authority, or license secured from such patent or trademark owner. Concerning Use of the USP Dietary Supplements Compendium Attention is called to the fact that USP Dietary Supplements Compendium text is fully copyrighted. Authors and others wishing to use portions of the text should request permission to do so from the Legal Department of the United States Pharmacopeial Convention. Copyright © 2015 The United States Pharmacopeial Convention ISBN: 978-1-936424-41-2 12601 Twinbrook Parkway, Rockville, MD 20852 All rights reserved. DSC Contents iii Contents USP Dietary Supplements Compendium Volume 1 Volume 2 Members . v. Preface . v Mission and Preface . 1 Dietary Supplements Admission Evaluations . 1. General Notices and Requirements . 9 USP Dietary Supplement Verification Program . .205 USP–NF General Chapters . 25 Dietary Supplements Regulatory USP–NF Dietary Supplement Monographs . -

Simultaneous Measurement of Vitamins A, D, E and K Along With
Simultaneous Measurement of 1110 Note Application Vitamins A, D, E and K Along with CoQ10 and Carotenoids, in Multivitamin Tablets, Infant Formula and Milk Ian Acworth and Paul Gamache, Thermo Fisher Scientific, Chelmsford, MA, USA Key Words Carotenoids, Food Supplements, HPLC-ECD, Multivitamins, Retinoids, Tocopheryl Acetate Goal To develop a sensitive and selective HPLC-electrochemical detection (ECD) method for the simultaneous measurement of numerous fat-soluble nutrients Introduction Consumer interest and regulatory concerns for food This Application Note shows the use of the Thermo supplements, fortified food products and dietary nutrients Scientific™ Dionex™ CoulArray™ Coulometric Array have stimulated the development of improved analytical Detector for the measurement of a variety of lipid- methods. Fat-soluble nutrients are of particular interest soluble nutrients including vitamins A (retinol), D2 due to their potential health benefits and, in some cases, (ergocalciferol), D3 (cholecalciferol), E (a- and toxicity. Accurate, simple techniques for comprehensive γ-tocopherol), and K1 (phylloquinone), along with analysis is important for product labeling, nutritional carotenoids (a- and b-carotene), retinoids (retinyl research, development and quality control.1 palmitate), tocopheryl acetate, and coenzyme Q10 (ubiquinone) (Figure 1). The analysis of multivitamin Most laboratories use individual methods for a single tablets, infant formula and milk are given as examples. analyte class. Many methods, for example, include a Since extraction -
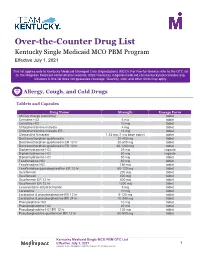
Over-The-Counter Drug List
Over-the-Counter Drug List Kentucky Single Medicaid MCO PBM Program Effective July 1, 2021 This list applies only to Kentucky Medicaid Managed Care Organizations (MCO). For Fee-for-Service refer to the OTC list on the Magellan Medicaid Administration website: https://kentucky.magellanmedicaid.com/kentucky/source/index.asp. Inclusion in this list does not guarantee coverage. Quantity, cost, and other limits may apply. Allergy, Cough, and Cold Drugs Tablets and Capsules Drug Name Strength Dosage Form All Day Allergy (cetirizine) tablet Cetirizine HCl 5 mg tablet Cetirizine HCl 10 mg tablet Chlorpheniramine maleate 4 mg tablet Chlorpheniramine maleate ER 12 mg tablet Clemastine fumarate 1.34 mg (1 mg base equiv) tablet Dextromethorphan-guaifenesin 20-400 mg tablet Dextromethorphan-guaifenesin ER 12 hr 30-600 mg tablet Dextromethorphan-guaifenesin ER 12 hr 60-1200 mg tablet Diphenhydramine HCl 25 mg capsule Diphenhydramine HCl 50 mg capsule Diphenhydramine HCl 50 mg tablet Fexofenadine HCl 60 mg tablet Fexofenadine HCl 180 mg tablet Fexofenadine-pseudoephedrine ER 12 hr 60-120 mg tablet Guaifenesin 200 mg tablet Guaifenesin 400 mg tablet Guaifenesin ER 12 hr 600 mg tablet Guaifenesin ER 12 hr 1200 mg tablet Levocetirizine dihydrochloride 5 mg tablet Loratadine 10 mg tablet Loratadine & pseudoephedrine ER 12 hr 5-120 mg tablet Loratadine & pseudoephedrine ER 24 hr 10-240 mg tablet Phenylephrine HCl 10 mg tablet Pseudoephedrine HCl 30 mg tablet Pseudoephedrine HCl ER 12 hr 120 mg tablet Pseudoephedrine-guaifenesin ER 12 hr 60-600 mg tablet Kentucky Medicaid Single MCO PBM OTC List Effective July 1, 2021 1 Copyright © 2021 MedImpact Healthcare Systems, Inc. -
Possible Ocular Adverse Effects Attributable to Bisphosphonate
r e v c o l o m b r e u m a t o l . 2 0 1 7;2 4(1):54–59 w ww.elsevier.es/rcreuma Case report Possible ocular adverse effects attributable to ଝ bisphosphonate therapy: Two case reports a b,∗ Luis Guillermo Gómez Escobar , Deyanira González Devia a Facultad de Medicina, Universidad de los Andes, Bogotá, Colombia b Medicina Interna, Endocrinología, Hospital Universitario Fundación Santa Fe de Bogotá, Bogotá, Colombia a r t i c l e i n f o a b s t r a c t Article history: Bisphosphonates are used in the management of diseases characterized by an increase in Received 16 June 2015 bone resorption such as osteoporosis, metatasic bone disease, malignant hypercalcemia Accepted 6 June 2016 among others. It has been reported that the use of IV bisphosphonates as zoledronate and Available online 30 April 2017 pamidronate generate ocular adverse effects by an acute phase reaction mediated by an increase of interleukin 6 (IL-6) and tumoral necrosis factor (TNF-␣). We present 2 cases, a Keywords: woman 71 years old and a 67 years old man that received therapy with bisphosphonates Uveitis and 24–72 h later they presented an anterior uveitis. Bisphosphonates © 2016 Asociacion´ Colombiana de Reumatologıa.´ Published by Elsevier Espana,˜ S.L.U. All Zoledronic acid rights reserved. Adverse effect Posibles efectos adversos oculares de los bifosfonatos. Reporte de 2 casos r e s u m e n Palabras clave: Los bifosfonatos se utilizan para el manejo de enfermedades con incremento de la resor- Uveítis ción ósea como la osteoporosis, la enfermedad metastásica ósea y la hipercalcemia maligna, Bifosfonatos entre otras patologías. -

Simultaneous LC/MS Analysis of Carotenoids and Fat-Soluble Vitamins in Costa Rican Avocados (Persea Americana Mill.)
molecules Article Simultaneous LC/MS Analysis of Carotenoids and Fat-Soluble Vitamins in Costa Rican Avocados (Persea americana Mill.) Carolina Cortés-Herrera 1,*, Andrea Chacón 1, Graciela Artavia 1 and Fabio Granados-Chinchilla 2 1 Centro Nacional de Ciencia y Tecnología de Alimentos, Universidad de Costa Rica, Ciudad Universitaria Rodrigo Facio, 11501-2060 San José, Costa Rica; [email protected] (A.C.); [email protected] (G.A.) 2 Centro de Investigación en Nutrición Animal (CINA), Universidad de Costa Rica, Ciudad Universitaria Rodrigo Facio, 11501-2060 San José, Costa Rica; [email protected] * Correspondence: [email protected]; Tel.: +506-2511-7226 Academic Editor: Severina Pacifico Received: 26 August 2019; Accepted: 5 October 2019; Published: 10 December 2019 Abstract: Avocado (a fruit that represents a billion-dollar industry) has become a relevant crop in global trade. The benefits of eating avocados have also been thoroughly described as they contain important nutrients needed to ensure biological functions. For example, avocados contain considerable amounts of vitamins and other phytonutrients, such as carotenoids (e.g., β-carotene), which are fat-soluble. Hence, there is a need to assess accurately these types of compounds. Herein we describe a method that chromatographically separates commercial standard solutions containing both fat-soluble vitamins (vitamin A acetate and palmitate, Vitamin D2 and D3, vitamin K1, α-, δ-, and γ-vitamin E isomers) and carotenoids (β-cryptoxanthin, zeaxanthin, lutein, β-carotene, and lycopene) effectively (i.e., analytical recoveries ranging from 80.43% to 117.02%, for vitamins, and from 43.80% 1 to 108.63%). -

Multigenics®
Multigenics® Optimum Multiple Vitamin/Mineral Formula Fast-Release Tablet Form: Tablets Flavor: Size: 180 Tablets Multigenics® is a unique vitamin and mineral formula designed for optimal disintegration and digestibility, featuring: High levels of ratio-balanced B vitamins with extra B12 to support homocysteine metabolism.* Caro-xan®, our proprietary blend of betacarotene and Betatene® mixed carotenoids for antioxidant protection.* A 2-to-1 ratio of calcium to magnesium for nutritional bone support.* Selenium (as selenium Storage: Keep tightly closed in a cool, dry place. Ingredient Amount Daily 200 mcg 364% Value aspartate) WARNING: Accidental overdose of iron- Serving Size 6 Tablets Copper (as copper citrate) 2 mg 222% containing products is a leading cause of fatal Servings Per Container 30 Manganese (as manganese 1 mg 43% poisoning in children under 6. Keep this product citrate) Total Carbohydrate 2 g 1% out of the reach of children. In case of Chromium (as chromium Dietary Fiber 2 g 7% 200 mcg 571% accidental overdose, call a doctor or poison citrate) control center immediately. Vitamin A (from mixed 3,000 Molybdenum (as carotenoids, beta-carotene,† 333% 100 mcg 222% mcg molybdenum aspartate) *Percent Daily Values are based on a 2,000 calorie and retinyl acetate) Potassium (as potassium diet. 1,200 99 mg 2% Vitamin C (as ascorbic acid) 1,333% aspartate) mg **Daily Value not established. Betaine HCl 325 mg ** Vitamin D (as 0.5 mcg 3% † ® cholecalciferol) (20 IU) Myo-Inositol 188 mg ** Caro-xan , a proprietary blend of beta-carotene and ® Vitamin E (as d-alpha Citrus Bioflavonoid Complex 100 mg ** Betatene mixed carotenoids ††As Metafolin®.