Usefulness of Antidepressants for Improving the Neuropathic Pain-Like State and Pain-Induced Anxiety Through Actions at Different Brain Sites
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetic Neuropathy: a Position Statement by the American
136 Diabetes Care Volume 40, January 2017 Diabetic Neuropathy: A Position Rodica Pop-Busui,1 Andrew J.M. Boulton,2 Eva L. Feldman,3 Vera Bril,4 Roy Freeman,5 Statement by the American Rayaz A. Malik,6 Jay M. Sosenko,7 and Dan Ziegler8 Diabetes Association Diabetes Care 2017;40:136–154 | DOI: 10.2337/dc16-2042 Diabetic neuropathies are the most prevalent chronic complications of diabetes. This heterogeneous group of conditions affects different parts of the nervous system and presents with diverse clinical manifestations. The early recognition and appropriate man- agement of neuropathy in the patient with diabetes is important for a number of reasons: 1. Diabetic neuropathy is a diagnosis of exclusion. Nondiabetic neuropathies may be present in patients with diabetes and may be treatable by specific measures. 2. A number of treatment options exist for symptomatic diabetic neuropathy. 3. Up to 50% of diabetic peripheral neuropathies may be asymptomatic. If not recognized and if preventive foot care is not implemented, patients are at risk for injuries to their insensate feet. 4. Recognition and treatment of autonomic neuropathy may improve symptoms, POSITION STATEMENT reduce sequelae, and improve quality of life. Among the various forms of diabetic neuropathy, distal symmetric polyneurop- athy (DSPN) and diabetic autonomic neuropathies, particularly cardiovascular au- tonomic neuropathy (CAN), are by far the most studied (1–4). There are several 1 atypical forms of diabetic neuropathy as well (1–4). Patients with prediabetes may Division of Metabolism, Endocrinology & Diabe- – tes, Department of Internal Medicine, University also develop neuropathies that are similar to diabetic neuropathies (5 10). -

5-HT1A Receptor-Dependent Modulation of Emotional
www.nature.com/scientificreports OPEN 5-HT1A receptor-dependent modulation of emotional and neurogenic defcits elicited by Received: 8 May 2017 Accepted: 19 January 2018 prolonged consumption of alcohol Published: xx xx xxxx Arnauld Belmer 1,2, Omkar L. Patkar1,2, Vanessa Lanoue3 & Selena E. Bartlett 1,2 Repeated episodes of binge-like alcohol consumption produce anxiety, depression and various deleterious efects including alterations in neurogenesis. While the involvement of the serotonin receptor 1 A (5-HT1A) in the regulation of anxiety-like behavior and neurogenesis is well documented, its contribution to alcohol withdrawal-induced anxiety and alcohol-induced defcits in neurogenesis is less documented. Using the Drinking-In-the-Dark (DID) paradigm to model chronic long-term (12 weeks) binge-like voluntary alcohol consumption in mice, we show that the selective partial activation of 5-HT1A receptors by tandospirone (3 mg/kg) prevents alcohol withdrawal-induced anxiety in a battery of behavioral tests (marble burying, elevated-plus-maze, open-feld), which is accompanied by a robust decrease in binge-like ethanol intake (1 and 3 mg/kg). Furthermore, using triple immunolabelling of proliferation and neuronal diferentiation markers, we show that long-term DID elicits profound defcits in neurogenesis and neuronal fate specifcation in the dorsal hippocampus that are entirely reversed by a 2-week chronic treatment with the 5-HT1A partial agonist tandospirone (3 mg/kg/day). Together, our results confrm previous observations that 5-HT1A receptors play a pivotal role in alcohol drinking behavior and the associated emotional and neurogenic impairments, and suggest that 5-HT1A partial agonists represent a promising treatment strategy for alcohol abuse. -

Pharmacologic Management of Chronic Neuropathic Pain Review of the Canadian Pain Society Consensus Statement
Clinical Review Pharmacologic management of chronic neuropathic pain Review of the Canadian Pain Society consensus statement Alex Mu MD FRCPC Erica Weinberg MD Dwight E. Moulin MD PhD Hance Clarke MD PhD FRCPC Abstract Objective To provide family physicians with EDITOR’S KEY POINTS a practical clinical summary of the Canadian • Gabapentinoids and tricyclic antidepressants play an important role in Pain Society (CPS) revised consensus first-line management of neuropathic pain (NeP). Evidence published statement on the pharmacologic management since the 2007 Canadian Pain Society consensus statement on treatment of neuropathic pain. of NeP shows that serotonin-norepinephrine reuptake inhibitors should now also be among the first-line agents. Quality of evidence A multidisciplinary • Tramadol and opioids are considered second-line treatments owing to their interest group within the CPS conducted a increased complexity of follow-up and monitoring, plus their potential for systematic review of the literature on the adverse side effects, medical complications, and abuse. Cannabinoids are current treatments of neuropathic pain in currently recommended as third-line agents, as sufficient-quality studies are drafting the revised consensus statement. currently lacking. Recommended fourth-line treatments include methadone, anticonvulsants with lesser evidence of efficacy (eg, lamotrigine, lacosamide), tapentadol, and botulinum toxin. There is some support for analgesic Main message Gabapentinoids, tricyclic combinations in selected NeP conditions. antidepressants, and serotonin-norepinephrine reuptake inhibitors are the first-line agents • Many of these pharmacologic treatments are off-label for pain or for treating neuropathic pain. Tramadol and on-label for specific pain conditions, and these issues should be clearly other opioids are recommended as second- conveyed and documented. -

NMDA Receptor Antagonists for the Treatment of Neuropathic Pain Compared to Placebo: a Systematic Review and Meta-Analysis
Open Journal of Dentistry and Oral Medicine 5(4): 59-71, 2017 http://www.hrpub.org DOI: 10.13189/ojdom.2017.050401 NMDA Receptor Antagonists for the Treatment of Neuropathic Pain Compared to Placebo: A Systematic Review and Meta-analysis Byron Larsen1, Kristin Mau1, Mariela Padilla2, Reyes Enciso3,* 1Master of Science Program in Orofacial Pain and Oral Medicine, Herman Ostrow School of Dentistry, University of Southern California, USA 2Division of Periodontology, Diagnostic Sciences and Dental Hygiene, Herman Ostrow School of Dentistry, University of Southern California, USA 3Division of Dental Public Health and Pediatric Dentistry, Herman Ostrow School of Dentistry, University of Southern California, USA Copyright©2017 by authors, all rights reserved. Authors agree that this article remains permanently open access under the terms of the Creative Commons Attribution License 4.0 International License Abstract The objective of this study is to evaluate the Neuropathic pain has been linked to structural and efficacy of N-Methyl-D-aspartate (NMDA) receptor functional somatosensory nervous system alternations that antagonists on neuropathic pain disorders that can occur in produce spontaneous pain and pathologically intensified the orofacial region. These disorders included: Postherpetic reactions to noxious and innocuous stimuli [1]. It is Neuralgia (PHN), Complex Regional Pain Syndrome suggested that different mechanisms are at play regarding (CRPS), Atypical Odontalgia, Temporomandibular Joint orofacial neuropathic pain due to the diverse clinical (TMJ) Arthralgia and facial neuropathies. Materials and manifestations in disorders of various etiologies [2]. More Methods: Three databases (Medline through PubMed, Web specifically, involvement pertains to both peripheral and of Science, and Cochrane library) were searched on January central sensitization mechanisms [3]. -

The Journal of Rheumatology Volume 75, No. Is Fibromyalgia a Neuropathic Pain Syndrome?
The Journal of Rheumatology Volume 75, no. Is fibromyalgia a neuropathic pain syndrome? Michael C Rowbotham J Rheumatol 2005;75;38-40 http://www.jrheum.org/content/75/38 1. Sign up for TOCs and other alerts http://www.jrheum.org/alerts 2. Information on Subscriptions http://jrheum.com/faq 3. Information on permissions/orders of reprints http://jrheum.com/reprints_permissions The Journal of Rheumatology is a monthly international serial edited by Earl D. Silverman featuring research articles on clinical subjects from scientists working in rheumatology and related fields. Downloaded from www.jrheum.org on September 24, 2021 - Published by The Journal of Rheumatology Is Fibromyalgia a Neuropathic Pain Syndrome? MICHAEL C. ROWBOTHAM ABSTRACT. The fibromyalgia syndrome (FM) seems an unlikely candidate for classification as a neuropathic pain. The disorder is diagnosed based on a compatible history and the presence of multiple areas of musculoskeletal tenderness. A consistent pathology in either the peripheral or central nervous system (CNS) has not been demonstrated in patients with FM, and they are not at higher risk for diseases of the CNS such as multiple sclerosis or of the peripheral nervous system such as peripheral neuropathy. A large proportion of FM suf- ferers have accompanying symptoms and signs of uncertain etiology, such as chronic fatigue, sleep distur- bance, and bowel/bladder irritability. With the exception of migraine headaches and possibly irritable bowel syndrome, the accompanying disorders are clearly not neurological in origin. The impetus to classify the FM as a neuropathic pain comes from multiple lines of research suggesting widespread pain and tenderness are associated with chronic sensitization of the CNS. -

Anxiolytic Activity of Tribulus Terrestris on Elevated Plus Maze
Journal of Applied Pharmaceutical Science Vol. 4 (02), pp. 126-128, February, 2014 Available online at http://www.japsonline.com DOI: 10.7324/JAPS.2014.40220 ISSN 2231-3354 Short Communication Anxiolytic activity of Tribulus terrestris on elevated plus maze Saima Ahmed1, Sualiha Lutfullah2, Izhar Ahmed1, Reshma Farooq3, Javeid Iqbal1 1Department of Pharmacology, Faculty of Pharmacy, Hamdard University, Karachi, Pakistan. 2Dr HMI Institute of Pharmacology and Hebal Sciences, Hamdard University, Karachi, Pakistan. 3Department of Basic Sciences, College of Nursing, Kind Abdul Aziz University, Kingdom of Saudi Arabia. ARTICLE INFO ABSTRACT Article history: Received on: 10/11/2013 Tribulus terrestris widely used in Asian countries as soothing effect and decoration especially in festivals and has Revised on: 25/01/2014 brain calming effect and it reduces behavior related anxiety and psychic behavior in rodents also. Tribulus Accepted on: 10/02/2014 Terrestris extract produce significantly increase time spent in the open arm of plus maze and rearing significantly increase in elevated plus mazes that shows reduction in anxiety behavior. Increase number of entries Available online: 27/02/2014 in open arm significantly shows anxiety relieving capabilities in treated NMRI mice. Key words: Anxiolytic, Tribulus terrestris, elevated plus maze, psychic behavior. INTRODUCTION File, 1986) and behavioral (Lister, 1987; Pellow et al., 1985) manipulations in rodents. Time spent in open areas is frequently Depressive anxiety is one of the most common emotional reported as spent time of treated mice in open arm compared to disorders and treatment of phobias or panic attacks is still not control mice, time spent in the closed and open areas, thereby trivial. -

The Gerbil Elevated Plus-Maze I: Behavioral Characterization and Pharmacological Validation Geoffrey B
The Gerbil Elevated Plus-Maze I: Behavioral Characterization and Pharmacological Validation Geoffrey B. Varty, Ph.D., Cynthia A. Morgan, B.Sc., Mary E. Cohen-Williams, B.Sc., Vicki L. Coffin, Ph.D., and Galen J. Carey, Ph.D. Several neurokinin NK1 receptor antagonists currently produced anxiolytic-like effects on risk-assessment being developed for anxiety and depression have reduced behaviors (reduced stretch-attend postures and increased affinity for the rat and mouse NK1 receptor compared with head dips). Of particular interest, the antidepressant drugs human. Consequently, it has proven difficult to test these imipramine (1–30 mg/kg p.o.), fluoxetine (1–30 mg/kg, p.o.) agents in traditional rat and mouse models of anxiety and and paroxetine (0.3–10 mg/kg p.o.) each produced some depression. This issue has been overcome, in part, by using acute anxiolytic-like activity, without affecting locomotor non-traditional lab species such as the guinea pig and activity. The antipsychotic, haloperidol, and the gerbil, which have NK1 receptors closer in homology to psychostimulant, amphetamine, did not produce any human NK1 receptors. However, there are very few reports anxiolytic-like effects (1–10 mg/kg s.c). The anxiogenic describing the behavior of gerbils in traditional models of -carboline, FG-7142, reduced time spent in the open arm anxiety. The aim of the present study was to determine if the and head dips, and increased stretch-attend postures (1–30 elevated plus-maze, a commonly used anxiety model, could mg/kg, i.p.). These studies have demonstrated that gerbils be adapted for the gerbil. -

Neuropathic Pain (E Eisenberg, Section Editor)
Curr Pain Headache Rep (2017) 21: 28 DOI 10.1007/s11916-017-0629-5 NEUROPATHIC PAIN (E EISENBERG, SECTION EDITOR) Neuropathic Pain: Central vs. Peripheral Mechanisms Kathleen Meacham1,2 & Andrew Shepherd1,2 & Durga P. Mohapatra1,2 & Simon Haroutounian1,2 Published online: 21 April 2017 # Springer Science+Business Media New York 2017 Abstract identify potentially self-sustaining infra-slow CNS oscillatory Purpose of Review Our goal is to examine the processes— activity that may be unique to pNP patients. both central and peripheral—that underlie the development of Summary While new preclinical evidence supports and ex- peripherally-induced neuropathic pain (pNP) and to highlight pands upon the key role of central mechanisms in neuropathic recent evidence for mechanisms contributing to its mainte- pain, clinical evidence for an autonomous central mechanism nance. While many pNP conditions are initiated by damage remains relatively limited. Recent findings from both preclin- to the peripheral nervous system (PNS), their persistence ap- ical and clinical studies recapitulate the critical contribution of pears to rely on maladaptive processes within the central ner- peripheral input to maintenance of neuropathic pain. Further vous system (CNS). The potential existence of an autonomous clinical investigations on the possibility of standalone central pain-generating mechanism in the CNS creates significant im- contributions to pNP may be assisted by a reconsideration of plications for the development of new neuropathic pain treat- the agreed terms or criteria for diagnosing the presence of ments; thus, work towards its resolution is crucial. Here, we central sensitization in humans. seek to identify evidence for PNS and CNS independently generating neuropathic pain signals. -
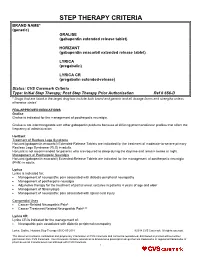
STEP THERAPY CRITERIA BRAND NAME* (Generic) GRALISE (Gabapentin Extended Release Tablet)
STEP THERAPY CRITERIA BRAND NAME* (generic) GRALISE (gabapentin extended release tablet) HORIZANT (gabapentin enacarbil extended release tablet) LYRICA (pregabalin) LYRICA CR (pregabalin extended-release) Status: CVS Caremark Criteria Type: Initial Step Therapy; Post Step Therapy Prior Authorization Ref # 656-D * Drugs that are listed in the target drug box include both brand and generic and all dosage forms and strengths unless otherwise stated FDA-APPROVED INDICATIONS Gralise Gralise is indicated for the management of postherpetic neuralgia. Gralise is not interchangeable with other gabapentin products because of differing pharmacokinetic profiles that affect the frequency of administration. Horizant Treatment of Restless Legs Syndrome Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the treatment of moderate-to-severe primary Restless Legs Syndrome (RLS) in adults. Horizant is not recommended for patients who are required to sleep during the daytime and remain awake at night. Management of Postherpetic Neuralgia Horizant (gabapentin enacarbil) Extended-Release Tablets are indicated for the management of postherpetic neuralgia (PHN) in adults. Lyrica Lyrica is indicated for: Management of neuropathic pain associated with diabetic peripheral neuropathy Management of postherpetic neuralgia Adjunctive therapy for the treatment of partial onset seizures in patients 4 years of age and older Management of fibromyalgia Management of neuropathic pain associated with spinal cord injury Compendial Uses Cancer-Related Neuropathic Pain6 Cancer Treatment Related Neuropathic Pain6,12 Lyrica CR Lyrica CR is indicated for the management of: Neuropathic pain associated with diabetic peripheral neuropathy Lyrica, Gralise, Horizant Step Therapy 656-D 05-2018 ©2018 CVS Caremark. All rights reserved. This document contains confidential and proprietary information of CVS Caremark and cannot be reproduced, distributed or printed without written permission from CVS Caremark. -

Elevated Mazes As Animal Models of Anxiety: Effects of Serotonergic Agents
Anais da Academia Brasileira de Ciências (2007) 79(1): 71-85 (Annals of the Brazilian Academy of Sciences) ISSN 0001-3765 www.scielo.br/aabc Elevated mazes as animal models of anxiety: effects of serotonergic agents SIMONE H. PINHEIRO1, HÉLIO ZANGROSSI-Jr.2, CRISTINA M. DEL-BEN1 and FREDERICO G. GRAEFF1 1Departamento de Neurologia, Psiquiatria e Psicologia Médica, Hospital das Clínicas Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo Avenida Bandeirantes 3.900, 14048-900 Ribeirão Preto, SP, Brasil 2Departamento de Farmacologia, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo Avenida Bandeirantes 3.900, 14049-900 Ribeirão Preto, SP, Brasil Manuscript received on March 23, 2006; accepted for publication on April 12, 2006; contributed by FREDERICO G. GRAEFF* ABSTRACT This article reviews reported results about the effects of drugs that act upon the serotonergic neurotransmission mea- sured in three elevated mazes that are animal models of anxiety. A bibliographic search has been performed in MED- LINE using different combinations of the key words X-maze, plus-maze, T-maze, serotonin and 5-HT, present in the title and/or the abstract, with no time limit. From the obtained abstracts, several publications were excluded on the basis of the following criteria: review articles that did not report original results, species other than the rat, intracerebral drug administration alone, genetically manipulated rats, and animals having any kind of experimental pathology. The reported results indicate that the effect of drugs on the inhibitory avoidance task performed in the elevated T-maze and on the spatio temporal indexes of anxiety measured in the X and plus mazes correlate with their effect in patients diagnosed with generalized anxiety disorder. -

Pharmacotherapy of Neuropathic Pain: Which Drugs, Which Treatment Algorithms? Nadine Attal*, Didier Bouhassira
Biennial Review of Pain Pharmacotherapy of neuropathic pain: which drugs, which treatment algorithms? Nadine Attal*, Didier Bouhassira Abstract Neuropathic pain (NP) is a significant medical and socioeconomic burden. Epidemiological surveys have indicated that many patients with NP do not receive appropriate treatment for their pain. A number of pharmacological agents have been found to be effective in NP on the basis of randomized controlled trials including, in particular, tricyclic antidepressants, serotonin and norepinephrine reuptake inhibitor antidepressants, pregabalin, gabapentin, opioids, lidocaine patches, and capsaicin high- concentration patches. Evidence-based recommendations for the pharmacotherapy of NP have recently been updated. However, meta-analyses indicate that only a minority of patients with NP have an adequate response to drug therapy. Several reasons may account for these findings, including a modest efficacy of the active drugs, a high placebo response, the heterogeneity of diagnostic criteria for NP, and an inadequate classification of patients in clinical trials. Improving the current way of conducting clinical trials in NP could contribute to reduce therapeutic failures and may have an impact on future therapeutic algorithms. Keywords: Neuropathic pain, Pharmacotherapy, Clinical trials, Therapeutic algorithms, Phenotypic subgrouping 1. Introduction Here, we briefly present the major pharmacological treatments studied in NP and the latest therapeutic recommendations for Neuropathic pain (NP) is estimated to affect as much as 7% of the general population in European countries19,83 and induces their use. We then outline the difficulties associated with a specific disease burden in patients.6,30,83 It is now considered pharmacotherapy of NP in clinical trials and draw prospects for as a clinical entity regardless of the underlying etiology.4 Epidemi- future drug trials and therapeutic algorithms. -

Intervention Mechanism of Repeated Oral GABA Administration on Anxiety- Like Behaviors Induced by Emotional Stress in Rats T
Psychiatry Research 271 (2019) 649–657 Contents lists available at ScienceDirect Psychiatry Research journal homepage: www.elsevier.com/locate/psychres Intervention mechanism of repeated oral GABA administration on anxiety- like behaviors induced by emotional stress in rats T He Yongjiana,b,#, Ouyang Junyana,b,#, Hu Zhuoyana, Yang Jiea,b, Chu Yuea,b, Huang Shaowena,b, ⁎ Yang Yichaoc, Liu Chunhonga,b, a College of Food Science, South China Agricultural University, Guangzhou, GZ, China b Guangdong Provincial Key Laboratory of Food Quality and Safety, South China Agricultural University, Guangzhou 510642, China c School of Public Health, Guangzhou Medical University, Guangzhou, GZ, China ARTICLE INFO ABSTRACT Keywords: The purpose of this study was to investigate the effects and mechanism of repeated oral administration of GABA gamma-aminobutyric acid (GABA) on anxiety-like behaviors induced by emotional stress. Male Sprague-Dawley Emotional stress rats were randomly divided into five groups (8 rats each): control, emotional stress model, three emotional Nitric oxide stress + GABA-treated groups (0.5, 1, 2 mg/kg). The rats were given empty water bottles after the training of Anxiety-like behaviors drinking water to induce emotional stress. Each group was treated with saline or different doses of GABA re- OF spectively for 21 consecutive days. Then open field and elevated plus maze were used to assess anxiety-like EPM behaviors. Both frontal cortex and plasma NO metabolites nitrate and nitrite (NOx) levels were determined spectrophotometrically. Results showed that oral administration of GABA significantly reversed the stress-in- duced anxiety-like negative responses dose-dependently. The frontal cortex NOx levels were lower in stressed rats than in control group (P < 0.05), but higher in 2 mg/kg GABA-treated group than stress model group (P < 0.05).