Gene Dosage and the Escape from X Chromosome Inactivation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unc93b Antibody (Pab)
21.10.2014Unc93b antibody (pAb) Rabbit Anti -Human/Mouse/Rat Unc93b Instruction Manual Catalog Number PK-AB718-4553 Synonyms Unc93b Antibody: Unc93b1, homolog of C. elegans Unc93 Description The endoplasmic reticulum (ER) protein Unc93b, a human homolog of the C. elegans Unc93 gene, was initially identified by a forward genetic screen using N-ethyl-N-nitrosourea where a histidine- to-arginine substitution in Unc93b caused defects in Toll-like receptor (TLR) 3, 7 and 9 signaling. Unlike Unc93a, another homolog of the C. elegans Unc93 gene whose function is unknown, Unc93b specifically interacts with TLR3, 7 and 9; the histidine-to-arginine point mutation used to identify Unc93b abolishes this interaction. Mice carrying this point mutation are highly susceptible to infection with a number of viruses, indicating that Unc93b plays an important role in innate immunity. Multiple isoforms of Unc93a are known to exist. This antibody will not cross-react with Unc93a. Quantity 100 µg Source / Host Rabbit Immunogen Unc93b antibody was raised in rabbits against a 19 amino acid peptide from near the amino terminus of human Unc93b. Purification Method Affinity chromatography purified via peptide column. Clone / IgG Subtype Polyclonal antibody Species Reactivity Human, Mouse, Rat Specificity Multiple isoforms of Unc93a are known to exist. This antibody will not cross-react with Unc93a. Formulation Antibody is supplied in PBS containing 0.02% sodium azide. Reconstitution During shipment, small volumes of antibody will occasionally become entrapped in the seal of the product vial. For products with volumes of 200 μl or less, we recommend gently tapping the vial on a hard surface or briefly centrifuging the vial in a tabletop centrifuge to dislodge any liquid in the container’s cap. -

Variants Affecting the C-Terminal Tail of UNC93B1 Are Not a Common Risk Factor for Systemic Lupus Erythematosus
G C A T T A C G G C A T genes Article Variants Affecting the C-Terminal Tail of UNC93B1 Are Not a Common Risk Factor for Systemic Lupus Erythematosus Sarah Kiener 1,2 , Camillo Ribi 3 , Irene Keller 4, Carlo Chizzolini 5 , Marten Trendelenburg 6, Uyen Huynh-Do 7 , Johannes von Kempis 8, on behalf of Swiss SLE Cohort Study (SSCS) † and Tosso Leeb 1,2,* 1 Institute of Genetics, Vetsuisse Faculty, University of Bern, 3012 Bern, Switzerland; [email protected] 2 Dermfocus, University of Bern, 3001 Bern, Switzerland 3 Division of Immunology and Allergy, Department of Medicine, Lausanne University Hospital (CHUV) and University of Lausanne (UNIL), 1011 Lausanne, Switzerland; [email protected] 4 Interfaculty Bioinformatics Unit, University of Bern, 3012 Bern, Switzerland; [email protected] 5 Department of Pathology and Immunology, School of Medicine, Geneva University, 1211 Geneva, Switzerland; [email protected] 6 Laboratory for Clinical Immunology, Department of Biomedicine and Division of Internal Medicine, University Hospital of Basel, 4031 Basel, Switzerland; [email protected] 7 Division of Nephrology and Hypertension, Inselspital, Bern University Hospital, 3010 Bern, Switzerland; [email protected] 8 Division of Rheumatology, Cantonal Hospital St. Gallen, 9007 St. Gallen, Switzerland; [email protected] * Correspondence: [email protected]; Tel.: +41-31-684-2326 † Association of the Swiss SLE Cohort Study (ASSCS), 4031 Basel, Switzerland. Citation: Kiener, S.; Ribi, C.; Keller, I.; Abstract: Systemic lupus erythematosus (SLE) is a heterogeneous multifactorial disease. Upregulated Chizzolini, C.; Trendelenburg, M.; TLR7 signaling is a known risk factor for SLE. -

Functional Characterization of a Novel ENU-Induced Mutation In
Functional characterization of a novel ENU‐induced mutation in Unc93b1 and its role in single‐stranded RNA virus infection Erin Isabel Lafferty Division of Experimental Medicine McGill University, Montréal April 2014 A thesis submitted to McGill University in partial fulfillment of the requirements of the degree of Doctor of Philosophy © Erin Isabel Lafferty, 2014 Acknowledgements I would like to thank my supervisor Dr. Salman Qureshi for providing me with the opportunity, tools, and guidance to tackle this stimulating project and for always challenging me to achieve excellence. In addition, I would like to thank the members of my supervisory committee, Dr. Silvia Vidal, Dr. Ciriaco Piccirillo, and Dr. Danuta Radzioch, for helpful advice both during and between my yearly committee meetings. I would also like to thank all manuscript co‐authors, in particular Adam Flaczyk and Sean Wiltshire, for their technical, intellectual, and editorial contributions. A big thank you to past and present members of the Qureshi Lab for experimental and general support and to members of the MGH L11 for smiles in the hall and lunchtime conversations. In particular, thank you to Dr. Scott Carroll for teaching me how to be a PhD student and Isabelle Angers for her technical expertise, friendship, and French translation skills. Thank you to the people I have met and worked with through SKILLSETS, Let’s Talk Science, and the PGSS Equity Committee for your friendship and advice on life, careers, and graduate school; with special thanks to my thesis writing buddy Heather. To my incredible friends who live near and far; Carolyn, Monique, Sophia, Marie‐Claire, Iona, and many more; you have been beside me through so much, both in person and on the phone/over Skype. -

Atypical Solute Carriers
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1346 Atypical Solute Carriers Identification, evolutionary conservation, structure and histology of novel membrane-bound transporters EMELIE PERLAND ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-513-0015-3 UPPSALA urn:nbn:se:uu:diva-324206 2017 Dissertation presented at Uppsala University to be publicly examined in B22, BMC, Husargatan 3, Uppsala, Friday, 22 September 2017 at 10:15 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in English. Faculty examiner: Professor Carsten Uhd Nielsen (Syddanskt universitet, Department of Physics, Chemistry and Pharmacy). Abstract Perland, E. 2017. Atypical Solute Carriers. Identification, evolutionary conservation, structure and histology of novel membrane-bound transporters. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1346. 49 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0015-3. Solute carriers (SLCs) constitute the largest family of membrane-bound transporter proteins in humans, and they convey transport of nutrients, ions, drugs and waste over cellular membranes via facilitative diffusion, co-transport or exchange. Several SLCs are associated with diseases and their location in membranes and specific substrate transport makes them excellent as drug targets. However, as 30 % of the 430 identified SLCs are still orphans, there are yet numerous opportunities to explain diseases and discover potential drug targets. Among the novel proteins are 29 atypical SLCs of major facilitator superfamily (MFS) type. These share evolutionary history with the remaining SLCs, but are orphans regarding expression, structure and/or function. They are not classified into any of the existing 52 SLC families. -

TLR7 Trafficking and Signaling in B Cells Is Regulated by the MHCII-Associated Invariant Chain
© 2020. Published by The Company of Biologists Ltd | Journal of Cell Science (2020) 133, jcs236711. doi:10.1242/jcs.236711 RESEARCH ARTICLE SPECIAL ISSUE: CELL BIOLOGY OF THE IMMUNE SYSTEM TLR7 trafficking and signaling in B cells is regulated by the MHCII-associated invariant chain Mira Tohme1, Lucie Maisonneuve2,3, Karim Achour4, Michaël Dussiot5, Sophia Maschalidi6 and Bénédicte Manoury2,3,* ABSTRACT respectively. The localization, traffic and folding of intracellular Toll-like receptor 7 (TLR7) is an endosomal receptor that recognizes TLRs are regulated by the endoplasmic reticulum (ER)-resident single-stranded RNA from viruses. Its trafficking and activation is protein UNC93B1 (Tabeta et al., 2006; Brinkmann et al., 2007; regulated by the endoplasmic reticulum (ER) chaperone UNC93B1 Pelka et al., 2018; Majer et al., 2019). UNC93B1 binds directly to and lysosomal proteases. UNC93B1 also modulates major the transmembrane region of TLR3, TLR7, TLR8 and TLR9 in the histocompatibility complex class II (MHCII) antigen presentation, ER and transports them to endocytic compartments upon and deficiency in MHCII protein diminishes TLR9 signaling. These stimulation (Kim et al., 2008). In dendritic cells (DCs) purified results indicate a link between proteins that regulate both innate and from mice expressing a point mutation in UNC93B1 (3d), adaptive responses. Here, we report that TLR7 resides in lysosomes intracellular TLRs are retained in the ER, preventing DCs from and interacts with the MHCII-chaperone molecule, the invariant chain secreting cytokines upon engagement of TLR3, TLR7 and TLR9 (Ii) or CD74, in B cells. In the absence of CD74, TLR7 displays both (Tabeta et al., 2006). However, in B cells, even though UNC93B1 is ER and lysosomal localization, leading to an increase in pro- still required for intracellular TLR signaling, TLR9 seems, at the inflammatory cytokine production. -

Single-Cell Transcriptomes Reveal a Complex Cellular Landscape in the Middle Ear and Differential Capacities for Acute Response to Infection
fgene-11-00358 April 9, 2020 Time: 15:55 # 1 ORIGINAL RESEARCH published: 15 April 2020 doi: 10.3389/fgene.2020.00358 Single-Cell Transcriptomes Reveal a Complex Cellular Landscape in the Middle Ear and Differential Capacities for Acute Response to Infection Allen F. Ryan1*, Chanond A. Nasamran2, Kwang Pak1, Clara Draf1, Kathleen M. Fisch2, Nicholas Webster3 and Arwa Kurabi1 1 Departments of Surgery/Otolaryngology, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States, 2 Medicine/Center for Computational Biology & Bioinformatics, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States, 3 Medicine/Endocrinology, UC San Diego School of Medicine, VA Medical Center, La Jolla, CA, United States Single-cell transcriptomics was used to profile cells of the normal murine middle ear. Clustering analysis of 6770 transcriptomes identified 17 cell clusters corresponding to distinct cell types: five epithelial, three stromal, three lymphocyte, two monocyte, Edited by: two endothelial, one pericyte and one melanocyte cluster. Within some clusters, Amélie Bonnefond, Institut National de la Santé et de la cell subtypes were identified. While many corresponded to those cell types known Recherche Médicale (INSERM), from prior studies, several novel types or subtypes were noted. The results indicate France unexpected cellular diversity within the resting middle ear mucosa. The resolution of Reviewed by: Fabien Delahaye, uncomplicated, acute, otitis media is too rapid for cognate immunity to play a major Institut Pasteur de Lille, France role. Thus innate immunity is likely responsible for normal recovery from middle ear Nelson L. S. Tang, infection. The need for rapid response to pathogens suggests that innate immune The Chinese University of Hong Kong, China genes may be constitutively expressed by middle ear cells. -

SUPPLEMENTARY MATERIAL Supplementary Fig. S1. LD Mice Used in This Study Accumulate Polyglucosan Inclusions (Lafora Bodies) in the Brain
1 SUPPLEMENTARY MATERIAL Supplementary Fig. S1. LD mice used in this study accumulate polyglucosan inclusions (Lafora bodies) in the brain. Samples from the hippocampus of five months old control, Epm2a-/- (lacking laforin) and Epm2b-/- mice (lacking malin) were stained with periodic acid Schiff reagent (PAS staining), which colors polysaccharide granules in red. Bar: 50 m. Supplementary Fig. S2. Principal component analysis (PCA) representing the first two components with the biggest level of phenotypic variability. Samples 1_S1 to 4_S4 corresponded to control, 5_S5, 6_S6 and 8_S8 to Epm2a-/- and 9_S9 to 12_S12 to Epm2b- /- samples, of animals of 16 months of age respectively. Supplementary Table S1. Primers used in this work to validate the expression of the corresponding genes by RT-qPCR. Supplementary Table S2: Genes downregulated more than 0.5 fold in Epm2a-/- and Epm2b-/- mice of 16 months of age. The gene name, false discovery rate (FDR), fold change (FC), description and MGI Id (mouse genome informatics) are indicated. Genes are arranged according to FC. Supplementary Table S3: Genes upregulated more than 1.5 fold in Epm2a-/- mice of 16 months of age. The gene name, false discovery rate (FDR), fold change (FC), description and MGI Id (mouse genome informatics) are indicated. Genes are arranged according to FC. Supplementary Table S4: Genes upregulated more than 1.5 fold in Epm2b-/- mice of 16 months of age. The gene name, false discovery rate (FDR), fold change (FC), description and MGI Id (mouse genome informatics) are indicated. Genes are arranged according to FC. 2 Supplementary Table S5: Genes upregulated in both Epm2a-/- and Epm2b-/- mice of 16 months of age. -
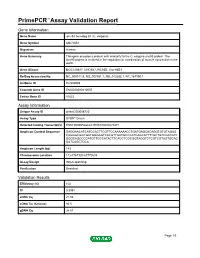
Primepcr™Assay Validation Report
PrimePCR™Assay Validation Report Gene Information Gene Name unc-93 homolog B1 (C. elegans) Gene Symbol UNC93B1 Organism Human Gene Summary This gene encodes a protein with similarity to the C. elegans unc93 protein. The Unc93 protein is involved in the regulation or coordination of muscle contraction in the worm. Gene Aliases MGC126617, UNC93, UNC93B, Unc-93B1 RefSeq Accession No. NC_000011.9, NG_007581.1, NG_012282.1, NT_167190.1 UniGene ID Hs.502989 Ensembl Gene ID ENSG00000110057 Entrez Gene ID 81622 Assay Information Unique Assay ID qHsaCID0008720 Assay Type SYBR® Green Detected Coding Transcript(s) ENST00000528423, ENST00000227471 Amplicon Context Sequence GAGGAACATCATCCACTTCGTTCCAAAAAACCTGATGAGCACAGGTGTGTAGAG CAGGGCGGCGATGGGAGTCACGTTGATGCCCATCAGCATTTTGCTGTCGATGTC GGGCAGCCCCATGTTGCCATACTTCACCTCGCGGTAGGTCTCGTCGTAGTGCAG GATCAGCTGCA Amplicon Length (bp) 143 Chromosome Location 11:67767120-67770633 Assay Design Intron-spanning Purification Desalted Validation Results Efficiency (%) 102 R2 0.9991 cDNA Cq 21.08 cDNA Tm (Celsius) 86.5 gDNA Cq 34.51 Page 1/5 PrimePCR™Assay Validation Report Specificity (%) 100 Information to assist with data interpretation is provided at the end of this report. Page 2/5 PrimePCR™Assay Validation Report UNC93B1, Human Amplification Plot Amplification of cDNA generated from 25 ng of universal reference RNA Melt Peak Melt curve analysis of above amplification Standard Curve Standard curve generated using 20 million copies of template diluted 10-fold to 20 copies Page 3/5 PrimePCR™Assay Validation Report Products used to generate validation data Real-Time PCR Instrument CFX384 Real-Time PCR Detection System Reverse Transcription Reagent iScript™ Advanced cDNA Synthesis Kit for RT-qPCR Real-Time PCR Supermix SsoAdvanced™ SYBR® Green Supermix Experimental Sample qPCR Human Reference Total RNA Data Interpretation Unique Assay ID This is a unique identifier that can be used to identify the assay in the literature and online. -

Toll-Like Receptor Signaling in the Establishment and Function of the Immune System
cells Review Toll-Like Receptor Signaling in the Establishment and Function of the Immune System Jahnavi Aluri, Megan A. Cooper and Laura G. Schuettpelz * Department of Pediatrics, Washington University School of Medicine, St. Louis, MO 63110, USA; [email protected] (J.A.); [email protected] (M.A.C.) * Correspondence: [email protected]; Tel.: +1-314-286-1813; Fax: +1-314-286-2893 Abstract: Toll-like receptors (TLRs) are pattern recognition receptors that play a central role in the development and function of the immune system. TLR signaling promotes the earliest emergence of hematopoietic cells during development, and thereafter influences the fate and function of both primitive and effector immune cell types. Aberrant TLR signaling is associated with hematopoietic and immune system dysfunction, and both loss- and gain-of- function variants in TLR signaling- associated genes have been linked to specific infection susceptibilities and immune defects. Herein, we will review the role of TLR signaling in immune system development and the growing number of heritable defects in TLR signaling that lead to inborn errors of immunity. Keywords: TLR; immune system; inborn errors of immunity 1. Introduction Citation: Aluri, J.; Cooper, M.A.; Toll-like receptors (TLRs) are a family of pattern recognition receptors that play a Schuettpelz, L.G. Toll-Like Receptor significant role in the development and maintenance of the immune system. These receptors Signaling in the Establishment and recognize a wide variety of pathogens, as well as endogenous ligands associated with Function of the Immune System. Cells cellular damage. Signaling through TLRs leads to the production of proinflammatory 2021, 10, 1374. -

TLR8 on Dendritic Cells and TLR9 on B Cells Restrain TLR7-Mediated Spontaneous Autoimmunity in C57BL/6 Mice
TLR8 on dendritic cells and TLR9 on B cells restrain TLR7-mediated spontaneous autoimmunity in C57BL/6 mice Benoit Desnuesa,b,c,1, Amanda Beatriz Macedoa,b,c,1, Annie Roussel-Quevala,b,c, Johnny Bonnardela,b,c, Sandrine Henria,b,c, Olivier Demariaa,b,c,2, and Lena Alexopouloua,b,c,3 aCentre d’Immunologie de Marseille-Luminy, Aix-Marseille University UM 2, 13288 Marseille, France; bInstitut National de la Santé et de la Recherche Médicale, Unité Mixte de Recherche 1104, 13288 Marseille, France; and cCentre National de la Recherche Scientifique, Unité Mixte de Recherche 7280, 13288 Marseille, France Edited* by Richard A. Flavell, Yale School of Medicine, Howard Hughes Medical Institute, New Haven, CT, and approved December 18, 2013 (received for review August 5, 2013) Systemic lupus erythematosus (SLE) is a complex autoimmune endosomal localization isolate TLR3, TLR7, TLR8, and disease with diverse clinical presentations characterized by the TLR9 away from self-nucleic acids in the extracellular space, still presence of autoantibodies to nuclear components. Toll-like re- self-RNA or -DNA can become a potent trigger of cell activation ceptor (TLR)7, TLR8, and TLR9 sense microbial or endogenous nucleic when transported into TLR-containing endosomes, and such acids and are implicated in the development of SLE. In mice TLR7- recognition can result in sterile inflammation and autoimmunity, deficiency ameliorates SLE, but TLR8- or TLR9-deficiency exacerbates including SLE (4, 15, 16). The connection of the endosomal the disease because of increased TLR7 response. Thus, both TLR8 TLRs with SLE originates mainly from mouse models, where and TLR9 control TLR7 function, but whether TLR8 and TLR9 act in TLR7 signaling seems to play a central role. -

Reticulum Via Association with UNC93B1 Sensing Tlrs from The
LRRC59 Regulates Trafficking of Nucleic Acid−Sensing TLRs from the Endoplasmic Reticulum via Association with UNC93B1 This information is current as Megumi Tatematsu, Kenji Funami, Noriko Ishii, Tsukasa of October 1, 2021. Seya, Chikashi Obuse and Misako Matsumoto J Immunol 2015; 195:4933-4942; Prepublished online 14 October 2015; doi: 10.4049/jimmunol.1501305 http://www.jimmunol.org/content/195/10/4933 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2015/10/14/jimmunol.150130 Material 5.DCSupplemental http://www.jimmunol.org/ References This article cites 37 articles, 15 of which you can access for free at: http://www.jimmunol.org/content/195/10/4933.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on October 1, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2015 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology LRRC59 Regulates Trafficking of Nucleic Acid–Sensing TLRs from the Endoplasmic Reticulum via Association with UNC93B1 Megumi Tatematsu,* Kenji Funami,* Noriko Ishii,* Tsukasa Seya,* Chikashi Obuse,† and Misako Matsumoto* Compartmentalization of nucleic acid (NA)–sensing TLR3, 7, 8, and 9 is strictly regulated to direct optimal response against microbial infection and evade recognition of host-derived NAs. -

An in Vivo Atlas of Host–Pathogen Transcriptomes During Streptococcus Pneumoniae Colonization and Disease
An in vivo atlas of host–pathogen transcriptomes during Streptococcus pneumoniae colonization and disease Adonis D’Melloa, Ashleigh N. Rieglerb, Eriel Martínezb, Sarah M. Benob, Tiffany D. Rickettsb, Ellen F. Foxmanc, Carlos J. Orihuelab,1, and Hervé Tettelina,1,2 aDepartment of Microbiology and Immunology, Institute for Genome Sciences, University of Maryland School of Medicine, Baltimore, MD 21201; bDepartment of Microbiology, University of Alabama at Birmingham, Birmingham, AL 35294; and cDepartment of Laboratory Medicine, Yale University School of Medicine, New Haven, CT 06520 Edited by Ralph R. Isberg, Tufts University School of Medicine, Boston, MA, and approved November 6, 2020 (received for review May 24, 2020) Streptococcus pneumoniae (Spn) colonizes the nasopharynx and consideration for anatomical site-specific differences. One approach can cause pneumonia. From the lungs it spreads to the blood- was the use of signature tagged mutagenesis to identify mutants that stream and causes organ damage. We characterized the in vivo are unable to replicate in vivo in an anatomical site-specific manner Spn and mouse transcriptomes within the nasopharynx, lungs, (10). Accompanying studies using microarrays to examine in vivo blood, heart, and kidneys using three Spn strains. We identified isolated RNA from the bacteria indicated that Spn gene expression Spn genes highly expressed at all anatomical sites and in an organ- varies according to the host site (11). Other RNA-sequencing specific manner; highly expressed genes were shown to have vital (RNA-seq) studies have also focused on the host response within roles with knockout mutants. The in vivo bacterial transcriptome the lungs upon pneumococcal infection. These have identified key during colonization/disease was distinct from previously reported genes involved in neutrophil recruitment and response to diverse Spn in vitro transcriptomes.