Onychomadesis Following Gianotti-Crosti Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Concurrent Beau Lines, Onychomadesis, and Retronychia Following Scurvy
CASE REPORT Concurrent Beau Lines, Onychomadesis, and Retronychia Following Scurvy Dayoung Ko, BS; Shari R. Lipner, MD, PhD the proximal nail plate from the distal nail plate leading to shedding of the nail. It occurs due to a complete growth PRACTICE POINTS arrest in the nail matrix and is thought to be on a con- • Beau lines, onychomadesis, and retronychia are nail tinuum with Beau lines. The etiologies of these 2 condi- conditions with distinct clinical findings. tions overlap and include trauma, inflammatory diseases, • Beau lines and onychomadesis may be seen 1-5 concurrently following trauma, inflammatory dis- systemic illnesses, hereditary conditions, and infections. eases, systemic illnesses, hereditary conditions, In almost all cases of both conditions, normal nail plate and infections. production ensues upon identification and removal of the 3,4,6 • Retronychia shares a common pathophysiology inciting agent or recuperation from the causal illness. with Beau lines and onychomadesis, and all reflect Beau lines will move distally as the nail grows out and slowing or cessation of nail plate production. can be clipped. In onychomadesis, the affected nails will be shed with time. Resolution of these nail defects can be estimated from average nail growth rates (1 mm/mo for fingernails and 2–3 mm/mo for toenails).7 Beau lines, onychomadesis, and retronychia are nail conditions with Retronychia is defined as a proximal ingrowing of their own characteristic clinical findings. It has been hypothesized the nail plate into the ventral surface of the proximal nail that these 3 disorders may share a common pathophysiologic fold.4,6 It is thought to occur via vertical progression of mechanism of slowing and/or halting nail plate production at the the nail plate into the proximal nail fold, repetitive nail nail matrix. -

Truncal Rashes Stan L
Healthy Baby Practical advice for treating newborns and toddlers. Getting Truculent with Truncal Rashes Stan L. Block, MD, FAAP A B C All images courtesy of Stan L. Block, MD, FAAP. Figure 1. Afebrile 22-month-old white male presents to your office with this slowly spreading, somewhat generalized, and refractory truncal rash for the past 4 weeks. It initially started on the right side of his trunk (A) and later extended down his right upper thigh (B). The rash has now spread to the contralateral side on his back (C), and is most confluent and thickest over his right lateral ribs. n a daily basis, we pediatricians would not be readily able to identify this rash initially began on the right side of his encounter a multitude of rashes relatively newly described truncal rash trunk (see Figure 1A) and then extended O of varied appearance in children shown in some of the following cases. distally down to his right upper thigh (see of all ages. Most of us gently-seasoned As is typical, certain clues are critical, Figure 1B). Although the rash is now dis- clinicians have seen nearly all versions including the child’s age, the duration tributed over most of his back (see Figure of these “typical” rashes. Yet, I venture and the distribution of the rash. Several 1C), it is most confluent and most dense to guess that many practitioners, who of these rashes notably mimic more com- over his right lateral ribs. would be in good company with some of mon etiologies, as discussed in some of From Figure 1, you could speculate my quite erudite partners (whom I asked), the following cases. -

Tips for Managing Treatment-Related Rash and Dry Skin
RASH Tips for Managing Treatment-Related Rash and Dry Skin Presented by Stewart B. Fleishman, MD Continuum Cancer Centers of New York: Beth Israel & St. Luke’s-Roosevelt Lindy P. Fox, MD University of California San Francisco David H. Garfield, MD University of Colorado Comprehensive Cancer Center Carol S. Viele, RN, MS University of California San Francisco Carolyn Messner, DSW CancerCare Learn about: • Effects of targeted treatments on the skin • Managing rashes and dry skin • Treating nail conditions • Your support team Help and Hope CancerCare is a national nonprofit organization that provides free support services to anyone affected by cancer: people with cancer, caregivers, children, loved ones, and the bereaved. CancerCare programs—including counseling and support groups, education, financial assistance, and practical help—are provided by professional oncology social workers and are completely free of charge. Founded in 1944, CancerCare provided individual help to more than 100,000 people last year and had more than 1 million unique visitors to our websites. For more information, call 1-800-813-HOPE (4673) or visit www.cancercare.org. Contacting CancerCare National Office Administration CancerCare Tel: 212-712-8400 The material presented in this patient booklet is provided for your general 275 Seventh Avenue Fax: 212-712-8495 information only. It is not intended as medical advice and should not be relied New York, NY 10001 Email: [email protected] upon as a substitute for consultations with qualified health professionals who Email: [email protected] Website: www.cancercare.org are aware of your specific situation. We encourage you to take information and Services questions back to your individual health care provider as a way of creating a Tel: 212-712-8080 dialogue and partnership about your cancer and your treatment. -

Drug Eruptions- When to Worry
3/17/2017 Drug reactions: Drug Eruptions‐ When to Worry 3 things you need to know 1. Type of drug reaction 2. Statistics: – Which drugs are most likely to cause that type of Lindy P. Fox, MD reaction? Associate Professor 3. Timing: Director, Hospital Consultation Service – How long after the drug started did the reaction Department of Dermatology University of California, San Francisco begin? [email protected] I have no conflicts of interest to disclose 1 Drug Eruptions: Common Causes of Cutaneous Drug Degrees of Severity Eruptions • Antibiotics Simple Complex • NSAIDs Morbilliform drug eruption Drug hypersensitivity reaction Stevens-Johnson syndrome •Sulfa (SJS) Toxic epidermal necrolysis (TEN) • Allopurinol Minimal systemic symptoms Systemic involvement • Anticonvulsants Potentially life threatening 1 3/17/2017 Morbilliform (Simple) Drug Eruption Morbilliform (Simple) Drug Eruption Per the drug chart, the most likely culprit is: Per the drug chart, the most likely culprit is: Day Day Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 A vancomycin x x x x A vancomycin x x x x B metronidazole x x B metronidazole x x C ceftriaxone x x x C ceftriaxone x x x D norepinephrine x x x D norepinephrine x x x E omeprazole x x x x E omeprazole x x x x F SQ heparin x x x x F SQ heparin x x x x trimethoprim/ trimethoprim/ G xxxxxxx G xxxxxxx sulfamethoxazole sulfamethoxazole Admit day Rash onset Admit day Rash onset Morbilliform (Simple) Drug Eruption Drug Induced Hypersensitivity Syndrome • Begins 5‐10 days after drug started -

Cutaneous Manifestations of Systemic Disease
Cutaneous Manifestations of Systemic Disease Dr. Lloyd J. Cleaver D.O. FAOCD FAAD Northeast Regional Medical Center A.T.Still University/KCOM Assistant Vice President/Professor ACOI Board Review Disclosure I have no financial relationships to disclose I will not discuss off label use and/or investigational use in my presentation I do not have direct knowledge of AOBIM questions I have been granted approvial by the AOA to do this board review Dermatology on the AOBIM ”1-4%” of exam is Dermatology Table of Test Specifications is unavailable Review Syllabus for Internal Medicine Large amount of information Cutaneous Multisystem Cutaneous Connective Tissue Conditions Connective Tissue Diease Discoid Lupus Erythematosus Subacute Cutaneous LE Systemic Lupus Erythematosus Scleroderma CREST Syndrome Dermatomyositis Lupus Erythematosus Spectrum from cutaneous to severe systemic involvement Discoid LE (DLE) / Chronic Cutaneous Subacute Cutaneous LE (SCLE) Systemic LE (SLE) Cutaneous findings common in all forms Related to autoimmunity Discoid LE (Chronic Cutaneous LE) Primarily cutaneous Scaly, erythematous, atrophic plaques with sharp margins, telangiectasias and follicular plugging Possible elevated ESR, anemia or leukopenia Progression to SLE only 1-2% Heals with scarring, atrophy and dyspigmentation 5% ANA positive Discoid LE (Chronic Cutaneous LE) Scaly, atrophic plaques with defined margins Discoid LE (Chronic Cutaneous LE) Scaly, erythematous plaques with scarring, atrophy, dyspigmentation DISCOID LUPUS Subacute Cutaneous -

DRESS Syndrome: Improvement of Acute Kidney Injury and Rash with Corticosteroids Dawnielle Endly, DO,* Jonathan Alterie, BS,** David Esguerra, DO,*** Richard A
DRESS Syndrome: Improvement of Acute Kidney Injury and Rash with Corticosteroids Dawnielle Endly, DO,* Jonathan Alterie, BS,** David Esguerra, DO,*** Richard A. Miller, DO**** *Co-lead Author, Dermatology Resident, Nova Southeastern University College of Osteopathic Medicine/Largo Medical Center, Largo, FL **Co-lead Author, 4th-year Medical Student, Chicago College of Osteopathic Medicine, Chicago, IL ***Clinical Professor, Nova Southeastern University College of Osteopathic Medicine, Largo, FL ****Program Director, Dermatology Residency Program, Nova Southeastern University College of Osteopathic Medicine/Largo Medical Center, Largo, FL Abstract DRESS syndrome (drug rash with eosinophilia and systemic symptoms) is a rare and potentially life-threatening idiosyncratic drug reaction that may involve a number of visceral organs. This syndrome often mimics other serious systemic disease processes, making the diagnosis complicated and often delayed. Herein, we present a unique case of DRESS syndrome accompanied by acute interstitial nephritis that responded to oral prednisone during a hospital stay. Introduction superficial dermis. The patient reported minimal negative. An echocardiogram revealed a decrease DRESS syndrome is a drug reaction that symptomatic relief, but the rash progressed and in EF from 25% at baseline to 10% to 20% with usually manifests with fever, a pruritic macular became generalized with total body involvement. severe diffuse hypokinesis and severe biatrial and papular rash, hematologic abnormalities Due to clinical suspicion for a cutaneous drug enlargement. All clinical data was entered into (leukocytosis, eosinophilia, and/or atypical reaction, her primary care provider stopped the the RegiSCAR group diagnosis chart for DRESS lymphocytes), and internal organ involvement. furosemide and prescribed spironolactone a few syndrome and revealed a total of 7 (see Table 1), This drug reaction is characterized by a delayed days prior to her hospitalization. -

Prevention and Treatment of Acneiform Rash in Patients Treated with EGFR Inhibitor Therapies Effective Date: November, 2020
Guideline Resource Unit [email protected] Prevention and Treatment of Acneiform Rash in Patients Treated with EGFR Inhibitor Therapies Effective Date: November, 2020 Clinical Practice Guideline SUPP-003 – Version 2 www.ahs.ca/guru Background The epidermal growth factor receptor (EGFR) plays a central role in tumour growth and proliferation, and over-expression of EGFR is correlated with a poor prognosis, disease progression, and reduced sensitivity to chemotherapy.1 EGFR-targeted agents are used in several types of cancer, including lung, colorectal, breast, pancreatic, and head and neck. Classes of EGFR inhibitors include monoclonal antibodies (e.g. cetuximab, panitumumab, pertuzumab) and small molecular weight tyrosine kinase inhibitors (e.g. erlotinib, gefitinib, lapatinib, afatinib, osimertinib). These agents have been evaluated in phase II and III trials and are increasingly being incorporated into therapeutic plans for patients, both as front-line therapy, and after progression on standard chemotherapy. EGFR inhibitors are generally well tolerated and are not associated with the moderate or severe systemic side effects of standard cancer therapies such as chemotherapy or radiation. However, because of the role of EGFR in skin biology they are associated with a variety of dermatologic reactions.2 The most commonly reported side effect is acneiform (papulopustular) rash; Table 1 lists the incidence rate for each EFGR inhibitor. Acneiform rash is typically localized to the face, scalp, upper chest and back. Although it is usually mild or moderate in severity, it can cause significant physical and psychosocial distress in patients, which may lead to decreased quality of life, and disruption or discontinuation of therapy.3, 4 Thus, timely and appropriate interventions are essential.5 Table 1. -

Exanthems and Drug Reactions
Dermatology Exanthems and Morton Rawlin drug reactions ‘Well, Mr Jones, I think we should put you on this tablet to Background fix this problem. Now, the things you need to look out for Drug reactions are a common cause of rashes and can vary are any rashes…’ from brief, mildly annoying, self limiting rashes to severe conditions involving multiple organ systems. How often in general practice do you hear yourself Objective offering this advice? Why do almost all drugs list rash as This article outlines an approach to exanthems that a side effect? How do they occur and what can you do to may be related to drug reactions and details appropriate recognise and manage them? management. The skin is the largest organ of the body and, from a diagnostic Discussion viewpoint, we can see it change to various stimuli. Medications Rashes related to drug reactions are both nonallergic and allergic. Nonallergic rashes are usually predictable and are commonly used and are integral to the general practitioner’s may be avoidable. Allergic rashes include morbilliform armamentarium for treating most ills. However, it is also important erythema, urticaria and angioedema, erythema multiforme to note that increasing access to medications by consumers through and vasculitic rashes. The vast majority of cases are other health professionals (eg. naturopaths) and the self prescribed rapidly resolving and self limiting once the offending use of over-the-counter, complementary and alternative medicines agent is removed. Early recognition and supportive should be remembered in the history taking of a patient presenting measures are the keys to care in the majority of cases. -

Petechial Rash May Mask Bacterial Infection
22 PEDIATRIC DERMATOLOGY SEPTEMBER 2009 • SKIN & ALLERGY NEWS Petechial Rash May Mask Bacterial Infection BY BRUCE JANCIN diatric infectious diseases sponsored by north of the nipple line are a somewhat of petechiae wasn’t predictive of serious the Children’s Hospital, Denver. reassuring but less than conclusive indi- disease, said Dr. Dominguez of the Uni- VAIL, COLO. — When is it time to He worries more about one of these cator that the child doesn’t have invasive versity of Colorado, Denver. worry about a child or adolescent with possibilities if the patient appears ill on bacterial disease. In his review of four Once the findings of these four stud- a petechial rash? physical examination; has generalized large published studies of children pre- ies are combined, roughly 10% of chil- Three potentially lethal yet treatable petechiae, purpura, prolonged capillary senting to emergency departments with dren with a petechial rash who present to bacterial infections often produce a pe- refill; and/or an abnormal CBC, C-reac- a petechial rash, two studies totaling 408 the emergency department have under- techial rash: Staphylococcus aureus sepsis, tive protein, or other laboratory tests. He patients concluded that no one with pe- lying meningococcal disease, he added. meningococcal disease, and Rocky worries less if the youth looks well and techiae located only above the nipple line Dr. Dominguez said that any serious- Mountain spotted fever, Dr. Samuel R. has normal lab values. had invasive bacterial disease. In the oth- ly ill youth with a petechial rash ought Dominguez noted at a conference on pe- Petechiae confined to a distribution er two studies, however, the distribution to be treated empirically with ceftriaxone to address a possible Neisseria meningitidis infection, vancomycin to cover methi- cillin-resistant or methicillin-sensitive S. -
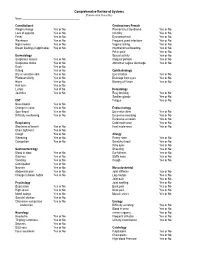
Comprehensive Review of Systems (Please Circle Yes Or No) Name: ______
Comprehensive Review of Systems (Please circle Yes or No) Name: __________________________________________ Constitutional Genitourinary Female Weight change Yes or No Premenstrual Syndrome Yes or No Loss of appetite Yes or No Infertility Yes or No Fever Yes or No Dysmenorrheal Yes or No Weakness Yes or No Frequent yeast infections Yes or No Night sweats Yes or No Vaginal itching Yes or No Breast feeding (if applicable) Yes or No Intermenstrual bleeding Yes or No Pelvic pain Yes or No Dermatology Sexual activity Yes or No Suspicious lesions Yes or No Irregular periods Yes or No Suspicious moles Yes or No Abnormal vaginal discharge Yes or No Rash Yes or No Itching Yes or No Ophthalmology Dry or sensitive skin Yes or No Eye irritation Yes or No Photosensitivity Yes or No Drainage from eyes Yes or No Hives Yes or No Blurring of Vision Yes or No Hair loss Yes or No Lumps Yes of No Hematology Jaundice Yes or No Easy bruising Yes or No Swollen glands Yes or No ENT Fatigue Yes or No Nose bleeds Yes or No Change in voice Yes or No Endocrinology Sore throat Yes or No Excessive thirst Yes or No Difficulty swallowing Yes or No Excessive sweating Yes or No Excessive urination Yes or No Respiratory Cold intolerance Yes or No Shortness of breath Yes or No Heat intolerance Yes or No Chest tightness Yes or No Cough Yes or No Allergy Wheezing Yes or No Runny nose Yes or No Congestion Yes or No Scratchy throat Yes or No Itchy eyes Yes or No Gastroenterology Sneezing Yes or No Blood in stool Yes or No Ear fullness Yes or No Diarrhea Yes or No Stuffy nose -

Scabies Fact Sheet
Scabies Fact Sheet What is scabies? Human scabies is caused by a mite that burrows under the skin. Scabies can spread from one person to another by direct contact (touching). Who gets scabies? Scabies is a common disease that may affect people of all races and social classes. What should I look for? The earliest and most common symptoms of scabies are itching and skin rash especially at night time. This itchy rash looks like a pimple or thin, irregular burrow tracks made up of tiny blisters or bumps on your skin. Scabies may affect either your whole body or only localized warm areas of your skin, such as between your fingers, your wrist, elbow armpit, penis, nipple, waist, or buttocks. How can scabies be transmitted? Scabies can be transmitted by direct and prolonged skin-to-skin contact with an person who has scabies. Scabies can also be transmitted by sharing bedding or clothing. The disease spreads easily to household members, roommates, and sexual partners of a person with scabies. Scabies can spread more easily in crowded settings like hospitals, child-care facilities, nursing homes, homeless shelters, and jails/prisons. What are the complications of scabies? The severe itching of scabies causes people to scratch, which may cause breaks in the skin that allow bacteria to enter and cause skin infection. What should I do if I have itching and/or rash or I think I have been exposed? You should consult with a doctor or go to the nearest emergency room or urgent care if: 1- You have a skin rash and are itching. -

Review of Systems
Warren E. Hill, MD, FACS Neal A. Nirenberg, MD, FACS East Valley Ophthalmology, Ltd. Diplomate, American Board of Ophthalmology Diplomate, American Board of Ophthalmology 5620 E. Broadway Road Diplomate, American Board of Eye Surgery Cataract and Comprehensive Ophthalmology Mesa, Arizona 85206-1438 Cataract and Anterior Segment Surgery Telephone: (480) 981-6111 Facsimile: (480) 985-2426 Jonathan B. Kao, MD Yuri F. McKee, MD Internet www.doctor-hill.com Diplomate, American Board of Ophthalmology Diplomate, American Board of Ophthalmology Cataract, Cornea and External Disease Cataract, Cornea and Anterior Segment Surgery Glaucoma Surgery and Management Review of Systems For new patients, established patients who may be having new problems, or patients we have not seen in a while, we need to update your overall medical health. In each area, if you are not having any difficulties please circle No problems. If you are experiencing any of the symptoms listed, please circle the ones that apply, or you may write in ones that may not be listed. If you have any questions, please ask one of our staff. Cardiovascular Ears/Nose/Throat Musculoskeletal Respiratory Chest pain Dizziness Back pain Cough Irregular heartbeat Hearing loss Joint pain Trouble breathing Shortness of breath Hoarseness Muscle aches Wheezing ________________ Ringing in ears Stiffness ________________ Sore throat Swelling ________________ ________________ No problems No problems No problems No problems Constitutional Hematologic Neurologic Skin Fatigue Bleeding Balance problems