Convalescent Plasma for the Prevention and Treatment of COVID-19: a Systematic Review and Quantitative Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Green Volunteers in the Spotlight
Wessel Ganzevoort Wessel Ganzevoort Green volunteers in the spotlight Green volunteers Green volunteers in the spotlight Understanding action for nature through studying citizen scientists and other nature volunteers WESSEL GANZEVOORT COVER PLANO DEF.indd 1 01-02-2021 13:30 Green Volunteers in the Spotlight Understanding action for nature through studying citizen scientists and other nature volunteers Wessel Ganzevoort Green Volunteers in the Spotlight Green Volunteers in the Spotlight Understanding action for nature through studying citizen scientists and other nature volunteers Proefschrift Colofon Author: Wessel Ganzevoort ter verkrijging van de graad van doctor Cover: The Oak King by Emily Balivet aan de Radboud Universiteit Nijmegen Lay-out: Luc Dinnissen, studio ds op gezag van de rector magnificus prof. dr. J.H.J.M. van Krieken, Printed by: DPN Rikken (Nijmegen) volgens besluit van het college van decanen ISBN: 978-94-640-2724-2 in het openbaar te verdedigen op Ganzevoort, W. (2021). Green volunteers in the spotlight: Understanding action for dinsdag 16 maart 2021 nature through studying citizen scientists and other nature volunteers. Doctoral disser- om 16.30 uur precies tation, Radboud University. door © W.B. Ganzevoort, 2021 All rights reserved. No part of this publication may be reproduced or transmitted in Wessel Bote Ganzevoort any form by any means without permission from the author. geboren op 18 oktober 1991 We have done our utmost to contact Emily Balivet, the copyright holder of the art- te Utrecht work on the cover. If this book comes to her attention, we ask her to contact us at [email protected]. 3 Green Volunteers in the Spotlight “I almost altered my title to ‘The love and study of the living bird in nature’, but reflected than in the eyes of a number of ornitholo- gists, the use of the word ‘love’ would be unscientific. -

Participant List
Participant List 10/20/2019 8:45:44 AM Category First Name Last Name Position Organization Nationality CSO Jillian Abballe UN Advocacy Officer and Anglican Communion United States Head of Office Ramil Abbasov Chariman of the Managing Spektr Socio-Economic Azerbaijan Board Researches and Development Public Union Babak Abbaszadeh President and Chief Toronto Centre for Global Canada Executive Officer Leadership in Financial Supervision Amr Abdallah Director, Gulf Programs Educaiton for Employment - United States EFE HAGAR ABDELRAHM African affairs & SDGs Unit Maat for Peace, Development Egypt AN Manager and Human Rights Abukar Abdi CEO Juba Foundation Kenya Nabil Abdo MENA Senior Policy Oxfam International Lebanon Advisor Mala Abdulaziz Executive director Swift Relief Foundation Nigeria Maryati Abdullah Director/National Publish What You Pay Indonesia Coordinator Indonesia Yussuf Abdullahi Regional Team Lead Pact Kenya Abdulahi Abdulraheem Executive Director Initiative for Sound Education Nigeria Relationship & Health Muttaqa Abdulra'uf Research Fellow International Trade Union Nigeria Confederation (ITUC) Kehinde Abdulsalam Interfaith Minister Strength in Diversity Nigeria Development Centre, Nigeria Kassim Abdulsalam Zonal Coordinator/Field Strength in Diversity Nigeria Executive Development Centre, Nigeria and Farmers Advocacy and Support Initiative in Nig Shahlo Abdunabizoda Director Jahon Tajikistan Shontaye Abegaz Executive Director International Insitute for Human United States Security Subhashini Abeysinghe Research Director Verite -

HLPE Report # 12
HLPE REPORT 12 Nutrition and food systems A report by The High Level Panel of Experts on Food Security and Nutrition September 2017 HLPE High Level Panel of Experts HLPE Reports series #1 Price volatility and food security (2011) #2 Land tenure and international investments in agriculture (2011) #3 Food security and climate change (2012) #4 Social protection for food security (2012) #5 Biofuels and food security (2013) #6 Investing in smallholder agriculture for food security (2013) #7 Sustainable fisheries and aquaculture for food security and nutrition (2014) #8 Food losses and waste in the context of sustainable food systems (2014) #9 Water for food security and nutrition (2015) #10 Sustainable agricultural development for food security and nutrition: what roles for livestock? (2016) #11 Sustainable forestry for food security and nutrition (2017) #12 Nutrition and food systems (2017) All HLPE reports are available at www.fao.org/cfs/cfs-hlpe 2 HLPE Steering Committee members (September 2017) Patrick Caron (Chair) Carol Kalafatic (Vice-Chair) Amadou Allahoury Louise Fresco Eileen Kennedy Muhammad Azeem Khan Bernardo Kliksberg Fangquan Mei Sophia Murphy Mohammad Saeid Noori Naeini Michel Pimbert Juan Ángel Rivera Dommarco Magdalena Sepúlveda Martin Yemefack Rami Zurayk HLPE Project Team members Jessica Fanzo (Team Leader) Mandana Arabi Barbara Burlingame Lawrence Haddad Simon Kimenju Gregory Miller Fengying Nie Elisabetta Recine Lluís Serra-Majem Dipa Sinha Coordinator of the HLPE Nathanaël Pingault This report by the High Level Panel of Experts on Food Security and Nutrition (HLPE) has been approved by the HLPE Steering Committee. The views expressed do not necessarily reflect the official views of the Committee on World Food Security, of its members, participants, or of the Secretariat. -

Tamil Amma Magan Kama Kathaigalpeperonity
Tamil Amma Magan Kama Kathaigal.peperonity Tamil Amma Magan Kama Kathaigal.peperonity 1 / 3 2 / 3 Amma magan okkum kathai peperonity. then the point is just to tell what did the mother did to her son. TamilKamakathaikal Tamil Kamakathaikal Tamil Kama.. Maganai okkum tamil akka thambi Great first amma kama kathai tamil kama kathaigal cerita Here the evergreen website peperonity. 2014 marumagan.. Tamill Font Pdf Family Anni Amma Akka AuntyThambi Magan Appa Free Peperonity Blogspot. Tamil Kama Kathai Amma pundai kathaigal, amma magan olu.. 5 mars 2018 . Tamil Amma Magan Kama Kathaigal.peperonity > DOWNLOAD (Mirror #1). Spoiler. Tamil Kama sutra Tamil sex stories. RSS. Sample Page.. siteku(peperonity) vanthu ammavaium okkalanu therinthukonde. neraiya per . DOC-Live: amma magan kama kathaigal - Online Free Unlimited pdf . Amma Magan Kama Kadhai In Tamil Language 6. ammavai tadaviya thatha Busil Enudan.. amma magan udan seiyum kamaleelai gal tamil kamakathaikal if you want to read amma . uravu kalla uravu kathaigal kama kathaikalamma magan kaamakathai . stories amm vdeo amma akka thangai pdf amma kathaikal peperonity amma.. Mar 5, 2018 . Tamil Amma Magan Kama Kathaigal.peperonity >> DOWNLOAD.. One of them (my Lord tamil amma magan kama kathaigal peperonity zip is your friend; but me thinks my lady weeps; I like not that. So he gave command that the.. Photos Tamil Pengal Aunty Soothu Padangal. com. kaai kai adi. peperonity, tamil . magan amma kamakathaigal: juz amma arabic: amma magan kama kathaiy: . tamil. akka,akkavin adi pavadai,periya mulai, kama tamil kathai. peperonity ,.. Feb 5, 2018 . Amma Magan Kama Kathai Download PDF Velangatha unmai sollavantha kathai amma . Amma Magan Kamakathaikal In Tamil Tamilkamakathaikal Tamil . -

China's Space and Counterspace Capabilities and Activities
China’s Space and Counterspace Capabilities and Activities Prepared for: The U.S.-China Economic and Security Review Commission Prepared By: Mark Stokes, Gabriel Alvarado, Emily Weinstein, and Ian Easton March 30, 2020 Disclaimer: This research report was prepared at the request of the U.S.-China Economic and Security Review Commission to support its deliberations. Posting of the report to the Commission's website is intended to promote greater public understanding of the issues addressed by the Commission in its ongoing assessment of U.S.-China economic relations and their implications for U.S. security, as mandated by Public Law 106-398 and Public Law 113-291. However, it does not necessarily imply an endorsement by the Commission or any individual Commissioner of the views or conclusions expressed in this commissioned research report. Table of Contents KEY FINDINGS ............................................................................................................................ 3 RECOMMENDATIONS ............................................................................................................... 4 INTRODUCTION .......................................................................................................................... 5 SECTION ONE: Drivers for Current and Future PLA Space/Counterspace Capabilities ........ 8 Space-Related Policy Statements ........................................................................................................... 9 Strategic Drivers and Doctrine ........................................................................................................... -

Plant to Build Office Buildings, Warehouse Here to Cost $750,000
Complete Newi, Picture* A Newspaper Devoted Presented Fairly, Clearly To the Community Interest Impartially Each Week Full Local Coverage *X.'.. vol. XLVII-NO. 13. Entered ts atcond Olui Utttn 4;!' »t tht Poat'Offli*, WoodMdg*, If, J. WOODBRIDOE, N. J., THURSDAY, MAY 19, 1955 PRICE EIGHT CENTS Governor Attends Reception Here for New California Oil Head Plant to Build Office Buildings, Warehouse Here to Cost $750,000 •2*1 Jennings, Adams Appointed Metal-Thermit To New Air Force Academy Headquarters WOODBRIDGE—A WoodbrldRe High School student and a former resident of Woodbridge were among the Ml cadets out of 8,000 can- To be Shifted didates chosen for th« first class of the new Air Foroe Academy, ac- cording to an announcement made by Secretary Harold K. Talbott. WOODBRIDOE Announce- The local student la Robert Sidney Franklin J*nnlnga, son of Mr. ment was made yesterday by •nnd Mrs. Wlllard K. Jennings, 5 Falrvlew Avenue, Colonia. The former Metal 4t Thermit Corporation it resident is James Riven Adams, will erect a $750,000 Reneral of- son of Mr. ahd Mrs. Clement H. Watson, Oarfleld Road, Concord, Win Coveted Places fice building and warehouse here Mass., and the grandson of Mr. adjacent to lta Research Labora- and Mrs. Janwa J./Dunne, Oreen tory on Rahway Avenue. It Is ex- Street. Rivers, who will graduate pected the building will be ready from Concord High School,1 June for occupancy in April, 1956. 8. has been an honor student. Hl| The office building will consist TI-I)Iinn was held yesterday pany and was attended by Gov- left to right, vt Charles E. -
Free Movie Aaj Ka Samson
Free Movie Aaj Ka Samson 1 / 4 2 / 4 Free Movie Aaj Ka Samson 3 / 4 See the full list of Aaj Ka Samson cast and crew including actors, directors, producers and ... Two children, Samson and Reshma, want to spend their lives together when they grow up. ... see full movie info ... Win FREE MoviePass for a Year!. 4 Jul 2016 - 135 min - Uploaded by Old Classic MoviesAaj Ka Samson | Full Hindi Movie | Hemant Birje, Sahila Chaddha, Goga Kapoor, Gulshan .... We don't offer download of the Movie AAJ KA SAMSON, nor we send free poster of the Movie along with its VCD order. We also don't offer free wallpaper or .... Watch Aaj Ka Samson 1991 Full Hindi Movie Free Online Director: Kukoo Kapoor Starring: Hemant Birje, Sahila Chaddha, Goga Kapoor, Puneet Issar Genre: .... 10 May 2018 ... AAJ KA SAMSON || FULL HINDI MOVIE || HEMANT BIRJE, SAHILA CHADDHA, GOGA KAPOOR || EVERGREEN CINEMA. by News Facto .... Buy Aaj Ka Samson: Read Movies & TV Reviews - Amazon.com. ... Start your 7-day free trial. The romantic drama about two children who want to spend their .... 4 Nov 2016 - 124 min - Uploaded by Bollywood CinemasWatch Aaj Ka Samson (1991) Full Length Hindi Movie - Hemant Birje, Sahila Chadha, Goga .... Buy Aaj Ka Samson: Read Movies & TV Reviews - Amazon.com. ... Watch with Eros Now Start your 7-day free trial. Add to. Watchlist. By placing your order or .... 17 Nov 2016 ... Aaj Ka Samson (1991) – Hindi Movie Watch Online. ... Full Movie Putlocker Aaj Ka Samson online free streaming Aaj Ka Samson Watch Online .... Aaj Ka Samson (1991) .. -
The Orthodox Patristic Teaching on the Human Embryo and the Ethical Repercussions on Abortion and Related Issues
Durham E-Theses The orthodox patristic teaching on the human embryo and the ethical repercussions on abortion and related issues Televantos, FR Anastasios How to cite: Televantos, FR Anastasios (1998) The orthodox patristic teaching on the human embryo and the ethical repercussions on abortion and related issues, Durham theses, Durham University. Available at Durham E-Theses Online: http://etheses.dur.ac.uk/4865/ Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in Durham E-Theses • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. Please consult the full Durham E-Theses policy for further details. Academic Support Oce, Durham University, University Oce, Old Elvet, Durham DH1 3HP e-mail: [email protected] Tel: +44 0191 334 6107 http://etheses.dur.ac.uk 2 THE ORTHODOX PATRISTIC TEACHING ON THE HUMAN EMBRYO AND THE ETHICAL REPERCUSSIONS ON ABORTION AND RELATED ISSUES Tlie copyright of tliis thesis rests with the author. No quotation from it should be published witliout tlie written consent of die audior and information derived from it should be acknowledged. FR ANASTASIOS TELEVANTOS submitting for the MA(Theology) qualification UNIVERSITY OF DURHAM DEPARTMENT OF THEOLOGY 1998 1 1 MAY 1999 ACKNOWLEDGEMENTS I wish to express my gratitude to Dr A. -
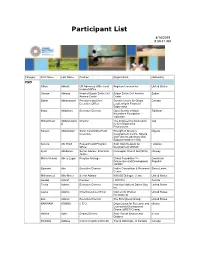
Participant List
Participant List 4/14/2019 8:59:41 AM Category First Name Last Name Position Organization Nationality CSO Jillian Abballe UN Advocacy Officer and Anglican Communion United States Head of Office Osman Abbass Head of Sudan Sickle Cell Sudan Sickle Cell Anemia Sudan Anemia Center Center Babak Abbaszadeh President and Chief Toronto Centre for Global Canada Executive Officer Leadership in Financial Supervision Ilhom Abdulloev Executive Director Open Society Institute Tajikistan Assistance Foundation - Tajikistan Mohammed Abdulmawjoo Director The Engineering Association Iraq d for Development & Environment Kassim Abdulsalam Zonal Coordinator/Field Strength in Diversity Nigeria Executive Development Centre, Nigeria and Farmers Advocacy and Support Initiative in Nig Serena Abi Khalil Research and Program Arab NGO Network for Lebanon Officer Development (ANND) Kjetil Abildsnes Senior Adviser, Economic Norwegian Church Aid (NCA) Norway Justice Maria Victoria Abreu Lugar Program Manager Global Foundation for Dominican Democracy and Development Republic (GFDD) Edmond Abu Executive Director Native Consortium & Research Sierra Leone Center Mohammed Abu-Nimer Senior Advisor KAICIID Dialogue Centre United States Aouadi Achraf Founder I WATCH Tunisia Terica Adams Executive Director Hamilton National Dance Day United States Inc. Laurel Adams Chief Executive Officer Women for Women United States International Zoë Adams Executive Director The Strongheart Group United States BAKINAM ADAMU C E O Organization for Research and Ghana Community Development Ghana -

Baby Boy Names Registered in 2010
Page 1 of 39 Baby Boy Names Registered in 2010 # Baby Boy Names # Baby Boy Names # Baby Boy Names 1 A. 1 Abdulahi 1 Adas-Wandycz 1 A.G. 1 Abdul-Azeez 1 Addison 1 A.J 1 Abdulhay 1 Addox 1 A.J. 1 Abdul-Kareem 1 Ade 1 Aaden 1 Abdulla 2 Adé 1 Aadhi 13 Abdullah 1 Adekola 2 Aadi 6 Abdullahi 2 Adem 1 Aaen 1 Abdul-Majid 1 Ademíl 1 Aagam 1 Abdulmuhaimin 13 Aden 2 Aahil 1 Abdul-Rafay 1 Adeoluwa 1 Aaidan 1 Abdulraheem 1 Adewale 1 Aamir 2 Abdulrahman 3 Adham 1 Aarab 1 Abdul-Rahman 1 Adhwaidh 1 Aaran 1 Abdur 1 Adib 14 Aarav 1 Abdurahman 2 Adil 1 Aaravjeet 1 Abdu-Rahman 1 Adino 3 Aaric 1 Abdurrahman 1 Adison 1 Aarion 2 Abe 5 Aditya 1 Aaris 1 Abeer 1 Adler 1 Aarish 7 Abel 1 Adley 4 Aariz 1 Abhay 1 Adnaan 2 Aarnav 1 Abhaykaran 2 Adnan 69 Aaron 1 Abhijit 1 Adolf 2 Aarush 4 Abhijot 1 Adonai 1 Aarya 3 Abhiraj 1 Adoniah 4 Aaryan 2 Abiel 1 Adrean 1 Aashim 1 Abinaik 31 Adrian 1 Aathmaj 1 Abnet 3 Adriano 1 Aave 1 Abo 4 Adriel 2 Aayaan 1 Abokor 4 Adrien 2 Aayan 1 Abolfazl 2 Adrik 1 Aazan 1 Aboubacar 2 Advaith 1 Abad 4 Abraham 1 Advay 8 Abbas 8 Abram 1 Advaya 1 Abbott 1 Absera 1 Adwin 1 Abdallah 1 Absham 1 Adyson 1 Abdar 1 Abubaker 1 Aedan 1 Abdelaziz 1 Abubkr 1 Aeden 4 Abdi 1 Acaden 1 Aelam 1 Abdias 3 Ace 1 Aellilan 1 Abdiaziz 1 Acer 1 Aemen 1 Abdifatah 1 Acesa 1 Aeodyn 1 Abdihakim 1 Aceton 1 Aeric 1 Abdiqani 3 Achilles 1 Aeron 1 Abdiraxman 1 Adain 2 Aeson 1 Abdirihman 123 Adam 1 Afan 1 Abdisamad 1 Adam-Mustapha 1 Afeef 1 Abdosh 1 Adan 1 Afnan 1 Abdruhman 1 Adar 1 Afraz 7 Abdul 2 Adarsh 1 Afsheen Page 2 of 39 Baby Boy Names Registered in 2010 # Baby Boy Names -
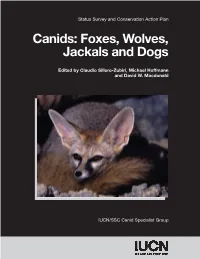
Canids: Status Survey and Conservation Action Plan
IUCN/Species Survival Commission Foxes, Wolves, Jackals and Dogs Canids: Status Survey and Conservation Action Plan The Species Survival Commission (SSC) is one of six volunteer commissions of IUCN – The World Conservation Union, a union of sovereign states, government agencies and non- governmental organisations. IUCN has three basic conservation objectives: to secure the conservation of nature, and especially of biological diversity, as an essential foundation for the future; to ensure that where the Earth’s natural resources are used this is done in a wise, Canids: Foxes, Wolves, equitable and sustainable way; and to guide the development of human communities towards ways of life that are both of good quality and in enduring harmony with other components of the biosphere. Jackals and Dogs A volunteer network comprised of some 8,000 scientists, field researchers, government officials and conservation leaders from nearly every country of the world, the SSC membership is an unmatched source of information about biological diversity and its conservation. As such, SSC Edited by Claudio Sillero-Zubiri, Michael Hoffmann members provide technical and scientific counsel for conservation projects throughout the world and serve as resources to governments, international conventions and conservation and David W. Macdonald organisations. IUCN/SSC Action Plans assess the conservation status of species and their habitats, and specifies conservation priorities. The series is one of the world’s most authoritative sources of Survey and Conservation Action -

2016 General Conference Directory
Celebrating the Bi-Centennial 1816-2016 50TH QUADRENNIAL SESSION OF THE GENERAL CONFERENCE PHILADELPHIA, PENNSYLVANIA July 6 – 13, 2016 Bishop Samuel L. Green, Sr. General Conference Commission Chairperson Bishop McKinley Young Program Committee Chairperson Bishop Gregory G.M. Ingram Host Bishop Bishop John R. Bryant Senior Bishop Bishop John F. White, Sr. OFFICIAL DIRECTORY Council of Bishops President Dr. Richard Allen LeWis, Sr. Treasurer & Chief Financial Officer Dr. Jeffery B. Cooper General Secretary & Chief Information Officer AMEC General Conference 2016 TABLE OF CONTENTS GENERAL CONFERENCE AGENDA............................................................................................................................2 BISHOPS OF THE CHURCH 2012-2016...................................................................................................................13 RETIRED BISHOPS...........................................................................................................................................................16 WOMEN’S MISSIONARY SOCIETY SUPERVISORS 2012-2016......................................................................18 GENERAL OFFICERS 2012-2016...............................................................................................................................23 CONNECTIONAL DEPARTMENT HEADS AND OFFICERS 2012-2016.......................................................26 BOARD OF TRUSTEES 2012-2016............................................................................................................................30