The Generalized Aminoaciduria Seen in Patients with Hepatocyte Nuclear Factor-1 Mutations Is a Feature of All Patients with Diab
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leading Article the Molecular and Genetic Base of Congenital Transport
Gut 2000;46:585–587 585 Gut: first published as 10.1136/gut.46.5.585 on 1 May 2000. Downloaded from Leading article The molecular and genetic base of congenital transport defects In the past 10 years, several monogenetic abnormalities Given the size of SGLT1 mRNA (2.3 kb), the gene is large, have been identified in families with congenital intestinal with 15 exons, and the introns range between 3 and 2.2 kb. transport defects. Wright and colleagues12 described the A single base change was identified in the entire coding first, which concerns congenital glucose and galactose region of one child, a finding that was confirmed in the malabsorption. Subsequently, altered genes were identified other aZicted sister. This was a homozygous guanine to in partial or total loss of nutrient absorption, including adenine base change at position 92. The patient’s parents cystinuria, lysinuric protein intolerance, Menkes’ disease were heterozygotes for this mutation. In addition, it was (copper malabsorption), bile salt malabsorption, certain found that the 92 mutation was associated with inhibition forms of lipid malabsorption, and congenital chloride diar- of sugar transport by the protein. Since the first familial rhoea. Altered genes may also result in decreased secretion study, genomic DNA has been screened in 31 symptomatic (for chloride in cystic fibrosis) or increased absorption (for GGM patients in 27 kindred from diVerent parts of the sodium in Liddle’s syndrome or copper in Wilson’s world. In all 33 cases the mutation produced truncated or disease)—for general review see Scriver and colleagues,3 mutant proteins. -

Novel Insights Into the Pathophysiology of Kidney Disease in Methylmalonic Aciduria
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2017 Novel Insights into the Pathophysiology of Kidney Disease in Methylmalonic Aciduria Schumann, Anke Posted at the Zurich Open Repository and Archive, University of Zurich ZORA URL: https://doi.org/10.5167/uzh-148531 Dissertation Published Version Originally published at: Schumann, Anke. Novel Insights into the Pathophysiology of Kidney Disease in Methylmalonic Aciduria. 2017, University of Zurich, Faculty of Medicine. Novel Insights into the Pathophysiology of Kidney Disease in Methylmalonic Aciduria Dissertation zur Erlangung der naturwissenschaftlichen Doktorwürde (Dr. sc. nat.) vorgelegt der Mathematisch-naturwissenschaftlichen Fakultät der Universität Zürich von Anke Schumann aus Deutschland Promotionskommission Prof. Dr. Olivier Devuyst (Vorsitz und Leitung der Dissertation) Prof. Dr. Matthias R. Baumgartner Prof. Dr. Stefan Kölker Zürich, 2017 DECLARATION I hereby declare that the presented work and results are the product of my own work. Contributions of others or sources used for explanations are acknowledged and cited as such. This work was carried out in Zurich under the supervision of Prof. Dr. O. Devuyst and Prof. Dr. M.R. Baumgartner from August 2012 to August 2016. Peer-reviewed publications presented in this work: Haarmann A, Mayr M, Kölker S, Baumgartner ER, Schnierda J, Hopfer H, Devuyst O, Baumgartner MR. Renal involvement in a patient with cobalamin A type (cblA) methylmalonic aciduria: a 42-year follow-up. Mol Genet Metab. 2013 Dec;110(4):472-6. doi: 10.1016/j.ymgme.2013.08.021. Epub 2013 Sep 17. Schumann A, Luciani A, Berquez M, Tokonami N, Debaix H, Forny P, Kölker S, Diomedi Camassei F, CB, MK, Faresse N, Hall A, Ziegler U, Baumgartner M and Devuyst O. -
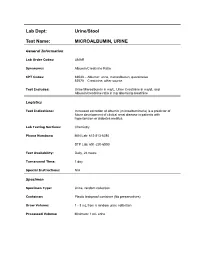
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE General Information Lab Order Codes: UMAR Synonyms: Albumin/Creatinine Ratio CPT Codes: 82043 – Albumin: urine, microalbumin, quantitative 82570 – Creatinine; other source Test Includes: Urine Microalbumin in mg/L, Urine Creatinine in mg/dL and Albumin/creatinine ratio in mg albumin/g creatinine Logistics Test Indications: Increased excretion of albumin (microalbuminuria) is a predictor of future development of clinical renal disease in patients with hypertension or diabetes mellitus. Lab Testing Sections: Chemistry Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 day Special Instructions: N/A Specimen Specimen Type: Urine, random collection Container: Plastic leakproof container (No preservatives) Draw Volume: 1 - 3 mL from a random urine collection Processed Volume: Minimum: 1 mL urine Collection: A random urine sample may be obtained by voiding into a urine cup and is often performed at the laboratory. Bring the refrigerated container to the lab. Make sure all specimens submitted to the laboratory are properly labeled with the patient’s name, medical record number and date of birth. Special Processing: Lab Staff: Centrifuge specimen before analysis. Patient Preparation: Sample should not be collected after exertion, in the presence of a urinary tract infection, during acute illness, immediately after surgery, or after acute fluid load. Sample Rejection: Mislabled or unlabeled specimens; samples contaminated with blood Interpretive Reference Range: Albumin/creatinine ratio (A/C <30 mg/g Normal ratio) 30 - 299 mg/g Microalbuminuria >300 mg/g Clinical albuminuria Urine Creatinine: No reference ranges established Critical Values: N/A Limitations: Due to variability in urinary albumin excretion, at least two of three test results measured within a 6-month period should show elevated levels before a patient is designated as having microalbuminuria. -

Prevalence of Microalbuminuria and Associated Risk Factors Among Adult Korean Hypertensive Patients in a Primary Care Setting
Hypertension Research (2013) 36, 807–823 & 2013 The Japanese Society of Hypertension All rights reserved 0916-9636/13 www.nature.com/hr ORIGINAL ARTICLE Prevalence of microalbuminuria and associated risk factors among adult Korean hypertensive patients in a primary care setting Yon Su Kim 1, Han Soo Kim2, Ha Young Oh3, Moon-Kyu Lee4, Cheol Ho Kim5, Yong Soo Kim6,DavidWu6, Amy O Johnson-Levonas6 and Byung-Hee Oh7 Microalbuminuria is an early sign of nephropathy and an independent predictor of end-stage renal disease. The purpose of this study was to assess microalbuminuria prevalence and its contributing factors in Korean hypertensive patients. This cross-sectional study enrolled male and female patients of X35 years old with an essential hypertension diagnosis as made by 841 physicians in primary care clinics and 17 in general hospitals in the Republic of Korea between November 2008 and July 2009. To assess microalbuminuria prevalence, urine albumin/creatinine ratio (UACR) was measured in patients with a positive dipstick test. Of the 40 473 enrolled patients, 5713 (14.1%) had a positive dipstick test. Of 5393 patients with a positive dipstick test and valid UACR values, 2657 (6.6%) had significantly elevated UACR (X30 lgmgÀ1), 2158 (5.4%) had microalbuminuria (30 lgmgÀ1pUACR o300 lgmgÀ1) and 499 (1.2%) had macroalbuminuria (UACR X300 lgmgÀ1). Based on multivariate analysis, independent factors associated with elevated UACR included low adherence to antihypertensive medication (23% higher; P ¼ 0.042), poorly controlled blood pressure (BP; 38% higher for systolic BP/diastolic BP X130 mm Hg/X80 mm Hg; Po0.001), obesity (47% higher for body mass index (BMI) X25.0 kg m À2; Po0.001), age (17% lower and 58% higher for age categories 35–44 years (P ¼ 0.043) and 475 years (Po0.001), respectively) and a prior history of diabetes (151% higher; Po0.001) and kidney-related disease (71% higher; Po0.001). -

Transient Acquired Fanconi Syndrome with Unusual and Rare Aetiologies: a Case Study of Two Dogs
Veterinarni Medicina, 65, 2020 (01): 41–47 Case Report https://doi.org/10.17221/103/2019-VETMED Transient acquired Fanconi syndrome with unusual and rare aetiologies: A case study of two dogs Ju-Yong Park1, Ji-Hwan Park1, Hyun-Jung Han2, Jung-Hyun Kim3* 1Department of Veterinary Internal Medicine, Veterinary Medical Teaching Hospital, Konkuk University, Seoul, Republic of Korea 2Department of Veterinary Emergency, College of Veterinary Medicine, Konkuk University, Seoul, Republic of Korea 3Department of Veterinary Internal Medicine, College of Veterinary Medicine, Konkuk University, Seoul, Republic of Korea *Corresponding author: [email protected] Ju-Yong Park and Ji-Hwan Park contributed equally to this work Citation: Park JY, Park JH, Han HJ, Kim JH (2020): Transient acquired Fanconi syndrome with unusual and rare aetiolo- gies: A case study of two dogs. Vet Med-Czech 65, 41–47. Abstract: The acquired form of Fanconi syndrome is seldom identified in dogs; those cases that have been reported have been secondary to hepatic copper toxicosis, primary hypoparathyroidism, ingestion of chicken jerky treats, exposure to ethylene glycol, or gentamicin toxicity. However, to the best of our knowledge, there have been no reports of acquired Fanconi syndrome secondary to Babesia infection or ingestion of cosmetics in dogs. We here report on two dogs presented with a history of marked polyuria, polydipsia, and lethargy. Laboratory examina- tions showed glucosuria with normoglycaemia and severe urinary loss of amino acids. One dog was infected with Babesia gibsoni and the other dog had a history of cosmetics ingestion. The first dog received treatment for Babesia infection and the second dog received aggressive care to correct metabolic acidosis, electrolyte imbalances, and other add-on deficiencies. -

Original Article Prevalence of Aminoacidurias in a Tertiary Care Pediatric Medical College Hospital J
DOI: 10.14260/jemds/2015/650 ORIGINAL ARTICLE PREVALENCE OF AMINOACIDURIAS IN A TERTIARY CARE PEDIATRIC MEDICAL COLLEGE HOSPITAL J. N. George1, A. Amaresh2, N. J. Gokula Kumari3 HOW TO CITE THIS ARTICLE: J. N. George, A. Amaresh, N. J. Gokula Kumari. “Prevalence of Aminoacidurias in a Tertiary Care Pediatric Medical College Hospital”. Journal of Evolution of Medical and Dental Sciences 2015; Vol. 4, Issue 26, March 30; Page: 4500-4508, DOI: 10.14260/jemds/2015/650 ABSTRACT: BACKGROUND: Inborn errors of metabolism (IEM) comprises of a diverse group of heterogeneous disorders manifesting in paediatric population. Cases of Inborn errors of metabolism, individually are rare but collectively are common. The timing of presentation depends on significant accumulation of toxic metabolites or on the deficiency of substrate. These disorders manifest by subtle neurologic or psychiatric features often go undiagnosed until adulthood. OBJECTIVES: The objectives of the present study was to carry out preliminary screening on urine samples from pediatric population with either metabolic or neurological manifestations for inborn errors of metabolism and to know the prevalence of aminoaciduria in tertiary care setup for early diagnosis and detection. METHODS: The present study is a cross sectional time bound study carried out at Niloufer Institute of Child Health, Osmania Medical College, Hyderabad, from August 2013 to July 2014. A total of 119 samples were analyzed from suspected cases of IEM. Samples were analyzed for all physical and chemical parameters and positive cases reported by these investigations were referred for confirmation by TMS, HPLC, and GCMS. RESULTS: Among 119 children analyzed, 29 were given presumptive diagnosis of IEM based on screening tests, urinary aminoacidogram by TLC and clinical correlation. -

Pathological Findings in Homocystinuria
J Clin Pathol: first published as 10.1136/jcp.17.4.427 on 1 July 1964. Downloaded from J. clin. Path. (1964), 17, 427 Pathological findings in homocystinuria J. B. GIBSON', NINA A. J. CARSON, AND D. W. NEILL2 From the Departments ofPathology and of Child Health, and the Biochemistry Laboratory, The Queen's University of Belfast, and Royal Belfast Hospitalfor Sick Children, and Royal Victoria Hospital, Belfast SYNOPSIS Pathological findings are described in four cases of a new aminoaciduria in which homocystine is excreted in the urine. All the patients were mentally retarded children. Three of them presented diagnostic features of Marfan's syndrome. Necropsy on one case and biopsy findings in the others are described. Fatty change occurs in the liver. The most striking lesions are vascular. Metachromatic medial degeneration of the aorta and of the elastic arteries in the necropsied case are considered in relation to Marfan's syndrome. Other changes, particularly thrombosis which is prevalent in homocystinuria, suggest the possibility of a platelet defect. The findings are discussed in respect of an upset in the metabolism of sulphur-containing amino-acids and with particular reference to Marfan's syndrome. A systematic search for metabolic abnormalities in Their appearance was that of Marfan's syndrome mentally retarded individuals in Northern Ireland and in fact two of them had been designated pre- revealed a hitherto unrecognized specific amino- viously as classical examples of Marfan's syndrome aciduria, in which the sulphur-containing amino- in published studies of that condition (case A4, acid homocystine is excreted (Carson and Neill, Lynas, 1958; case 4, Loughridge, 1959). -

A New Inborn Error of Metabolism Associated with Mental Deficiency
Arch Dis Child: first published as 10.1136/adc.38.201.425 on 1 October 1963. Downloaded from Arch. Dis. Childl., 1963, 38, 425. HOMOCYSTINURIA: A NEW INBORN ERROR OF METABOLISM ASSOCIATED WITH MENTAL DEFICIENCY BY NINA A. J. CARSON*, D. C. CUSWORTHt, C. E. DENTt, C. M. B. FIELD+, D. W. NEILL§ and R. G. WESTALLt From Royal Belfast Hospital for Sick Children, University College Hospital Medical School, London, Belfast City Hospital, and Royal Victoria Hospital, Belfast (RECEIVED FOR PUBLICATION MARCH 20, 1963) It is now becoming generally noted that many imagine that sooner or later similar metabolic diseases of hitherto unknown aetiology are due to disorders will be discovered that will involve the inborn errors of metabolism in the sense in which remaining amino acids. Garrod (1923) used this term. Although these The present study concerns a further presumed diseases cover the whole of medicine it has been inborn error of amino acid metabolism, this time particularly gratifying to note that mental disease, involving the sulphur-containing compound homo- especially mental deficiency which currently is cystine. The discovery arose from the submission responsible for one of our main medical problems, by one of us (C.M.B.F.) of urine from two mentally has been especially involved in these recent dis- retarded sibs whose clinical features were thought coveries. In particular, a number of inborn errors to suggest a possible metabolic basis. The urine of metabolism causing mental disease have been was sent for examination to others of us (N.A.J.C. described recently in which the disorder concerned and D.W.N.) who were currently running a meta- copyright. -

Amino Acids (Urine)
Amino Acids (Urine) A profile of amino acids is provided: alanine, -amino butyric acid, arginine, asparagine, aspartic acid, carnosine, citrulline, cystine, glutamic acid, glutamine, glycine, histidine, homocystine, hydroxylysine, isoleucine, leucine, Description lysine, methionine, 1-methyl histidine, 3-methyl histidine, ornithine, phenylalanine, phosphoethanolamine, proline, sarcosine, serine, taurine, threonine, tyrosine, tryptophan, valine. In general, urine is useful when investigating a disorder of renal transport particularly with a positive urine nitroprusside test eg for cystinuria and homocystinuria, nephrolithiasis and or the Fanconi syndrome. Other Indication reasons maybe selective metabolic screening, hyperammonaemia, suspected aminoacidopathy, suspected disorder of energy metabolism, epileptic encephalopathy, control of protein restricted diet. Functions of amino acids include the basic structural units of proteins, metabolic intermediates and neurotransmission. Over 95% of the amino acid load filtered from the blood at the renal glomerulus is normally reabsorbed in the proximal Additional Info renal tubules by saturable transport systems. The term ‘aminoaciduria’ is used when more than 5% of the filtered load is detected in the urine. In normal individuals, aminoaciduria is transient and is associated with protein intake in excess of amino acid requirements. Concurrent Tests Plasma amino acids Dietary Requirements N/A Values depend on metabolic state. Cystinuria: Increased urinary cystine, lysine, arginine and ornithine. Interpretation Homocystinuria: Increased urinary homocysteine and methionine. Fanconi syndrome: Generalised increase in urinary amino acid excretion. Collection Conditions No restrictions. Repeat measurement inappropriate except in acute Frequency of testing presentation of undiagnosed suspected metabolic disorder. Version 1 Date: 25/01/11 Document agreed by: Dr NB Roberts . -

Disease Name Tyrosinemia Type III
Disease Name Tyrosinemia type III Alternate name(s) Hereditary infantile tyrosinemia, Hepatorenal tyrosinemia, Fumarylacetoacetase deficiency, Fumarylacetoacetate hydrolase FAH deficiency Acronym TYR-3 Disease Classification Amino Acid Disorder Variants Yes Variant name Tyrosinemia I chronic-type, Tyrosinemia II, Tyrosinemia III Symptom onset Infancy Symptoms Hepatocellular degeneration leading to acute hepatic failure or chronic cirrhosis and hepatocellular carcinoma, renal Fanconi syndrome, peripheral neuropathy, seizures and possible cardiomyopathy. Natural history without treatment Chronic liver disease leading to cirrhosis and hepatocellular carcinoma. Renal tubular disease (Fanconi syndrome) with phosphaturia, aminoaciduria and often glycosuria. May lead to clinical rickets. Peripheral neuropathy. Self- injurious behavior, seizures and cardiomyopathy have been observed. Coagulation problems. Natural history with treatment Hepatitic disease may progress despite dietary treatment. NTBC treatment leads to improvements in kidney, liver and neurologic function, but may not affect incidence of liver cancer. Treatment Dietary restriction of phenylalanine and tyrosine. NTBC (2-(2-nitro-4-trifluoro- methylbenzoyl)-1,3-cyclohexanedione) treatment which improves hepatic and renal function. Liver transplantation when indicated to prevent hepatocellular carcinoma. Vitamin D to heal rickets. Other Unpleasant odor due to accumulation of methionine. Sometimes described as “cabbage-like” odor. Physical phenotype No abnormalities present at birth. -
ACVIM Giger Cyst+Fanconi 2014F
UPDATES ON CYSTINURIA AND FANCONI SYNDROME: AMINO ACIDURIAS IN DOGS Urs Giger, DACVIM-SA, DECVIM CA, DECVCP, Ann-Kathrin Brons, Caitlin A Fitzgerald, Jeffrey Slutsky, Karthik Raj, Victor Stora, Adrian C Sewell and Paula S Henthorn Philadelphia, PA Introduction Disorders of the renal proximal tubules can cause selective or generalized aminoaciduria and may be associated with urinary losses of other solutes such as glucose, lactate, electrolytes and bicarbonate. Two renal tubular defects involving amino acids have long been recognized in dogs, namely cystinuria, leading to cystine calculi and urinary obstruction, and Fanconi syndrome, progressing to renal failure if untreated. Both hereditary disorders have been investigated at the molecular level and are more complex than originally anticipated. Furthermore, the ingestion of Chinese jerky treats has recently been found to be associated with Fanconi syndrome in many dogs and rarely cats. The current understanding of pathophysiology, clinicopathological findings, diagnosis, and therapeutic options will be presented. Fanconi Syndrome Fanconi syndrome, named after the Swiss pediatrician Guido Fanconi and also known as Fanconi’s syndrome or Fanconi disease, should not be confused with Fanconi anemia, a bone marrow disorder in humans. Fanconi syndrome represents a majorproximal renal tubular defect, which hampers the adequate reabsorption of glucose, amino acids, bicarbonate, sodium, calcium, phosphate, lactate, ketones, and carnitine. This rather general loss of multiple functions of the proximal renal tubules can be associated with renal tubular acidosis and lead to progressive renal failure if left untreated. In the renal tubules there are multiple co- transporters for sodium and glucose, amino acids, calcium, and inorganic phosphorus and a sodium/hydrogen ion antiporter, which, depending upon the concentration gradient established by the sodium-potassium pump, move hydrogen ions into the urine. -

Adult Complications of Nephropathic Cystinosis: a Systematic Review
Pediatric Nephrology https://doi.org/10.1007/s00467-020-04487-6 REVIEW Adult complications of nephropathic cystinosis: a systematic review Rachel Nora Kasimer1 & Craig B Langman1 Received: 25 November 2019 /Revised: 18 January 2020 /Accepted: 20 January 2020 # IPNA 2020 Abstract While nephropathic cystinosis is classically thought of as a childhood disease, with improved treatments, patients are more commonly living into adulthood. We performed a systematic review of the literature available on what complications this population faces as it ages. Nearly every organ system is affected in cystinosis, either from the disease itself or from sequelae of kidney transplantation. While cysteamine is known to delay the onset of end-stage kidney disease, its effects on other complications of cystinosis are less well determined. More common adult-onset complications include myopathy, diabetes, and hypothyroidism. Some less common complications, such as neurologic dysfunction, can still have a profound impact on those with cystinosis. Areas for further research in this area include additional study of the impact of cysteamine on the nonrenal manifestations of cystinosis, as well as possible avenues for new and novel treatments. Keywords Cystinosis . Adult complications . Chronic kidney disease . Fanconi syndrome . Cardiovascular disease . Endocrinopathies Introduction live well into the adult years if treated early after diagnosis with a cystine-depleting agent. Since the outlook for living Nephropathic cystinosis (OMIM #219800 and 219900) is a into adulthood is now more a reality than ever before, we rare autosomal recessive disorder due to one of over a hundred undertook a systematic review to ascertain what is known known mutations in the lysosomal cystine transporter, about adult complications, and to set the stage for future cystinosin, and is the most frequent cause of an inherited renal studies.