Obstetrics & Gynecology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fearful Symmetries: Essays and Testimonies Around Excision and Circumcision. Rodopi
Fearful Symmetries Matatu Journal for African Culture and Society ————————————]^——————————— EDITORIAL BOARD Gordon Collier Christine Matzke Frank Schulze–Engler Geoffrey V. Davis Aderemi Raji–Oyelade Chantal Zabus †Ezenwa–Ohaeto TECHNICAL AND CARIBBEAN EDITOR Gordon Collier ———————————— ]^ ——————————— BOARD OF ADVISORS Anne V. Adams (Ithaca NY) Jürgen Martini (Magdeburg, Germany) Eckhard Breitinger (Bayreuth, Germany) Henning Melber (Windhoek, Namibia) Margaret J. Daymond (Durban, South Africa) Amadou Booker Sadji (Dakar, Senegal) Anne Fuchs (Nice, France) Reinhard Sander (San Juan, Puerto Rico) James Gibbs (Bristol, England) John A. Stotesbury (Joensuu, Finland) Johan U. Jacobs (Durban, South Africa) Peter O. Stummer (Munich, Germany) Jürgen Jansen (Aachen, Germany) Ahmed Yerma (Lagos, Nigeria)i — Founding Editor: Holger G. Ehling — ]^ Matatu is a journal on African and African diaspora literatures and societies dedicated to interdisciplinary dialogue between literary and cultural studies, historiography, the social sciences and cultural anthropology. ]^ Matatu is animated by a lively interest in African culture and literature (including the Afro- Caribbean) that moves beyond worn-out clichés of ‘cultural authenticity’ and ‘national liberation’ towards critical exploration of African modernities. The East African public transport vehicle from which Matatu takes its name is both a component and a symbol of these modernities: based on ‘Western’ (these days usually Japanese) technology, it is a vigorously African institution; it is usually -

Microperforated Hymen Presenting Spontaneous Pregnancy with Cesarean Delivery and Hymenotomy Surgery: a Case Report
ID Design Press, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2018 Mar 15; 6(3):528-530. https://doi.org/10.3889/oamjms.2018.123 eISSN: 1857-9655 Case Report Microperforated Hymen Presenting Spontaneous Pregnancy with Cesarean Delivery and Hymenotomy Surgery: A Case Report Brikene Elshani1, Heroid Arifi1, Armond Daci2* 1Department of Obstetrics and Gynecology, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo; 2Department of Pharmacy, Faculty of Medicine, University of Prishtina, Prishtina, Kosovo Abstract Citation: Elshani B, Arifi H, Daci A. Microperforated BACKGROUND: Female genital tract anomalies including imperforate hymen affect sexual life and fertility. Hymen Presenting Spontaneous Pregnancy with Cesarean Delivery and Hymenotomy Surgery: A Case Report. Open Access Maced J Med Sci. 2018 Mar 15; CASE PRESENTATION: In the present case, we describe a pregnant woman diagnosed with imperforate hymen 6(3):528-530. https://doi.org/10.3889/oamjms.2018.123 which never had penetrative vaginal sex. A 27–year-old married patient with 2 months of amenorrhea presented Keywords: Cesarean Delivery; Imperforate Hymen; in a clinic without any other complications. Her history of difficult intercourse and prolonged menstrual flow were Hymen Incision Surgery reported, and subsequent vaginal examination confirmed the diagnosis of imperforate hymen even though she *Correspondence: Armond Daci. Department of claims to made pinhole surgery in hymen during puberty. Her urine pregnancy test was positive, and an Pharmacy, Faculty of Medicine, University of Prishtina, ultrasound examination revealed 8.3 weeks pregnant. The pregnancy was followed up to 39.5 weeks when she Prishtina, Kosovo. E-mail: [email protected] entered in cesarean delivery in urgency. -

Current Fee Schedule 2018 11 01
Procedure Procedure Unit Charge in Procedure Description Code Modifier Dollars 10021 PR FINE NEEDLE ASP;W/O IMAGING GUIDANCE 247.00 10022 PR FINE NEEDLE ASP;W/IMAGING GUIDANCE 494.00 10040 PR ACNE SURGERY OF SKIN ABSCESS 203.00 10060 PR DRAIN SKIN ABSCESS SIMPLE 240.00 10061 PR DRAIN SKIN ABSCESS COMPLIC 328.00 10080 PR DRAIN PILONIDAL CYST SIMPL 261.00 10081 PR DRAIN PILONIDAL CYST COMPLIC 1248.00 10120 PR REMOVE FOREIGN BODY SIMPLE 360.00 10121 PR REMOVE FOREIGN BODY COMPLIC 616.00 10140 PR DRAINAGE OF HEMATOMA/FLUID 1343.00 10160 PR PUNCTURE DRAINAGE OF LESION 240.00 10180 PR COMPLEX DRAINAGE, WOUND 505.00 11000 PR DEBRIDEMENT, INFECTED SKIN, UP TO 10% BSA 321.00 11004 PR DEBRIDE NECR SKIN/TISS,SUBQ/MUSC/FASC,GENIT& 1378.00 11005 PR DEBRIDE NECROTIC SKIN/ TISSUE, ABD WALL 1757.00 11006 PR DEBR NEC SKIN/TISS,GEN/PERI/ADB WALL W/WO C 1592.00 11008 PR REMOVE MESH FROM ABD WALL FOR INFECTION 617.00 11010 PR DEBRIDE ASSOC OPEN FX/DISLOC SKIN/SUBQ 1118.00 11011 PR DEBRIDE ASSOC OPEN FX/DISLOC SKIN/MUSCLE 1217.00 11012 PR DEBRIDE ASSOC OPEN FX/DISLO SKIN/MUS/BONE 1632.00 11040 PR DEBRIDEMENT, SKIN, PARTIAL THICKNESS 91.00 11041 PR DEBRIDEMENT, SKIN, FULL THICKNESS 343.00 11042 PR DEBRIDEMENT, SKIN, SUB-Q TISSUE,=<20 SQ CM 322.00 11043 PR DEBRIDEMENT, SKIN, SUB-Q TISSUE,MUSCLE,=<20 SQ CM 451.00 11044 PR DEBRIDEMENT, SKIN, SUB-Q TISSUE,MUSCLE,BONE,=<20 SQ CM 679.00 11045 PR PR DEBRIDEMENT, SKIN, SUB-Q TISSUE,EACH ADD 20 SQ CM 96.00 11046 PR PR DEBRIDEMENT, SKIN, SUB-Q TISSUE,MUSCLE,EACH ADD 20 SQ CM 168.00 11047 PR PR DEBRIDEMENT, SKIN, SUB-Q -

Anesthesia Section
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN – PROCEDURE CODES SECTION 5 - SURGERY Physician – Procedure Codes, Section 5 - Surgery _____________________________________________________________________________ Table of Contents SURGERY SECTION -----------------------------------------------------------------------------2 GENERAL INFORMATION AND RULES -------------------------------------------------2 SURGERY SERVICES ----------------------------------------------------------------------------8 GENERAL -----------------------------------------------------------------------------------------8 INTERGUMENTARY SYSTEM --------------------------------------------------------------8 MUSCULOSKELETAL SYSTEM ---------------------------------------------------------- 30 RESPIRATORY SYSTEM ------------------------------------------------------------------- 90 CARDIOVASCULAR SYSTEM ---------------------------------------------------------- 102 HEMIC AND LYMPHATIC SYSTEMS ------------------------------------------------- 141 MEDIASTINUM AND DIAPHRAGM ---------------------------------------------------- 144 DIGESTIVE SYSTEM ----------------------------------------------------------------------- 144 URINARY SYSTEM ------------------------------------------------------------------------- 180 MALE GENITAL SYSTEM ---------------------------------------------------------------- 193 REPRODUCTIVE SYSTEM PROCEDURES ----------------------------------------- 200 FEMALE GENITAL SYSTEM ------------------------------------------------------------ 200 MATERNITY CARE -

Obstetrics/Gynecology & Subspecialties
PAGE 1 OF 6 Fairview Health Services OBSTETRICS/GYNECOLOGY & SUBSPECIALTIES Delineation of Privileges Applicant’s Name (please print): Must be an MD/DO and have completed Threshold Criteria listed in the individual privilege sections. Completion of an ACGME or AOA approved residency and fellowship program (as applicable) is required. Current board certification by an American Board of Medical Specialties (ABMS) approved board or AOA/RCPSC approved board, or admissible for examination for certification and certification must be achieved within the time frame mandated by the appropriate board or within five (5) years after completion of residency training for those specialties where time frames are not mandated. CROSSWALK FOR REQUESTING FAIRVIEW PRIVILEGES I Want to Work at the Following Fairview Entity I need to the following Fairview Entity Box on Privilege Form Inpatient/hospital(s) Individual Fairview hospital(s) Fairview Maple Grove Medical Center University of Minnesota Medical Center, Fairview (UMMC) (Ambulatory Care Center) 1, 2 Fairview Maple Grove Ambulatory Surgery Center 1 Fairview Maple Grove Ambulatory Surgery Center (MGASC) Fairview Hospital-Based Clinic (such as UMMC Clinics, Fairview Ridges Specialty Clinic for Individual Fairview hospital where clinic is affiliated Children, Fairview Southdale Oncology Clinic, Fairview Southdale Hospital Breast Center) 1, 3 Fairview Free-Standing Ambulatory Clinics 1 Fairview Group Practice Ambulatory Clinics (FV Clinics) 1 Ambulatory privileges to practice at Fairview hospital-based clinics and other non-hospital-based Fairview owned entities are only available to those practitioners authorized by Fairview to practice at those sites. Ambulatory privileges do not include performance of procedures which are not otherwise available or performed at the individual ambulatory sites as determined by the operational manager or other appropriate personnel. -

Imperforate Hymen Presenting with Massive Hematometra and Hematocolpos
logy & Ob o st ec e tr n i y c s G Okafor et al., Gynecol Obstet (Sunnyvale) 2015, 5:10 Gynecology & Obstetrics DOI: 10.4172/2161-0932.1000328 ISSN: 2161-0932 Case Report Open Access Imperforate Hymen Presenting with Massive Hematometra and Hematocolpos: A Case Report Okafor II*, Odugu BU, Ugwu IA, Oko DS, Enyinna PK and Onyekpa IJ Department of Obstetrics and Gynecology, Enugu State University Teaching Hospital, Enugu, Nigeria Abstract Background: Imperforate hymen is the commonest congenital anomaly that causes closure of the vagina. Ideally, diagnosis should be made early during fetal and neonatal examinations to prevent symptomatic presentations of its complications at puberty. Case report: We report a case of a 15-year-old girl who presented with delayed menarche, eight-month history of cyclic abdominal pain, and a three-week history of lower abdominal swelling. A doctor prescribed anthelmintic and analgesic drugs to her a month ago before she was verbally referred to ESUT Teaching Hospital, Enugu. The development of her secondary sexual characteristics was normal for her age. A 20 cm-sized suprapubic mass, and a bulging pinkish imperforate hymen were found on examination. Her transabdominal ultrasound revealed massive hematometra and hematocolpos. She had virginity-preserving hymenotomy and evacuation of about 1000 mls of accumulated coffee-colored menstrual blood. Conclusion: Clinicians should have high index of suspicion of imperforate hymen when assessing cases of delayed menarche with cyclic lower abdominal pain to prevent the consequences of its delayed treatment like massive hematometra and hematocolpos. Keywords: Imperforate hymen; Hematometra; Hematocolpos; of an imperforate hymen who presented late with delayed menarche, Hymenotomy; Enugu; Nigeria massive hematocolpos and hematometra. -

Physicians As Assistants at Surgery: 2016 Update
Physicians as Assistants at Surgery: 2016 Update Participating Organizations: American College of Surgeons American Academy of Ophthalmology American Academy of Orthopaedic Surgeons American Academy of Otolaryngology – Head and Neck Surgery American Association of Neurological Surgeons American Pediatric Surgical Association American Society of Colon and Rectal Surgeons American Society of Plastic Surgeons American Society of Transplant Surgeons American Urological Association Congress of Neurological Surgeons Society for Surgical Oncology Society for Vascular Surgery Society of American Gastrointestinal Endoscopic Surgeons The American College of Obstetricians and Gynecologists The Society of Thoracic Surgeons Physicians as Assistants at Surgery: 2016 Update INTRODUCTION This is the seventh edition of Physicians as Assistants at Surgery, a study first undertaken in 1994 by the American College of Surgeons and other surgical specialty organizations. The study reviews all procedures listed in the “Surgery” section of the 2016 American Medical Association’s Current Procedural Terminology (CPT TM). Each organization was asked to review new codes since 2013 that are applicable to their specialty and determine whether the operation requires the use of a physician as an assistant at surgery: (1) almost always; (2) almost never; or (3) some of the time. The results of this study are presented in the accompanying report, which is in a table format. This table presents information about the need for a physician as an assistant at surgery. Also, please note that an indication that a physician would “almost never” be needed to assist at surgery for some procedures does NOT imply that a physician is never needed. The decision to request that a physician assist at surgery remains the responsibility of the primary surgeon and, when necessary, should be a payable service. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -
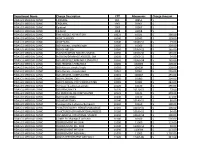
Department Name Charge Description CPT Mnemonic Charge Amount
Department Name Charge Description CPT Mnemonic Charge Amount FIDALGO MEDICAL CLINIC EPIDURAL 851 00851 $ - FIDALGO MEDICAL CLINIC EPIDURAL 1961 01961 $ - FIDALGO MEDICAL CLINIC Epidural 1967 01967 $ - FIDALGO MEDICAL CLINIC Epidural 1968 01968 $ - FIDALGO MEDICAL CLINIC FINE NEEDLE ASPIRATION 10021 10021 $ 338.00 FIDALGO MEDICAL CLINIC ACNE SURGERY 10040 10040 $ 139.00 FIDALGO MEDICAL CLINIC ACNE SURG. 10040 10040-51 $ 73.00 FIDALGO MEDICAL CLINIC I&D Abscess, simple/single 10060 10060 $ 228.00 FIDALGO MEDICAL CLINIC I&D OF ABCESS 10060 10060-22 $ 165.00 FIDALGO MEDICAL CLINIC INCISION/DRAIN ABSCESS SIMPLE- 10060 10060-50 $ 165.00 FIDALGO MEDICAL CLINIC INCISION/DRAINAGE ABSCESS; SIM 10060 10060-51 $ 54.00 FIDALGO MEDICAL CLINIC I&D ABSCESS/CARBUNCLE,STAGED,R 10060 10060-58 $ 165.00 FIDALGO MEDICAL CLINIC I&D ABSCESS/CARBUNCLE 10060 10060N $ 228.00 FIDALGO MEDICAL CLINIC I&D Abscess,simple/single 10060 10060R $ 228.00 FIDALGO MEDICAL CLINIC I&D Abscess, complicated 10061 10061 $ 295.00 FIDALGO MEDICAL CLINIC I&D ABSCESS, COMPLICATED 10061 10061R $ 295.00 FIDALGO MEDICAL CLINIC I&D PILONIDAL CYST 10080 10080 $ 204.00 FIDALGO MEDICAL CLINIC I&D PILONIDAL CYST COMPLICATED 10081 10081 $ 243.00 FIDALGO MEDICAL CLINIC Removal fb,subcutan,simple 10120 10120 $ 296.00 FIDALGO MEDICAL CLINIC I&D REMOVAL FB 10120 10120-51 $ 73.00 FIDALGO MEDICAL CLINIC INC REMOVAL FB COMPLICATED 10121 10121 $ 348.00 FIDALGO MEDICAL CLINIC I&D HEMATOMA 10140 10140 $ 171.00 FIDALGO MEDICAL CLINIC I&D HEMATOMA 10140 10140-51 $ 80.00 FIDALGO MEDICAL CLINIC Puncture drain-abscess/hematom 10160 10160 $ 100.00 FIDALGO MEDICAL CLINIC PUNCTURE/ASPIR. -

Outpatient Surgical Procedures – Site of Service: CPT/HCPCS Codes
UnitedHealthcare® Commercial Policy Appendix: Applicable Code List Outpatient Surgical Procedures – Site of Service: CPT/HCPCS Codes This list of codes applies to the Utilization Review Guideline titled Effective Date: August 1, 2021 Outpatient Surgical Procedures – Site of Service. Applicable Codes The following list(s) of procedure and/or diagnosis codes is provided for reference purposes only and may not be all inclusive. The listing of a code does not imply that the service described by the code is a covered or non-covered health service. Benefit coverage for health services is determined by the member specific benefit plan document and applicable laws that may require coverage for a specific service. The inclusion of a code does not imply any right to reimbursement or guarantee claim payment. Other Policies and Guidelines may apply. This list contains CPT/HCPCS codes for the following: • Auditory System • Female Genital System • Musculoskeletal System • Cardiovascular System • Hemic and Lymphatic Systems • Nervous System • Digestive System • Integumentary System • Respiratory System • Eye/Ocular Adnexa System • Male Genital System • Urinary System CPT Code Description Auditory System 69100 Biopsy external ear 69110 Excision external ear; partial, simple repair 69140 Excision exostosis(es), external auditory canal 69145 Excision soft tissue lesion, external auditory canal 69205 Removal foreign body from external auditory canal; with general anesthesia 69222 Debridement, mastoidectomy cavity, complex (e.g., with anesthesia or more -

Imperforate Hymen Causing Hematocolpos and Acute Urinary Retention in an Adolescent Girl
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Available online at www.sciencedirect.com Taiwanese Journal of Obstetrics & Gynecology 50 (2011) 118e120 www.tjog-online.com Research Letter Imperforate hymen causing hematocolpos and acute urinary retention in an adolescent girl Cihangir Mutlu Ercan*, Kazim Emre Karasahin, Ibrahim Alanbay, Mustafa Ulubay, Iskender Baser Department of Obstetrics and Gynecology, Gulhane Military Medical Academy, Ankara, Turkey Accepted 7 September 2009 Pelvic and abdominal pain is especially common in cyclic pelvic pain continuing for more than 1-year period. adolescent age group. Differential diagnosis could be gastro- Although the secondary sexual characteristics seemed to be intestinal, renal, gynecological, and psychosomatic causes. The normally developed, she had not experienced menarche yet. Her inability to pass urine, which is termed as acute urinary reten- breast development and axillary and pubic hairs were at Tanner tion (AUR), is an uncommon cause of pelvic pain. The etiology stage 3. We learned from her anamnesis that she did not have of AUR is age dependent; and in childhood, severe voiding any sexual intercourse. dysfunction may be drug induced with antihistamines or anti- On her physical examination, we palpated a tender mass in cholinergic drugs, psychogenic, related to viral infections, the pelvic region, which extended to the umbilicus level. On congenital anomalies, neurological bladders, or mechanical auscultation, active bowel movements were heard. On gyne- compression of the urethra via the mass of pelvis [1,2]. cological examination, a pale blue bulging imperforate hymen Hematocolpos is defined as the accumulation of menstrual completely occluding the vagina were seen (Fig. -
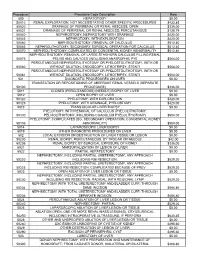
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES