COVID-19) Pandemic—Principles Underlying Prevention
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease. -

Atoltivimab, Maftivimab, and Odesivimab
PATIENT & CAREGIVER EDUCATION Atoltivimab, Maftivimab, and Odesivimab This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. What is this drug used for? It is used to treat infections caused by Ebolavirus. What do I need to tell my doctor BEFORE I take this drug? If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you are breast-feeding. Do not breast-feed while you take this drug. This drug may interact with other drugs or health problems. Tell your doctor and pharmacist about all of your drugs (prescription or OTC, natural products, vitamins) and health problems. You must check to make sure that it is safe for you to take this drug with all of your drugs and health problems. Do not start, stop, or change the dose of any drug without checking with your doctor. Atoltivimab, Maftivimab, and Odesivimab 1/5 What are some things I need to know or do while I take this drug? Tell all of your health care providers that you take this drug. This includes your doctors, nurses, pharmacists, and dentists. Talk with your doctor before getting any vaccines. Use of some vaccines with this drug may either raise the chance of an infection or make the vaccine not work as well. Tell your doctor if you are pregnant or plan on getting pregnant. -

October 2020
PharmNOTES Summary about new FDA-approved products, new indications, first-time generics, and WHAT IS IN THE PIPELINE. From: OCTOBER 2020 Date: 11/06/2020 ©2020 PharmPix. All rights reserved Table of Contents Page News 3 New FDA Approved Products 4-5 Inmazeb™ (atoltivimab, maftivimab, and odesivimab-ebgn) 4 Veklury™ (remdesivir) 5 New FDA Approved Formulations, Dosage Forms, Combination Products and Other Differences 6 New FDA Approved Indications 7 New First-Time Generic Drug Approval 8 Pipeline 9 References 10 2 NEWS ……………………………………………………………………………………………………………... Drug issue Date Details Avoid Use of NSAIDs in 10/15/2020 The FDA issued a warning to avoid the use of Non-steroidal Anti-inflammatory Drugs (NSAIDs) during pregnancy at 20 weeks or Pregnancy at 20 Weeks later. The use of NSAIDs around 20 weeks or later in pregnancy may cause serious kidney problems in the fetus, low levels of or Later amniotic fluids, and other complications. Previously NSAIDs labels warned to avoid use during the last three (3) months of pregnancy due to the risk of premature closure of the fetal ductus arteriosus. The FDA now requires changes in the prescribing information for both prescription and over the counter (OTC) NSAIDs. Recommendations for healthcare professionals: • Advise pregnant women to avoid the use of NSAIDs at 20 weeks of pregnancy or later. • If NSAIDs are necessary during 20 to 30 weeks of pregnancy, limit treatment to the lowest dose possible and for the shortest duration. Consider ultrasound monitoring of amniotic fluid if treatment extends over 48 hours. If low levels of amniotic fluid are identified, discontinue the NSAID. -

A Short Overview of Ebola Virus Disease
Short Communication Journal of Volume 6:4, 2021 DOI: 10.37421/jidm.2021.6.173 Infectious Diseases and Medicine A Short Overview of Ebola Virus Disease Akshay Thiwari* Department of Virology, University of Hyderabad, Hyderabad, Telangana, India Ebola [1] is an uncommon but lethal virus that causes fever, body Treatment for Ebola aches, diarrhea, and, in some cases, internal and external bleeding. The Ebola has no known cure, though researchers are working on one. For immune system and organs are harmed as the virus spreads through the the treatment of Ebola [2], two drug therapies have been authorized. Inmazeb body. As a result, the number of blood-clotting cells decreases. As a is a compound that consists of three monoclonal antibodies (atoltivimab, consequence, there is a lot of uncontrollable bleeding. Ebola hemorrhagic maftivimab, and odesivimab-ebgn). Ebanga (ansuvimab-zykl) is a monoclonal fever was the previous name for the outbreak, but it is now known as Ebola antibody that is given as an injection. It aids in stopping the virus from reaching virus. It kills up to 90% of those who become infected. the cell receptor. Doctors treat Ebola symptoms [3] with the following How does one contract Ebola? medication. Ebola isn't as infectious as viruses like the common cold, influenza, or Electrolytes and fluids, Oxygen (O2), Medication for high blood pressure, measles. Contact with the skin or bodily fluids of an infected animal, such as Transfusions of blood, and other diseases'. a monkey, chimp, or fruit bat, transmits the disease to humans. Then it Facts on Ebola passes from one person to the next in the same manner. -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -
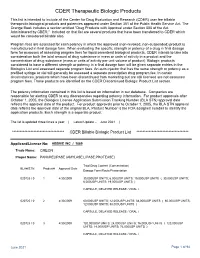
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

Risk Assessment and Risk Mitigation Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761169Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRM) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type BLA Application Number 761169 PDUFA Goal Date October 25, 2020 OSE RCM # 2020-264 Reviewer Name(s) Elizabeth Everhart, MSN, RN, ACNP Team Leader Naomi Boston, PharmD Acting Deputy Division Doris Auth, PharmD Director Review Completion Date August 10, 2020; date entered into DARRTS, August 20, 2020 Subject Evaluation of Need for a REMS Established Name atoltivimab – odesivimab – maftivimab (REGN-EB3) Trade Name Inmazeb Name of Applicant Regeneron Pharmaceuticals, Inc. Therapeutic Class Human IgG monoclonal antibody Formulation Solution for infusion Dosing Regimen 50 mg of each mAb/kg (3mL/kg) IV (b) (4) × 1 1 Reference ID: 4659652 Table of Contents EXECUTIVE SUMMARY ............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background .........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

761169Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761169Orig1s000 OTHER REVIEW(S) LABEL AND LABELING REVIEW Division of Medication Error Prevention and Analysis (DMEPA) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) *** This document contains proprietary information that cannot be released to the public*** Date of This Review: October 7, 2020 Requesting Office or Division: Division of Antivirals (DAV) Application Type and Number: BLA 761169 Product Name, Dosage Form, Inmazeb (atoltivimab, maftivimab, and odesivimab-ebgn) and Strength: Injection 241.7 mg/241.7 mg/241.7 mg per 14.5 mL (16.67 mg/16.67 mg/16.67 mg per mL) Product Type: Multi-Ingredient Product Rx or OTC: Prescription (Rx) Applicant/Sponsor Name: Regeneron Pharmaceuticals, Inc. (Regeneron) FDA Received Date: February 25, 2020 OSE RCM #: 2020-263 DMEPA Safety Evaluator: Valerie S. Vaughan, PharmD DMEPA Associate Director of Mishale Mistry, PharmD, MPH Nomenclature and Labeling: 1 1 REASON FOR REVIEW As part of the approval process for Inmazeb injection, 241.7 mg/241.7 mg/241.7 mg per 14.5 mL (16.67 mg/16.67 mg/16.67 mg per mL), the Division of Antivirals (DAV) requested that we review the proposed labels and labeling for areas that may lead to medication errors. 2 MATERIALS REVIEWED We considered the materials listed in Table 1 for this review. The Appendices provide the methods and results for each material reviewed. Table 1. Materials Considered for this -

Pipeline Report November 2020
Pipeline Report November 2020 Pipeline Report November 2020 © 2020 AcariaHealth. All rights reserved. Page 1 This quarterly at-a-glance publication is developed by our Clinical Pharmacy Drug Information team to increase your understanding of the drug pipeline, Table of Contents ensuring you’re equipped with insights to prepare for shifts in pharmacy benefit management. In this issue, you’ll learn more about key themes and notable drugs: Recent Drug Approvals 1 > On COVID-19, the FDA granted full approval to Veklury (remdesivir) for the treatment of COVID-19. Veklury is approved for use in hospitalized adults and pediatric patients (≥ 12 years of age and weighing ≥ 40 Upcoming Products 6 kg), and represents the very first therapy to garner full FDA approval for COVID-19. Other therapies will follow, gaining market access through EUA (LLY’s Bamlanivimab and Olumiant, and <likely> Regeneron’s Biosimilars 14 REGN-COV2). With the US crossing the 11 million total coronavirus infection mark, demand for these agents will be high while supply of the antibody treatment will be especially tight. The vaccine race accelerates as there are now two m-RNA based candidates both showing greater than 94% Generic Specialty Agents 15 efficacy in study populations. Both vaccines require 2 doses. Neither has FDA approval, and EUA reviews are pending. Supplies will be limited for months to come. Pfizer has stated it could produce 50 million doses by the end of 2020, and Moderna has promised up to 20 million doses in the same time frame. During 2021 Pfizer forecasts 1.3 billion doses while Moderna states between 500 million and 1 billion. -

Lääkeaineiden Yleisnimet (INN-Nimet) 21.6.2021
Lääkealan turvallisuus- ja kehittämiskeskus Säkerhets- och utvecklingscentret för läkemedelsområdet Finnish Medicines Agency Lääkeaineiden yleisnimet (INN-nimet) 21.6. -

NETTER, Jr., Robert, C. Et Al.; Dann, Dorf- (21) International Application
ll ( (51) International Patent Classification: (74) Agent: NETTER, Jr., Robert, C. et al.; Dann, Dorf- C07K 16/28 (2006.01) man, Herrell and Skillman, 1601 Market Street, Suite 2400, Philadelphia, PA 19103-2307 (US). (21) International Application Number: PCT/US2020/030354 (81) Designated States (unless otherwise indicated, for every kind of national protection av ailable) . AE, AG, AL, AM, (22) International Filing Date: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, 29 April 2020 (29.04.2020) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, (25) Filing Language: English DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, (26) Publication Language: English KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (30) Priority Data: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 62/840,465 30 April 2019 (30.04.2019) US OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, (71) Applicants: INSTITUTE FOR CANCER RESEARCH TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. D/B/A THE RESEARCH INSTITUTE OF FOX CHASE CANCER CENTER [US/US]; 333 Cottman Av¬ (84) Designated States (unless otherwise indicated, for every enue, Philadelphia, PA 191 11-2497 (US). UNIVERSTIY kind of regional protection available) . ARIPO (BW, GH, OF KANSAS [US/US]; 245 Strong Hall, 1450 Jayhawk GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, Boulevard, Lawrence, KS 66045 (US). -

International Nonproprietary Names for Pharmaceutical Substances (INN)
WHO Drug Information, Vol. 32, No. 4, 2018 Proposed INN: List 120 International Nonproprietary Names for Pharmaceutical Substances (INN) Notice is hereby given that, in accordance with article 3 of the Procedure for the Selection of Recommended International Nonproprietary Names for Pharmaceutical Substances, the names given in the list on the following pages are under consideration by the World Health Organization as Proposed International Nonproprietary Names. The inclusion of a name in the lists of Proposed International Nonproprietary Names does not imply any recommendation of the use of the substance in medicine or pharmacy. Lists of Proposed (1–117) and Recommended (1–78) International Nonproprietary Names can be found in Cumulative List No. 17, 2017 (available in CD-ROM only). The statements indicating action and use are based largely on information supplied by the manufacturer. This information is merely meant to provide an indication of the potential use of new substances at the time they are accorded Proposed International Nonproprietary Names. WHO is not in a position either to uphold these statements or to comment on the efficacy of the action claimed. Because of their provisional nature, these descriptors will neither be revised nor included in the Cumulative Lists of INNs. Dénominations communes internationales des Substances pharmaceutiques (DCI) Il est notifié que, conformément aux dispositions de l'article 3 de la Procédure à suivre en vue du choix de Dénominations communes internationales recommandées pour les Substances pharmaceutiques les dénominations ci-dessous sont mises à l'étude par l'Organisation mondiale de la Santé en tant que dénominations communes internationales proposées.