Author Index SOFT 2009 Bold Type
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug-Facilitated Sexual Assault Panel, Blood
DRUG-FACILITATED SEXUAL ASSAULT PANEL, BLOOD Blood Specimens (Order Code 70500) Alcohols Analgesics, cont. Anticonvulsants, cont. Antihistamines, cont. Ethanol Phenylbutazone Phenytoin Cyclizine Amphetamines Piroxicam Pregabalin Diphenhydramine Amphetamine Salicylic Acid* Primidone Doxylamine BDB Sulindac* Topiramate Fexofenadine Benzphetamine Tapentadol Zonisamide Guaifenesin Ephedrine Tizanidine Antidepressants Hydroxyzine MDA Tolmetin Amitriptyline Loratadine MDMA Tramadol Amoxapine Oxymetazoline* Mescaline* Anesthetics Bupropion Pyrilamine Methcathinone Benzocaine Citalopram Tetrahydrozoline Methamphetamine Bupivacaine Clomipramine Triprolidine Phentermine Etomidate Desipramine Antipsychotics PMA Ketamine Desmethylclomipramine 9-hydroxyrisperidone Phenylpropanolamine Lidocaine Dosulepin Aripiprazole Pseudoephedrine Mepivacaine Doxepin Buspirone Analgesics Methoxetamine Duloxetine Chlorpromazine Acetaminophen Midazolam Fluoxetine Clozapine Baclofen Norketamine Fluvoxamine Fluphenazine Buprenorphine Pramoxine* Imipramine Haloperidol Carisoprodol Procaine 1,3-chlorophenylpiperazine (mCPP) Mesoridazine Cyclobenzaprine Rocuronium Mianserin* Norclozapine Diclofenac Ropivacaine Mirtazapine Olanzapine Etodolac Antibiotics Nefazodone Perphenazine Fenoprofen Azithromycin* Nordoxepin Pimozide Hydroxychloroquine Chloramphenicol* Norfluoxetine Prochlorperazine Ibuprofen Ciprofloxacin* Norsertraline Quetiapine Ketoprofen Clindamycin* Nortriptyline Risperidone Ketorolac Erythromycin* Norvenlafaxine Thioridazine Meclofenamic Acid* Levofloxacin* Paroxetine -

Antidepressants
Antidepressants BMF 83 - Antidepressants BMF 83 - Antidepressants Depression is a common psychiatric disorder impacting millions of people worldwide. It is caused by an imbalance of chemicals 1 in the brain, namely serotonin and noradrenaline . Everyone experiences highs and lows, but depression is characterised by 2 persistent sadness for weeks or months . With depression there is lasting feeling of hopelessness, often accompanied by anxiety. Sufferers lose interest in things that they previously enjoyed, and experience bouts of tearfulness. Rational thinking and decision 2 making are impacted. Physical manifestations include tiredness, insomnia, loss of appetite and sex drive, aches and pains . At its worst depression can cause the sufferer to feel suicidal. Depression is usually treated with a combination of counselling and drug therapy. There is also evidence that exercise can help depression. Most people with moderate or severe depression benefit from antidepressant medication. There are a wide range of 3 antidepressants on the market, which can be broadly divided according to mechanism of action ; • Selective serotonin reuptake inhibitors (SSRIs) • Serotonin-norepinephrine reuptake inhibitors (SNRIs) • Serotonin modulator and stimulators (SMSs) • Serotonin antagonist and reuptake inhibitors (SARIs) • Norepinephrine reuptake inhibitors (NRIs or NERIs) • Tetracyclic antidepressants (TeCAs) • Tricyclic antidepressants (TCAs) • Monoamine oxidase inhibitors (MAOIs) www.chiron.no | E-mail: [email protected] | Tel.: +47 73 87 44 90 | Fax.: +47 73 73 87 44 99 | BMF 83 p.1/8 , 10_16 BMF 83 - Antidepressants BMF 83 - Antidepressants 1 Today the most common first choice of medication is a SSRI , i.e. Citalopram, Escitalopram, Fluvoxamine, Paroxetine, Sertraline, Fluoxetine. Antidepressants are not addictive, but can result in withdrawal symptoms when therapy is stopped. -

2016-11-BMF-83 Antidepressants
Antidepressants BMF 83 - Antidepressants BMF 83 - Antidepressants Depression is a common psychiatric disorder impacting millions of people worldwide. It is caused by an imbalance of chemicals 1 in the brain, namely serotonin and noradrenaline . Everyone experiences highs and lows, but depression is characterised by 2 persistent sadness for weeks or months . With depression there is lasting feeling of hopelessness, often accompanied by anxiety. Sufferers lose interest in things that they previously enjoyed, and experience bouts of tearfulness. Rational thinking and decision 2 making are impacted. Physical manifestations include tiredness, insomnia, loss of appetite and sex drive, aches and pains . At its worst depression can cause the sufferer to feel suicidal. Depression is usually treated with a combination of counselling and drug therapy. There is also evidence that exercise can help depression. Most people with moderate or severe depression benefit from antidepressant medication. There are a wide range of 3 antidepressants on the market, which can be broadly divided according to mechanism of action ; • Selective serotonin reuptake inhibitors (SSRIs) • Serotonin-norepinephrine reuptake inhibitors (SNRIs) • Serotonin modulator and stimulators (SMSs) • Serotonin antagonist and reuptake inhibitors (SARIs) • Norepinephrine reuptake inhibitors (NRIs or NERIs) • Tetracyclic antidepressants (TeCAs) • Tricyclic antidepressants (TCAs) • Monoamine oxidase inhibitors (MAOIs) www.chiron.no | E-mail: [email protected] | Tel.: +47 73 87 44 90 | Fax.: +47 73 73 87 44 99 | BMF 83 p.1/8 , 10_16 BMF 83 - Antidepressants BMF 83 - Antidepressants 1 Today the most common first choice of medication is a SSRI , i.e. Citalopram, Escitalopram, Fluvoxamine, Paroxetine, Sertraline, Fluoxetine. Antidepressants are not addictive, but can result in withdrawal symptoms when therapy is stopped. -

An Update on Therapeutic Drug Monitoring and Pharmacogenetic Testing for the Optimization of Therapy with Psychiatric Medication
J Lab Med 2014; aop Review Katharina M. Rentsch* An update on therapeutic drug monitoring and pharmacogenetic testing for the optimization of therapy with psychiatric medication DOI 10.1515/labmed-2014-0032 Keywords: antidepressants; antipsychotic drugs; cyto- Received September 28, 2013; accepted January 28, 2014 chrome; pharmacogenetics; psychiatric medication. Abstract: Therapeutic drug monitoring of psychiatric medication as well as pharmacogenetic testing is per- formed more and more frequently in numerous labora- Introduction tories. In this review, a summary of the literature in the years 2011 and 2012 has been completed. The guidelines The Therapeutic Drug Monitoring (TDM) of psychophar- of the German AGNP (Association for Neuropsychop- maceutical drugs is carried out in numerous laboratories harmacology and Pharmacopsychiatry) contain all the to an ever more frequent extent, as are pharmacogenetic information needed for the interpretation of drug concen- studies. Based on numerous studies that have shown that trations. The determination of serotonin in urine could pharmacogenetic polymorphisms, among other factors, be a marker for the assessment of the response of antide- cause large inter-individual differences in the pharma- pressants, and correlations between the occupancy of the cokinetics of psychopharmaceutical drugs, doctors who target receptors in the brain and drug concentration have prescribe such drugs increasingly order TDM tests. As part been established using positron emission tomography. of the diagnostics updates 2013 [1] a compilation of the The influence of age on drug concentrations has been literature on the above topics published in 2011 and 2012 controversially described, and additionally females have was prepared, and the individual papers and studies were always showed a slower metabolism and higher serum evaluated. -

Method Validation of a Tricyclic Antidepressant Drug Panel in Urine by LC-MS/MS
Method Validation of a Tricyclic Antidepressant Drug Panel in Urine by LC-MS/MS Chia-Ni Lin, 1 JoEtta M. Juenke, 2 and Kamisha L. Johnson –Davis1,2. 1Department of Pathology, University of Utah School of Medicine, Salt Lake City, UT USA, 2ARUP Institute for Clinical and Experimental Pathology, Salt Lake City, UT USA Introduction Imprecision Method Comparison Tricyclic antidepressants (TCA) can cause serious cardiac complications and Imprecision was determined by analyzing three levels of control material To evaluate accuracy, drug-free urine was pooled and used as a matrix to spike 22 samples with TCA at can be lethal if misused at high doses; as a result, TCA should be monitored. To prepared in quintuplicate at five concentrations for five days (n = 25 for each different concentrations. An additional 33 patient samples were collected and sent to an alternate monitor patient compliance to therapy, urine specimens may be preferred since concentration). laboratory for split sample comparison by gas chromatography-mass spectrometry (GC/MS). Out of a total the collection is non-invasive and the specimen can provide a longer detection of 55 results, there were three false negative results for nortriptyline and two false negative results for window. TCA are frequently monitored by immunoassay; however false Expected Mean Within Run Between Day Total amitriptyline, when compared to compared GC/MS method. The false negative results could be due to the positives and cross reactivity to other cyclic compounds may compromise Drug Sample N (ng/mL) (ng/mL) SD CV (%) SD CV (%) SD CV (%) different sample preparations and positive cut-off concentrations between the two laboratories. -

TOX.LC.3499 Rev 07, Effective 2015-08-12 to Present
Harris County Institute of Forensic Sciences Section: Toxicology Approved By: Chief Toxicologist Document Type: LC & LCMSMS Procedure No.: TOX.LC.3499 Title: Amitriptyline, Clozapine, Doxepin, Fluoxetine, Quetiapine and Olanzapine Rev.7 (LLE) by LCMSMS 1.0 Purpose 1.1 Amitriptyline, Nortriptyline, Clozapine, Doxepin, Nordoxepin (Desmethyldoxepin), Fluoxetine, Norfluoxetine, Quetiapine, Norquetiapine, and Olanzapine are assayed by High Performance Liquid Chromatography/Mass Spectrometry/Mass Spectrometry (HPLC/MS/MS) using multiple reaction monitoring (MRM) and their corresponding deuterated standards. 2.0 Scope 2.1 The analysis is applicable to all types of forensic specimens when compared with matrix matched controls. 3.0 Definitions and Abbreviations 3.1 None Applicable 4.0 Materials 4.1 Instruments and Equipment 4.1.1 Pipettes 4.1.2 13 x 100 mm screw cap test tubes 4.1.3 16 x 100 mm test tubes 4.1.4 Vortex mixer 4.1.5 Centrifuge 4.1.6 Autosampler vials 4.1.7 Vial caps with puncture seals 4.1.8 Solvent evaporator 4.1.9 Nitrogen compressed gas 4.1.10 0.2 m Filters 4.1.11 3 c.c. Syringe 4.1.12 C18 PLC column 4.1.13 LC-MS/MS 4.2 Reagents 4.2.1 Methanol, HPLC grade 4.2.2 n-Butyl Chloride, HPLC grade 4.2.3 Acetonitrile, HPLC grade 4.2.4 Formic Acid 88% 4.2.5 Water, 18.2 mega ohm or HPLC grade 4.2.6 Ammonium formate. Page 1 of 12 Harris County Institute of Forensic Sciences Section: Toxicology Approved By: Chief Toxicologist Document Type: LC & LCMSMS Procedure No.: TOX.LC.3499 Title: Amitriptyline, Clozapine, Doxepin, Fluoxetine, Quetiapine and Olanzapine Rev.7 (LLE) by LCMSMS 4.2.7 Saturated Sodium Borate Buffer A. -

Complete Article
_J Clin Pathol 1999;52:713-718 713 Leader Detection of drug misuse an addictive challenge. John H Galloway, Ian D Marsh Abstract base: "crack"). In addition to these illicit It is now accepted that drug misuse is a compounds various drugs intended for medical large and growing problem in the United use have been "adopted" into misuse. In Kingdom, some estimates of the number particular the benzodiazepines (diazepam and of regular illicit drug users being as high temazepam) are widely misused, as are opiates as three million. The aim of this paper is including diamorphine (heroin) and dihydroco- to provide insight into the methods used to deine. Ketamine, methadone, tricyclic antide- detect drug misuse. The strategy adopted pressants, and dextropropoxyphene are further by one laboratory is described and meth- examples of prescribed drugs encountered in ods of screening for, and identification of, individuals who have not been prescribed them. a wide range of compounds are provided. The casual use of these drugs may never be a No claim is made that this is the best problem and is, for many, a natural part of rec- approach or that the list of drugs detected reational activity. The use of these drugs is comprehensive; the range of drugs becomes a problem only if the individual encountered is always increasing and the involved becomes a habitual user and suffers lists are constantly updated. It is hoped longer term physical problems (illness and that users of toxicology laboratory serv- infections) and psychological problems which ices will gain an appreciation of the capa- make them unable to be fully active and bilities and limitations of the techniques productive members of society. -

Quantification of Tricyclic Antidepressants in Human Plasma Or Serum by LC-HRAM(MS) for Clinical Research
TECHNICAL NOTE 73330 Quantification of tricyclic antidepressants in human plasma or serum by LC-HRAM(MS) for clinical research Authors: Claudio De Nardi1, Katharina Kern2, Steffen Peters2 1Thermo Fisher Scientific GmbH, Dreieich, Germany 2RECIPE Chemicals + Instruments GmbH, Munich, Germany Keywords: Tricyclic antidepressants, offline sample preparation, plasma, serum, Orbitrap, high-resolution mass spectrometry Application benefits • Increased accuracy of method by implementation of a comprehensive ClinMass® kit for sample preparation Goal Implementation of an analytical method for the • High-resolution mass spectrometry for improved quantification of 13 different tricyclic antidepressants selectivity in human plasma or serum on a Thermo Scientific™ ™ ™ • Robust, sensitive hardware enables increased Q Exactive Plus hybrid quadrupole-Orbitrap mass confidence in data spectrometer. • Simple offline sample preparation by protein precipitation Introduction Tricyclic antidepressants (TCAs) are commonly used • 13 tricyclic antidepressants in a single quantitative to treat depression, anxiety reactions, and neuropathic method pain, despite the risk of severe side effects. Monitoring serum concentrations of TCAs can assess suspected toxicity, and/or drug-drug interactions. High-pressure Plasma or serum samples were extracted by offline internal liquid chromatography (HPLC) with ultraviolet (UV) standard addition and protein precipitation. Extracted spectrophotometric detection has been the recommended samples were injected onto a Thermo Scientific™ -

Antidepressant Drugs-1
Module: CNS Subject: Pharmacology Lecture: MBBS Antidepressant Drugs-1 Dr Biswadeep Das Assoc Prof(Pharmacology) Department of Pharmacology/AIIMS Rishikesh [email protected] Mental Depression… What is it ? What is Mental Depression ?-Mood Disorder Pleasure seeking = Hedonistic Inability to experience pleasure = Anhedonia Disorders of Mood (Affective Disorders) • Depression (unipolar depression) • Mania • Reactive depression (75%) • Endogenous depression (25%) • Manic-depression (bipolar depression) What are the possible mechanisms of depression ? • Depression is associated with insufficient central release of NE and 5-HT • Led to development of the Biogenic Amine Hypothesis Antidepressant Drugs-Classification n Tricyclic Agents ¨Imipramine/Desipramine/ Clomipramine/ Amitriptyline/Nortriptyline/ Protriptyline/Doxepin/ Nordoxepin Antidepressant Drugs-Classification (contd.) n Heterocyclic Agents ¨Unicyclic n Bupropion ¨Tetracyclic n Amoxapine(N-desmethyl loxapine)/Maprotilene/ Mirtazapine n 5-HT2 Antagonists ¨Nefazodone/Trazodone Antidepressant Drugs-Classification (contd.) n Mono-Amine-Oxidase-A Isozyme Inhibitors (MAO-AI’s) ¨Hydrazine group n Isocarboxazid/Phenelzine ¨Nonhydrazine group n Nialamide/Tranylcypromine/Clorgyline/Pargyline/ Moclobemide/Brofaromine/Cimoxatone/Toloxatone Selective Serotonin Reuptake Inhibitors (SSRI’s) n Selective Serotonin Reuptake Inhibitors (SSRI’s) ¨Citalopram/ Escitalopram/ Fluoxetine/ Paroxetine/ Sertraline/ Fluvoxamine Serotonin NE Reuptake Inhibitors (SNRI’s) n Serotonin Norepinephrine Reuptake -

Product Monograph
PRODUCT MONOGRAPH Pr SILENOR® Doxepin tablets 3 and 6 mg doxepin as doxepin hydrochloride Hypnotic Paladin Labs Inc. Date of Preparation: 6111 Royalmount Ave. December 07, 2012 Montreal, Quebec H4P 2T4 Version : 1.3 Submission Control No: 152398 ® Trademark of Pernix Therapeutics LLC. SILENOR Product Monograph Page 1 of 30 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................4 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ....................................................................................................8 DRUG INTERACTIONS ..................................................................................................13 DOSAGE AND ADMINISTRATION ..............................................................................15 OVERDOSAGE ................................................................................................................15 ACTION AND CLINICAL PHARMACOLOGY ............................................................17 STORAGE AND STABILITY ..........................................................................................19 -

Doxepin for Insomnia
Out of the Pipeline p Doxepin for insomnia Dimitri Markov, MD, and Karl Doghramji, MD ow-dose doxepin—3 mg and 6 mg— Table 1 Low-dose doxepin has demonstrated efficacy for insom- may relieve sleep Doxepin: Fast facts Lnia characterized by frequent or early- maintenance morning awakenings and an inability to Brand name: Silenor insomnia and is return to sleep (Table 1).1 FDA-approved in Indication: Insomnia characterized by difficulty not designated March 2010, doxepin (3 mg and 6 mg) is only with sleep maintenance as a controlled the second insomnia medication not des- Approval date: March 2010 ignated as a controlled substance and thus Availability date: September 7, 2010 substance may be of special value in patients with a Manufacturer: Somaxon Pharmaceuticals history of substance abuse. Dosage forms: 3 mg and 6 mg tablets Recommended dosage: 3 mg or 6 mg once Clinical implications daily within 30 minutes of bedtime Ramelteon, the other hypnotic that is not a controlled substance, is indicated for sleep initiation insomnia (ie, inability to fall How it works asleep). In contrast, low-dose doxepin is for Doxepin’s mechanism of action for treat- patients with sleep maintenance insomnia, ing depression and insomnia remains un- which is waking up frequently or early in known. The antidepressant effect of dox- the morning and not falling back asleep.1,2 epin is thought to result from inhibition A tricyclic antidepressant first approved of serotonin and norepinephrine reuptake in 1969, doxepin has long been available in at the synaptic cleft. Animal studies have larger doses (10-, 25-, 50-, 75-, 100-, and 150- shown anticholinergic and antihistamin- mg capsules) to treat depression and anxiety ergic activity with doxepin.2 Doxepin and as a topical preparation (5% cream) for is a potent histamine antagonist—pre- pruritus, but not in dosages <10 mg. -
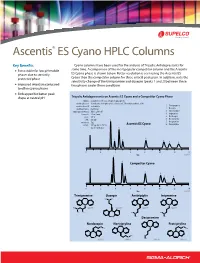
Ascentis® ES Cyano HPLC Columns
Ascentis® ES Cyano HPLC Columns Key Benefits Cyano columns have been used for the analysis of Tricyclic Antidepressants for some time. A comparison of the most popular competitor column and the Ascentis L Extra stable for low pH mobile phases due to sterically ES Cyano phase is shown below. Better resolution is seen using the Ascentis ES protected phase Cyano than the competitor column for three critical peak pairs. In addition, note the selectivity change of the trimipramine and doxepin (peaks 1 and 2) between these L Improved retention compared two phases under these conditions to other cyano phases L Endcapped for better peak shape at neutral pH Tricyclic Antidepressants on Ascentis ES Cyano and a Competitor Cyano Phase column: as indicated; 15 cm x 4.6 mm, 5 μm particle mobile phase A: 10 mM potassium phosphate, dibasic (pH 7.0 with phosphoric acid) mobile phase B: acetonitrile 1. Trimipramine mobile phase C: methanol 2. Doxepin mixing proportions: A:B:C, 25:60:15 3. Amitriptyline flow rate: 2.0 mL/min 4. Imipramine temp.: 25 °C 5. Nordoxepin det.: 215 nm 2 6. Nortriptyline injection: 5 μL Ascentis ES Cyano 7. Desipramine sample: 100 μg /mL in 70:30, 8. Protriptyline water: methanol 3 5 1 4 6 7 8 0 2 4 6 8 10 12 14 2 Min G004971 3 Competitor Cyano 1 5 4 6 7 8 02468101214 Min G004972 Trimipramine Doxepin Amitriptylin Imipramine G004973 G004974 G004975 G004976 Desipramine Nordoxepin Nortriptyline Protriptyline G004977 G004979 G004980 G004978 Extended Stability of Ascentis ES Cyano Compared to Traditional Cyano Columns using Acidic Mobile Phases 2.5 2.0 Ascentis ES Cyano 1.5 k’ Traditional Cyano 1.0 0.5 0 0102030405060 Void Volumes (x 1,000) G004981 Ascentis ES Cyano HPLC Columns Length (cm) ID (mm) Cat.