How Millions of People in West and Central Africa Are Being Left out of the Global Hiv Response
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Cavé in French Swordsmanship Patrick T
COLUMBIACLASSICALFENCING.COM The Cavé in French Swordsmanship Patrick T. Morgan Introduction French fencing masters wrote about the cavé (pronounced cahv-ay) as a distinct fencing action. In French, caver means to cave in or collapse. The cavé thus described how a fencer would change or position his wrist or body to create a sharp angle—“caving in” from, say, a straightened position— for a specific fencing purpose, whether offensive or defensive. Sensibly, then, the cavé is sometimes referred to as angulation today. But that term doesn’t always cover all the ways the French writers used the cavé. This is because, as explained below, you can also cavé by using no angulation. Three General Ways to Cavé For the French, there were three ways to cavé. From the on-guard position, you could cavé (1) at the hips or (2) with your rear leg. You could also (3) cavé the wrist of your sword arm, which itself was possible in three different ways. These methods were variously defensive or offensive. Importantly, these were not recommendations so much as taxonomy: as we’ll see, some of these ways of “cavé-ing” could get you killed. 1. The Cavé at the Hips Danet discussed the “cavation” of the body in the second volume of L’Art des Armes. The cavé of the hips is one of two types of esquive—that is, a movement or displacement of the fencer’s target area to evade a thrust—that Danet identified. As Danet described it, the cavé at the hips occurs by “lowering the shoulders and completely straightening the right knee” (en baissant les épaules, & dépliant tout-à- fait le genou droit). -

PLAN DE RÉPONSE HUMANITAIRE République Centrafricaine
CYCLE DE PROGRAMMATION PLAN DE RÉPONSE HUMANITAIRE 2020 HUMANITAIRE PUBLIÉ EN DECEMBRE 2019 République Centrafricaine 1 PLAN DE REPONSE HUMANITAIRE 2020 | À PROPOS Pour consulter les mises à jour À propos les plus récentes : Ce document est consolidé par OCHA pour le compte de l’Équipe OCHA coordonne l’action humanitaire pour humanitaire pays et des partenaires humanitaires. Il présente les priorités garantir que les personnes affectées par une et les paramètres de la réponse stratégique de l’Équipe humanitaire crise reçoivent l’assistance et la protection dont elles ont besoin. OCHA s’efforce pays, basés sur une compréhension partagée de la crise, énoncés dans de surmonter les obstacles empêchant l’Aperçu des besoins humanitaires. l’assistance humanitaire de joindre les Les désignations employées et la présentation des éléments dans le personnes affectées par des crises et est chef présent rapport ne signifient pas l’expression d’une quelque opinion que de file dans la mobilisation de l’assistance et de ressources pour le compte du système ce soit de la Partie du Secrétariat des Nations unies concernant le statut humanitaire juridique d’un pays, d’un territoire, d’une ville ou d’une zone ou de leurs autorités ou concernant la délimitation de frontières ou de limites. www.unocha.org/car twitter: @OCHA_CAR PHOTO DE COUVERTURE @UNICEF CAR / B. Matous Humanitarian Réponse est destiné à être le site Web central des outils et des services de Gestion de l’information permettant l’échange d’informations entre les clusters et les membres du IASC intervenant dans une crise. car.humanitarianresponse.info Humanitarian InSight aide les décideurs en leur donnant accès à des données humanitaires essentielles. -

Central African Republic Emergency Situation UNHCR Regional Bureau for Africa As of 26 September 2014
Central African Republic Emergency Situation UNHCR Regional Bureau for Africa as of 26 September 2014 N'Djamena UNHCR Representation NIGERIA UNHCR Sub-Office Kerfi SUDAN UNHCR Field Office Bir Nahal Maroua UNHCR Field Unit CHAD Refugee Sites 18,000 Haraze Town/Village of interest Birao Instability area Moyo VAKAGA CAR refugees since 1 Dec 2013 Sarh Number of IDPs Moundou Doba Entry points Belom Ndele Dosseye Sam Ouandja Amboko Sido Maro Gondje Moyen Sido BAMINGUI- Goré Kabo Bitoye BANGORAN Bekoninga NANA- Yamba Markounda Batangafo HAUTE-KOTTO Borgop Bocaranga GRIBIZI Paoua OUHAM 487,580 Ngam CAMEROON OUHAM Nana Bakassa Kaga Bandoro Ngaoui SOUTH SUDAN Meiganga PENDÉ Gbatoua Ngodole Bouca OUAKA Bozoum Bossangoa Total population Garoua Boulai Bambari HAUT- Sibut of CAR refugees Bouar MBOMOU GadoNANA- Grimari Cameroon 236,685 Betare Oya Yaloké Bossembélé MBOMOU MAMBÉRÉ KÉMO Zemio Chad 95,326 Damara DR Congo 66,881 Carnot Boali BASSE- Bertoua Timangolo Gbiti MAMBÉRÉ- OMBELLA Congo 19,556 LOBAYE Bangui KOTTO KADÉÏ M'POKO Mbobayi Total 418,448 Batouri Lolo Kentzou Berbérati Boda Zongo Ango Mbilé Yaoundé Gamboula Mbaiki Mole Gbadolite Gari Gombo Inke Yakoma Mboti Yokadouma Boyabu Nola Batalimo 130,200 Libenge 62,580 IDPs Mboy in Bangui SANGHA- Enyelle 22,214 MBAÉRÉ Betou Creation date: 26 Sep 2014 Batanga Sources: UNCS, SIGCAF, UNHCR 9,664 Feedback: [email protected] Impfondo Filename: caf_reference_131216 DEMOCRATIC REPUBLIC The boundaries and names shown and the OF THE CONGO designations used on this map do not imply GABON official endorsement or acceptance by the United CONGO Nations. Final boundary between the Republic of Sudan and the Republic of South Sudan has not yet been determined. -
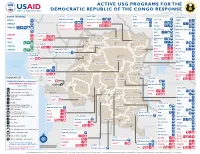
ACTIVE USG PROGRAMS for the DEMOCRATIC REPUBLIC of the CONGO RESPONSE Last Updated 07/27/20
ACTIVE USG PROGRAMS FOR THE DEMOCRATIC REPUBLIC OF THE CONGO RESPONSE Last Updated 07/27/20 BAS-UELE HAUT-UELE ITURI S O U T H S U D A N COUNTRYWIDE NORTH KIVU OCHA IMA World Health Samaritan’s Purse AIRD Internews CARE C.A.R. Samaritan’s Purse Samaritan’s Purse IMA World Health IOM UNHAS CAMEROON DCA ACTED WFP INSO Medair FHI 360 UNICEF Samaritan’s Purse Mercy Corps IMA World Health NRC NORD-UBANGI IMC UNICEF Gbadolite Oxfam ACTED INSO NORD-UBANGI Samaritan’s WFP WFP Gemena BAS-UELE Internews HAUT-UELE Purse ICRC Buta SCF IOM SUD-UBANGI SUD-UBANGI UNHAS MONGALA Isiro Tearfund IRC WFP Lisala ACF Medair UNHCR MONGALA ITURI U Bunia Mercy Corps Mercy Corps IMA World Health G A EQUATEUR Samaritan’s NRC EQUATEUR Kisangani N Purse WFP D WFPaa Oxfam Boende A REPUBLIC OF Mbandaka TSHOPO Samaritan’s ATLANTIC NORTH GABON THE CONGO TSHUAPA Purse TSHOPO KIVU Lake OCEAN Tearfund IMA World Health Goma Victoria Inongo WHH Samaritan’s Purse RWANDA Mercy Corps BURUNDI Samaritan’s Purse MAI-NDOMBE Kindu Bukavu Samaritan’s Purse PROGRAM KEY KINSHASA SOUTH MANIEMA SANKURU MANIEMA KIVU WFP USAID/BHA Non-Food Assistance* WFP ACTED USAID/BHA Food Assistance** SA ! A IMA World Health TA N Z A N I A Kinshasa SH State/PRM KIN KASAÏ Lusambo KWILU Oxfam Kenge TANGANYIKA Agriculture and Food Security KONGO CENTRAL Kananga ACTED CRS Cash Transfers For Food Matadi LOMAMI Kalemie KASAÏ- Kabinda WFP Concern Economic Recovery and Market Tshikapa ORIENTAL Systems KWANGO Mbuji T IMA World Health KWANGO Mayi TANGANYIKA a KASAÏ- n Food Vouchers g WFP a n IMC CENTRAL y i k -

Appraisal Report Kankan-Kouremale-Bamako Road Multinational Guinea-Mali
AFRICAN DEVELOPMENT FUND ZZZ/PTTR/2000/01 Language: English Original: French APPRAISAL REPORT KANKAN-KOUREMALE-BAMAKO ROAD MULTINATIONAL GUINEA-MALI COUNTRY DEPARTMENT OCDW WEST REGION JANUARY 1999 SCCD : N.G. TABLE OF CONTENTS Page PROJECT INFORMATION BRIEF, EQUIVALENTS, ACRONYMS AND ABBREVIATIONS, LIST OF ANNEXES AND TABLES, BASIC DATA, PROJECT LOGICAL FRAMEWORK, ANALYTICAL SUMMARY i-ix 1 INTRODUCTION.............................................................................................................. 1 1.1 Project Genesis and Background.................................................................................... 1 1.2 Performance of Similar Projects..................................................................................... 2 2 THE TRANSPORT SECTOR ........................................................................................... 3 2.1 The Transport Sector in the Two Countries ................................................................... 3 2.2 Transport Policy, Planning and Coordination ................................................................ 4 2.3 Transport Sector Constraints.......................................................................................... 4 3 THE ROAD SUB-SECTOR .............................................................................................. 5 3.1 The Road Network ......................................................................................................... 5 3.2 The Automobile Fleet and Traffic................................................................................. -
From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of the Congo (DRC) from Resource War to ‘Violent Peace’
paper 50 From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of the Congo (DRC) From Resource War to ‘Violent Peace’ Transition in the Democratic Republic of Congo (DRC) by Björn Aust and Willem Jaspers Published by ©BICC, Bonn 2006 Bonn International Center for Conversion Director: Peter J. Croll An der Elisabethkirche 25 D-53113 Bonn Germany Phone: +49-228-911960 Fax: +49-228-241215 E-mail: [email protected] Internet: www.bicc.de Cover Photo: Willem Jaspers From Resource War to ‘Violent Peace’ Table of contents Summary 4 List of Acronyms 6 Introduction 8 War and war economy in the DRC (1998–2002) 10 Post-war economy and transition in the DRC 12 Aim and structure of the paper 14 1. The Congolese peace process 16 1.1 Power shifts and developments leading to the peace agreement 17 Prologue: Africa’s ‘First World War’ and its war economy 18 Power shifts and the spoils of (formal) peace 24 1.2 Political transition: Structural challenges and spoiler problems 29 Humanitarian Situation and International Assistance 30 ‘Spoiler problems’ and political stalemate in the TNG 34 Systemic Corruption and its Impact on Transition 40 1.3 ‘Violent peace’ and security-related liabilities to transition 56 MONUC and its contribution to peace in the DRC 57 Security-related developments in different parts of the DRC since 2002 60 1.4 Fragility of security sector reform 70 Power struggles between institutions and parallel command structures 76 2. A Tale of two cities: Goma and Bukavu as case studies of the transition in North and South Kivu -

21738 Nov. 26—Dec. 3, 1966
21738 KEESING'S CONTEMPORARY ARCHIVES Nov. 26—Dec. 3, 1966 (c) Mr. M. C. Chagla (Education) was appointed External B. ORGANIZATION OF AFRICAN UNITY.—Fourth Affairs Minister ; and (d) Mr. Fakhruddin Ahmed became Assembly of Heads of State and Government. - Dispute Education Minister. between Ghana and Guinea. Mr. Chavan (53) was Chief Minister of Bombay in 1956-60 and The fourth Assembly of the Heads of State and Government Chief Minister of Maharashtra in 1960-62, and succeeded Mr. of the member-States of the Organization of African Unity Krishna Menon as Defence Minister in November 1962, during the (O.A.U.) took place in Addis Ababa on Nov. 5-9. It was border oonfliot with China. Sardar Swaran Singh (69) entered the preceded by a meeting of the Council of Ministers of the Cabinet in 1952, and held a succession of Ministries before becoming External Affairs Minister in 1964. Mr. Chagla (66), a former Chief O.A.U., but this meeting, as well as the Assembly itself, was Justice of the Bombay High Court, was Ambassador in Washington largely overshadowed by a dispute caused by the Government in 1958-62 and High Commissioner in London in 1962-63, and of Ghana in intercepting and detaining the Guinean mission entered the Cabinet as Education Minister in 1963. He is the first to the O.A.U. Moslem to hold the post Of External Affairs Minister. The Ghana-Guinea Dispute. While the Indian press strongly criticized Mrs. Gandhi for her alleged vacillation over the Cabinet changes, the Prime On Oct. 29 the Ghanaian authorities removed from a Pan Minister herself deprecated Mr. -

Global Suicide Rates and Climatic Temperature
SocArXiv Preprint: May 25, 2020 Global Suicide Rates and Climatic Temperature Yusuke Arima1* [email protected] Hideki Kikumoto2 [email protected] ABSTRACT Global suicide rates vary by country1, yet the cause of this variability has not yet been explained satisfactorily2,3. In this study, we analyzed averaged suicide rates4 and annual mean temperature in the early 21st century for 183 countries worldwide, and our results suggest that suicide rates vary with climatic temperature. The lowest suicide rates were found for countries with annual mean temperatures of approximately 20 °C. The correlation suicide rate and temperature is much stronger at lower temperatures than at higher temperatures. In the countries with higher temperature, high suicide rates appear with its temperature over about 25 °C. We also investigated the variation in suicide rates with climate based on the Köppen–Geiger climate classification5, and found suicide rates to be low in countries in dry zones regardless of annual mean temperature. Moreover, there were distinct trends in the suicide rates in island countries. Considering these complicating factors, a clear relationship between suicide rates and temperature is evident, for both hot and cold climate zones, in our dataset. Finally, low suicide rates are typically found in countries with annual mean temperatures within the established human thermal comfort range. This suggests that climatic temperature may affect suicide rates globally by effecting either hot or cold thermal stress on the human body. KEYWORDS Suicide rate, Climatic temperature, Human thermal comfort, Köppen–Geiger climate classification Affiliation: 1 Department of Architecture, Polytechnic University of Japan, Tokyo, Japan. -

The Impact of Climate Variability and Conflict on Childhood Diarrhea and Malnutrition in West Africa
City University of New York (CUNY) CUNY Academic Works All Dissertations, Theses, and Capstone Projects Dissertations, Theses, and Capstone Projects 2-2016 The Impact of Climate Variability and Conflict on Childhood Diarrhea and Malnutrition in West Africa Gillian Dunn Graduate Center, City University of New York How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/gc_etds/765 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] The Impact of Climate Variability and Conflict on Childhood Diarrhea and Malnutrition in West Africa by Gillian Dunn A dissertation submitted to the Graduate Faculty in Public Health in partial fulfillment of the requirements for the degree of Doctor of Public Health, The City University of New York 2016 © 2016 Gillian Dunn All Rights Reserved ii The Impact of Climate Variability and Conflict on Childhood Diarrhea and Malnutrition in West Africa by Gillian Dunn This manuscript has been read and accepted for the Graduate Faculty in Public Health to satisfy the dissertation requirement for the degree of Doctor of Public Health Deborah Balk, PhD Sponsor of Examining Committee Date Signature Denis Nash, PhD Executive Officer, Public Health Date Signature Examining Committee: Glen Johnson, PhD Grace Sembajwe, ScD Emmanuel d’Harcourt, MD THE CITY UNIVERSITY OF NEW YORK iii Dissertation Abstract Title: The Impact of Climate Variability and Conflict on Childhood Diarrhea and Malnutrition in West Africa Author: Gillian Dunn Sponsor: Deborah Balk Objectives: This dissertation aims to contribute to our understanding of how climate variability and armed conflict impacts diarrheal disease and malnutrition among young children in West Africa. -
Competition Rules and Regulations
Competition Rules and Regulations as at 1 January 2017 4 COMPETITION RULES - 01 GENERAL ASPECTS COMPETITION UIPM COMPETITION RULES AND REGULATIONS as at 1 January 2017 table of CONTENTS COMPETITION RULES 01MP - General Aspects Pg. 6 02MP - Fencing Pg. 30 03MP - Swimming Pg. 52 04MP - Riding Pg. 62 05MP - Laser-Run Pg. 80 06UIPM - Biathle Pg. 108 07UIPM - Triathle Pg. 116 EQUIPMENT REGULATIONS 01MP - General Aspects Pg. 123 02MP - Fencing Pg. 124 03MP - Swimming Pg. 138 04MP - Riding Pg. 140 05MP - Laser-Run Pg. 144 6 COMPETITION RULES - 01 GENERAL ASPECTS COMPETITION 01 GENERAL ASPECTS ABBREVIATIONS BAD Business Affairs Delegate NF National Federation CCh Continental Championships NTO National Technical Observer CISM Conseil Internationale du OG Olympic Games Sport Militaire PWR Pentathlon World Ranking EB Executive Board TC Technical Committee FOP Field of Play TD Technical Delegate HQ Headquarters TM Technical Meeting IJ International Judges UIPM Union Internationale de IOC International Olympic Pentathlon Moderne Committee WCC World Cup Competition LOC Local Organising Committee WCF World Cup Final Mins minutes WCh World Championships MD Medical Delegate YOG Youth Olympic Games MP Modern Pentathlon UIPM COMPETITION RULES AND REGULATIONS as at 1 January 2017 7 PART A MODERN PENTATHLON - CONTENTS COMPETITION RULES - 01 GENERAL ASPECTS COMPETITION 1.1 SPHERE OF APPLICATION 1.2 1 Age Groups 2 Calculating age AGE GROUPS 1.3 1 The Five Disciplines 2 Disciplines in Youth Competitions THE EVENTS 1.4 1 The Official UIPM Competitions in 3 OG -

Central African Rep.: Sub-Prefectures 09 Jun 2015
Central African Rep.: Sub-Prefectures 09 Jun 2015 NIGERIA Maroua SUDAN Birao Birao Abyei REP. OF Garoua CHAD Ouanda-Djallé Ouanda-Djalle Ndélé Ndele Ouadda Ouadda Kabo Bamingui SOUTH Markounda Kabo Ngaounday Bamingui SUDAN Markounda CAMEROON Djakon Mbodo Dompta Batangafo Yalinga Goundjel Ndip Ngaoundaye Boguila Batangafo Belel Yamba Paoua Nangha Kaga-Bandoro Digou Bocaranga Nana-Bakassa Borgop Yarmbang Boguila Mbrès Nyambaka Adamou Djohong Ouro-Adde Koui Nana-Bakassa Kaga-Bandoro Dakere Babongo Ngaoui Koui Mboula Mbarang Fada Djohong Garga Pela Bocaranga MbrÞs Bria Djéma Ngam Bigoro Garga Bria Meiganga Alhamdou Bouca Bakala Ippy Yalinga Simi Libona Ngazi Meidougou Bagodo Bozoum Dekoa Goro Ippy Dir Kounde Gadi Lokoti Bozoum Bouca Gbatoua Gbatoua Bakala Foulbe Dékoa Godole Mala Mbale Bossangoa Djema Bindiba Dang Mbonga Bouar Gado Bossemtélé Rafai Patou Garoua-BoulaiBadzere Baboua Bouar Mborguene Baoro Sibut Grimari Bambari Bakouma Yokosire Baboua Bossemptele Sibut Grimari Betare Mombal Bogangolo Bambari Ndokayo Nandoungue Yaloké Bakouma Oya Zémio Sodenou Zembe Baoro Bogangolo Obo Bambouti Ndanga Abba Yaloke Obo Borongo Bossembele Ndjoukou Bambouti Woumbou Mingala Gandima Garga Abba Bossembélé Djoukou Guiwa Sarali Ouli Tocktoyo Mingala Kouango Alindao Yangamo Carnot Damara Kouango Bangassou Rafa´ Zemio Zémio Samba Kette Gadzi Boali Damara Alindao Roma Carnot Boulembe Mboumama Bedobo Amada-Gaza Gadzi Bangassou Adinkol Boubara Amada-Gaza Boganangone Boali Gambo Mandjou Boganangone Kembe Gbakim Gamboula Zangba Gambo Belebina Bombe Kembé Ouango -
South Africa, a Country Notorious Tor Its Complete Oppression. of Africans, Has Been Making a Special Effort to Get Afro-Amat-Tean Entertainers to Visit Them
SHOULD Ar~eRICAN BLACKS TOUR SOUTH AFRICA TO ENTERTAIN AFRICANS? South Africa, a country notorious tor its complete oppression. of Africans, has been making a special effort to get Afro-Amat-tean entertainers to visit them. 1) In M:ay, 1970, Percy Sledge, a Black American singer whose \'\ records are big sellers in Cape Town, broke a twelve-year boycott \ and entertained segregated black and white audiences in South Africa, as reported in the Guardian \'Jeeklyfi June 6, 1970. 2) In October, 1971, Eartha Kitt entertained white South Africans in Swaziland. Newsweek reported in its November 22, 1971 issue that "The black sex kitten from the Carolina cotton fields ••• sat on the knee of a white South Africnn and purred her famous number 'C'est Si Bon' in his ear ••• Next April (1972) Eartha will tour South Africa itself for six weeks ••• " 3} On December 21, 1971, the New~ Times reported that black golfer Lee Elder competed in a golf tournament in South Africa. 4) The i:Jashington .M!:2.-dmerican reported on October 23, 1971. th~t singer Sammy Davis Jr., would entertain South Africans in Swaziland under a ~~210 cover charge. "It is reported that the Sammy Davis Show of at least fourteen artists have been guaranteed a minimum cf ,~·'3 50,000. tt 5) ill on July 29, 1971 stated that ~Ar.titha Franklin was scheduled to entertain Africans in South Africa for a reputed ~45,000 for three weeks. 6) On August 21, 1971, the Amsterdam~ reported that negotiations were under way for Muhammad Ali to give ten lectures in South Africa for a reputed ~300,000.