Better Intrapartum Practices to Reduce Newborn Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Late Preterm and Term Neonates Exposed to Maternal Chorioamnionitis Mitali Sahni1,4* , María E
Sahni et al. BMC Pediatrics (2019) 19:282 https://doi.org/10.1186/s12887-019-1650-0 RESEARCH ARTICLE Open Access Management of Late Preterm and Term Neonates exposed to maternal Chorioamnionitis Mitali Sahni1,4* , María E. Franco-Fuenmayor2 and Karen Shattuck3 Abstract Background: Chorioamnionitis is a significant risk factor for early-onset neonatal sepsis. However, empiric antibiotic treatment is unnecessary for most asymptomatic newborns exposed to maternal chorioamnionitis (MC). The purpose of this study is to report the outcomes of asymptomatic neonates ≥35 weeks gestational age (GA) exposed to MC, who were managed without routine antibiotic administration and were clinically monitored while following complete blood cell counts (CBCs). Methods: A retrospective chart review was performed on neonates with GA ≥ 35 weeks with MC during calendar year 2013. IT ratio (immature: total neutrophils) was considered suspicious if ≥0.3. The data were analyzed using independent sample T-tests. Results: Among the 275 neonates with MC, 36 received antibiotics for possible sepsis. Twenty-one were treated with antibiotics for > 48 h for clinical signs of infection; only one infant had a positive blood culture. All 21 became symptomatic prior to initiating antibiotics. Six showed worsening of IT ratio. Thus empiric antibiotic administration was safely avoided in 87% of neonates with MC. 81.5% of the neonates had follow-up appointments within a few days and at two weeks of age within the hospital system. There were no readmissions for suspected sepsis. Conclusions: In our patient population, using CBC indices and clinical observation to predict sepsis in neonates with MC appears safe and avoids the unnecessary use of antibiotics. -

Antenatal Corticosteroid Use and Clinical Evolution of Preterm Newborn Infants
0021-7557/04/80-04/277 Jornal de Pediatria Copyright © 2004 by Sociedade Brasileira de Pediatria ARTIGO ORIGINAL Uso antenatal de corticosteróide e evolução clínica de recém-nascidos pré-termo Antenatal corticosteroid use and clinical evolution of preterm newborn infants Rede Brasileira de Pesquisas Neonatais* Resumo Abstract Objetivo: Descrever a freqüência de utilização de corticosteróide Objectives: To describe the use of antenatal corticosteroid and antenatal e a evolução clínica dos recém-nascidos pré-termo. clinical evolution of preterm babies. Métodos: Estudo observacional prospectivo tipo coorte de todos Methods: An observational prospective cohort study was carried os neonatos com idade gestacional entre 23 e 34 semanas nascidos na out. All 463 pregnant women and their 514 newborn babies with Rede Brasileira de Pesquisas Neonatais entre agosto e dezembro de gestational age ranging from 23 to 34 weeks, born at the Brazilian 2001. Os prontuários médicos foram revistos, as mães entrevistadas e Neonatal Research Network units, were evaluated from August 1 to os pré-termos acompanhados. A análise dos dados foi realizada com o December 31, 2001. The data were obtained through maternal interview, teste do qui-quadrado, t de Student, Mann-Whitney, ANOVA e regres- analysis of medical records, and follow-up of the newborn infants. Data são logística múltipla, com nível de significância de 5%. analysis was performed with the use of chi-square, t Student, Mann- Resultados: Avaliaram-se 463 gestantes e seus 514 recém- Whitney, and ANOVA tests and multiple logistic regression, with level nascidos. As gestantes tratadas tiveram mais gestações prévias, of significance set at 5%. consultas de pré-natal, hipertensão arterial e maior uso de tocolíticos. -

Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H
Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H. Long, MD, PhD,a,b Jennifer G. Fiore, MD,a,b Riaz Gillani, MD,a,b Laurie M. Douglass, MD,c Alan M. Fujii, MD,d Jodi D. Hoffman, MDe A 2-day old term male infant was found to be hypotonic and minimally abstract reactive during routine nursing care in the newborn nursery. At 40 hours of life, he was hypoglycemic and had intermittent desaturations to 70%. His mother had an unremarkable pregnancy and spontaneous vaginal delivery. The mother’s prenatal serology results were negative for infectious risk factors. Apgar scores were 9 at 1 and 5 minutes of life. On day 1 of life, he fed, stooled, and voided well. Our expert panel discusses the differential diagnosis of hypotonia in a neonate, offers diagnostic and management recommendations, and discusses the final diagnosis. DRS LONG, FIORE, AND GILLANI, birth weight was 3.4 kg (56th PEDIATRIC RESIDENTS percentile), length was 52 cm (87th aDepartment of Medicine, Boston Children’s Hospital, d e percentile), and head circumference Boston, Massachusetts; and Neonatology Section, Medical A 2-day old male infant born at Genetics Section, cDivision of Child Neurology, and 38 weeks and 4 days was found to be was 33 cm (12th percentile). His bDepartment of Pediatrics, Boston Medical Center, Boston, limp and minimally reactive during physical examination at birth was Massachusetts routine care in the newborn nursery. normal for gestational age, with Drs Long, Fiore, and Gillani conceptualized, drafted, Just 5 hours before, he had an appropriate neurologic, cardiac, and and edited the manuscript; Drs Douglass, Fujii, and appropriate neurologic status when respiratory components. -

Early-Onset Neonatal Sepsis: a Continuing Problem in Need of Novel Prevention Strategies Barbara J
Early-Onset Neonatal Sepsis: A Continuing Problem in Need of Novel Prevention Strategies Barbara J. Stoll, MD Early-onset neonatal sepsis (EOS) colonized women or targeted IAP for remains a feared cause of severe women with obstetrical risk factors illness and death among infants of all in labor known to increase GBS birthweights and gestational ages, transmission. 5 Revised guidelines with particular impact among preterm in 2002 recommended universal infants. Centers for Disease Control and antenatal screening for GBS at 35 to Prevention investigators have studied 37 weeks’ gestational age to identify the changing epidemiology of invasive colonized women who should receive EOS for several decades. The Active IAP. 6 Guidelines were additionally Bacterial Core surveillance (ABCs) refined in 2010 to provide neonatal network, a collaboration between management recommendations based the Centers for Disease Control and on maternal risk factors and clinical H. Wayne Hightower Distinguished Professor in the Medical Prevention, state health departments, condition of the infant at birth, with Sciences and Dean, McGovern Medical School, University of and universities, was established in an attempt to reduce unnecessary Texas Health Science Center at Houston, Houston, Texas 1995 to address emerging infectious evaluations of well-appearing infants Opinions expressed in these commentaries are diseases of public health importance, without risk factors. 7 Widespread those of the author and not necessarily those of the including infections due to major adherence to national guidelines American Academy of Pediatrics or its Committees. neonatal pathogens. 1, 2 ABCs data resulted in a remarkable decline DOI: 10.1542/peds.2016-3038 are remarkable because of the in early onset GBS disease, but a Accepted for publication Sep 12, 2016 geographic distribution and size of the concomitant increase in exposure Address correspondence to Barbara J. -

Neonatal Sepsis Expanded Tracking Form Instructions
2014 ABCs Neonatal Infection Expanded Tracking Form Instruction Sheet Updated 12/19/2013 This form should be completed for all cases of early- and late-onset group B Streptococcus disease (GBS). Early-onset is defined as GBS disease onset at 0-6 days of age [(culture date-birth date) <7 days]. Late-onset is defined as GBS disease at 7-89 days of age [6 days < (culture date-birth date) <90 days]. This case report form for GBS disease can be completed on infants born at home, but not for stillbirths. Additionally, this form should be filled out for all neonatal sepsis cases, which includes both GBS and non-GBS cases. Neonatal sepsis is defined as invasive bacterial disease onset at 0-2 days of age [(culture date-birth date) <3 days]. Case report forms for neonatal sepsis cases should not be completed on infants born at home or stillbirths. For those sites participating in neonatal sepsis surveillance, please refer to the Neonatal Sepsis protocol for clarification on the inclusion and exclusion criteria. The following is an algorithm of which forms should be filled out for early- & late-onset GBS cases meeting the ABCs case definition: FORMS NNS Surveillance Form Neonatal Infection ABCs Case Report Form SCENARIO Expanded Tracking Form* Early-onset (& Neonatal √ √ √ Sepsis)† Late-onset √ √ *The Neonatal Infection Expanded Tracking Form is the expanded form that combines the Neonatal Sepsis Maternal Case Report Form and the Neonatal group B Streptococcus Disease Prevention Tracking Form. † For CA, CT, GA, and MN, please refer to the Neonatal -

Neonatal Pneumonia
Chapter 2 Neonatal Pneumonia Friedrich Reiterer Additional information is available at the end of the chapter http://dx.doi.org/10.5772/54310 1. Introduction Neonatal pneumonia is a serious respiratory infectious disease caused by a variety of microorganisms, mainly bacteria, with the potential of high mortality and morbidity (1,2). Worldwide neonatal pneumonia is estimated to account for up to 10% of childhood mortality, with the highest case fatality rates reported in developing countries (3,4). It´s impact may be increased in the case of early onset, prematurity or an underlying pulmonary condition like RDS, meconium aspiration or CLD/bronchopulmonary dysplasia (BPD), when the pulmonary capacity is already limited. Ureaplasma pneumonia and ventilator- associated pneumonia (VAP) have also been associated with the development of BPD and poor pulmonary outcome (5,6,7). In this chapter we will review different aspects of neonatal pneumonia and will present case reports from our level III neonatal unit in Graz. 2. Epidemiology Reported frequencies of neonatal pneumonia range from 1 to 35 %, the most commonly quoted figures being 1 percent for term infants and 10 percent for preterm infants (8). The incidence varies according to gestational age, intubation status, diagnostic criteria or case definition, the level and standard of neonatal care, race and socioeconomic status. In a retrospective analysis of a cohort of almost 6000 neonates admitted to our NICU pneumonia was diagnosed in all gestational age classes. The incidence of bacterial pneumonia including Ureaplasma urealyticum (Uu) pneumonia was 1,4 % with a median patient gestational age of 35 weeks (range 23-42 weeks) and a mortality of 2,5%. -

Autopsy Case Report and Review of the Literature Karyna C
Fatal Neonatal Echovirus 6 Infection: Autopsy Case Report and Review of the Literature Karyna C. Ventura, M.D., Hal Hawkins, M.D., Ph.D., Michael B. Smith, M.D., David H. Walker, M.D. Department of Pathology, University of Texas Medical Branch, Galveston, Texas CASE REPORT A full-term, healthy male neonate was delivered by caesarian section to a 26-year-old primigravida A full-term boy appropriate for his gestational age woman who had a history of fever and upper respi- was born via caesarian section to a 26-year-old G1P0 ratory tract infection. On the fourth day of life, the Latin American woman who had a medical history of a well-controlled seizure disorder for which she was neonate developed a sepsis-like syndrome, acute receiving carbamazepine. She had received regular respiratory and renal failure, and disseminated in- prenatal care, with negative prenatal serologic tests travascular coagulopathy. He died 13 days after for human immunodeficiency virus, hepatitis B virus, birth. Postmortem examination revealed jaundice, and syphilis. Two weeks before delivery, she experi- anasarca, massive hepatic necrosis, adrenal hemor- enced fever and an upper respiratory tract infection. rhagic necrosis, renal medullary hemorrhage, hem- At birth, the infant weighed 3838 g and had an Apgar orrhagic noninflammatory pneumonia, and severe score of 9. The neonate was put under an oxygen encephalomalacia. Echovirus type 6 was isolated hood, then was later slowly weaned from it. On his from blood, liver, and lungs. Although uncommon, fourth day of life, the neonate developed fever echovirus type 6 infection may produce a spectrum (38.6°C) and was observed to have decreased activity. -

The Effects of Maternal Chorioamnionitis on the Neonate
Neonatal Nursing Education Brief: The Effects of Maternal Chorioamnionitis on the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Maternal chorioamnionitis is a common condition that can have negative effects on the neonate. The use of broad spectrum antibiotics in labor can reduce the risks, but infants exposed to chorioamnionitis continue to require treatment. The neonatal sepsis risk calculator can guide treatment. NICU, chorioamnionitis, early onset neonatal sepsis, sepsis risk calculator The Effects of Maternal Chorioamnionitis on the Neonate Purpose and Goal: CNEP # 2090 • Understand the effects of chorioamnionitis on the neonate. • Learn about a new approach for treating infants at risk. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the pathogenesis of maternal chorioamnionitis. • Describe the outcomes for neonates exposed to chorioamnionitis. • Identify 2 approaches for the treatment of early onset sepsis. Introduction • Chorioamnionitis is a common complication • It affects up to 10% of all pregnancies • It is an infection of the amniotic fluid and placenta • It is characterized by inflammation -

Bacterial Infection in the Fetus and Newborn
Arch Dis Child: first published as 10.1136/adc.46.245.1 on 1 February 1971. Downloaded from Review Article Archives of Disease in Childhood, 1971, 46, 1. Bacterial Infection in the Fetus and Newborn PAMELA A. DAVIES From the Neonatal Research Unit, Hammersmith Hospital, London The significance of potentially harmful influences years is illustrated by the fact that a request for a on the fetus and newborn may be judged in two Medlars search of the literature from 1963 to the ways. A direct effect on perinatal mortality is the middle of 1969 resulted in the retrieval of 17,147 more easily measured; while subtle damage at a relevant items. The computer rebelled at the size period of very rapid growth may have lasting effects, of this 'print-out' so relieving the writer of a 'read- not always immediately obvious, on the ultimate out' which would have extended into senescence. size and function of organs in survivors. Bacterial Those interested will therefore be deprived of a infection continues to exert an influence in both complete coverage ofthe problem, and subjected to a ways in the perinatal period, for the impact of personal and language bias. Much reliance has antibiotic and chemotherapeutic drugs has been been placed on previous review articles, so that less dramatic than at other ages, and humoral and often, and most regrettably, earlier original work copyright. cellular defence mechanisms may differ qualitatively goes unacknowledged. and quantitatively. It is difficult to assess the true extent of this The Defence Mechanisms of the Host problem from the recent literature, largely because The inflammatory response. -
Neonatal Sepsis Management Guidelines (PDF)
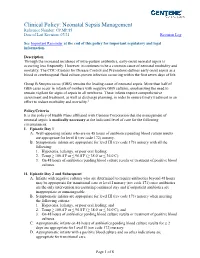
Clinical Policy: Neonatal Sepsis Management Reference Number: CP.MP.85 Date of Last Revision: 07/21 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Through the increased incidence of intra-partum antibiotics, early-onset neonatal sepsis is occurring less frequently. However, it continues to be a common cause of neonatal morbidity and mortality. The CDC (Centers for Disease Control and Prevention) defines early onset sepsis as a blood or cerebrospinal fluid culture-proven infection occurring within the first seven days of life. Group B Streptococcus (GBS) remains the leading cause of neonatal sepsis. More than half of GBS cases occur in infants of mothers with negative GBS cultures, emphasizing the need to remain vigilant for signs of sepsis in all newborns. These infants require comprehensive assessment and treatment, as well as discharge planning, in order to ensure timely treatment in an effort to reduce morbidity and mortality.2 Policy/Criteria It is the policy of Health Plans affiliated with Centene Corporation that the management of neonatal sepsis is medically necessary at the indicated level of care for the following circumstances: I. Episode Day 1 A. Well-appearing infants who are on 48 hours of antibiotics pending blood culture results are appropriate for level II (rev code 172) nursery. B. Symptomatic infants are appropriate for level III (rev code 173) nursery with all the following: 1. Hypotonia, lethargy, or poor oral feeding; 2. Temp ≥ 100.4◦F or ≤ 96.8◦F (≥ 38.0◦ or ≤ 36.0◦C); 3. On 48 hours of antibiotics pending blood culture results or treatment of positive blood cultures. -

Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update
Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update Aline Fuchsa, Julia Bielickia,b, Shrey Mathurb, Mike Sharlandb, Johannes N. Van Den Ankera,c a Paediatric Pharmacology and Pharmacometrics, University Children's Hospital Basel, Basel, Switzerland b Paediatric Infectious Disease Research Group, Institute for Infection and Immunity, St George's University of London, London, United Kingdom c Division of Clinical Pharmacology, Children’s National Health System, Washington, DC, USA WHO-Reviews 1 TABLE OF CONTENTS 1. INTRODUCTION ............................................................................................................................... 3 1.1. Aims ......................................................................................................................................... 3 1.2. Background ............................................................................................................................. 3 1.2.1. Definition and diagnosis ................................................................................................. 3 Neonatal Sepsis ............................................................................................................................... 3 Paediatric Sepsis ............................................................................................................................. 4 Community versus hospital acquired sepsis .................................................................................. 5 1.2.2. Microbiology .................................................................................................................. -

The Epidemiology, Risk Factors, Mortality Rate, Diagnosis, Etiologies and Treatment of Neonatal Respiratory Distress: a Scoping Review
The epidemiology, risk factors, mortality rate, diagnosis, etiologies and treatment of neonatal respiratory distress: a scoping review Joel Noutakdie Tochie ( [email protected] ) Human Research Education and Network (HREN), Yaoundé, Cameroon Aurelie T. Sibetcheu Université de Yaoundé I Celestin Danwang Université Catholique de Louvain Aime Noula Mbonda Central Africa Clustered Cross International Igor Kamla Université de Yaoundé I Gregory Ayissi Université de Yaoundé I Jan René Nkeck Université de Yaoundé I Dany Hermann Ngwanou University of Bamenda Mazou Ngou Temgoua Université de Yaoundé I Research Article Keywords: neonate, respiratory distress, prevalence, risk factors, etiologies, diagnosis, management, scoping review Posted Date: December 30th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-131366/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/22 Abstract Background: Quite a tricky day-to-day clinical condition which may present as the rst alarming sign of a life-threatening pathology, neonatal respiratory distress (NRD) remains an emergency until its etiology is diagnosed and appropriate treated delivered to the neonate. While the prevalence, risk factors, etiologies, diagnosis and management of this potentially fatal neonatal condition has not been examined extensively, the objective of this scoping review is to synthesise contemporary studies on the prevalence, risk factors, etiologies, diagnosis and management of NRD. Methods: We searched MEDLINE and Google Scholar up to November 13, 2020 for observational and experimental studies and systematic reviews addressing NRD without language restriction. Eight investigators working in four pairs independently selected and extracted relevant data. The methodological quality of all included studies was assessed.