American Nephrology Nurses Association
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pennsylvania Delegation Letter to Congressional Leadership on LIHTC
April 20, 2020 The Honorable Nancy Pelosi The Honorable Mitch McConnell Speaker of the House Majority Leader United States House of Representatives United States Senate Washington DC 20515 Washington DC 20510 The Honorable Kevin McCarthy The Honorable Charles Schumer Minority Leader Minority Leader United States House of Representatives United States Senate Washington DC 20515 Washington DC 20510 Dear Speaker Pelosi, Leader McConnell, Leader McCarthy, and Leader Schumer: As you consider additional legislative priorities related to COVID-19, we respectfully urge you to support critical improvements to the Low-Income Housing Tax Credit (LIHTC) Program. The LIHTC program, administered jointly by the Internal Revenue Service (IRS) and state tax credit allocating agencies, provides federal tax credits to developers in exchange for their investment in developing and preserving affordable rental housing. The Pennsylvania Housing Finance Agency, for instance, monitors more than 1,100 affordable housing communities receiving LIHTC. Across the country, LIHTC has led to the development and preservation of over 3 million affordable rental units. As American families struggle to cover health care, utilities, and food costs during this health and economic crisis, access to safe, permanent housing is critical to prevent homelessness and poverty. Targeted public-private investments help provide desperately needed affordable housing for low-income families. As you weigh additional federal assistance measures to address COVID-19, we strongly encourage you to include the following LIHTC changes: Enact a minimum 4% credit rate used to finance acquisitions and Housing Bond- financed developments. LIHTC rates fluctuate in response to market interest movements. Tied to declining federal borrowing rates, the value of the 4% credit rate is closer to 3% – the lowest it has ever been. -

Congressional Report Card
Congressional Report Card NOTE FROM BRIAN DIXON Senior Vice President for Media POPULATION CONNECTION and Government Relations ACTION FUND 2120 L St NW, Suite 500 Washington, DC 20037 ou’ll notice that this year’s (202) 332–2200 Y Congressional Report Card (800) 767–1956 has a new format. We’ve grouped [email protected] legislators together based on their popconnectaction.org scores. In recent years, it became twitter.com/popconnect apparent that nearly everyone in facebook.com/popconnectaction Congress had either a 100 percent instagram.com/popconnectaction record, or a zero. That’s what you’ll popconnectaction.org/116thCongress see here, with a tiny number of U.S. Capitol switchboard: (202) 224-3121 exceptions in each house. Calling this number will allow you to We’ve also included information connect directly to the offices of your about some of the candidates senators and representative. that we’ve endorsed in this COVER CARTOON year’s election. It’s a small sample of the truly impressive people we’re Nick Anderson editorial cartoon used with supporting. You can find the entire list at popconnectaction.org/2020- the permission of Nick Anderson, the endorsements. Washington Post Writers Group, and the Cartoonist Group. All rights reserved. One of the candidates you’ll read about is Joe Biden, whom we endorsed prior to his naming Sen. Kamala Harris his running mate. They say that BOARD OF DIRECTORS the first important decision a president makes is choosing a vice president, Donna Crane (Secretary) and in his choice of Sen. Harris, Joe Biden struck gold. Carol Ann Kell (Treasurer) Robert K. -
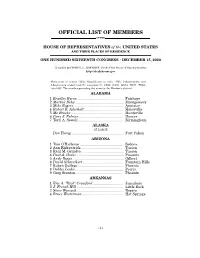
Official List of Members
OFFICIAL LIST OF MEMBERS OF THE HOUSE OF REPRESENTATIVES of the UNITED STATES AND THEIR PLACES OF RESIDENCE ONE HUNDRED SIXTEENTH CONGRESS • DECEMBER 15, 2020 Compiled by CHERYL L. JOHNSON, Clerk of the House of Representatives http://clerk.house.gov Democrats in roman (233); Republicans in italic (195); Independents and Libertarians underlined (2); vacancies (5) CA08, CA50, GA14, NC11, TX04; total 435. The number preceding the name is the Member's district. ALABAMA 1 Bradley Byrne .............................................. Fairhope 2 Martha Roby ................................................ Montgomery 3 Mike Rogers ................................................. Anniston 4 Robert B. Aderholt ....................................... Haleyville 5 Mo Brooks .................................................... Huntsville 6 Gary J. Palmer ............................................ Hoover 7 Terri A. Sewell ............................................. Birmingham ALASKA AT LARGE Don Young .................................................... Fort Yukon ARIZONA 1 Tom O'Halleran ........................................... Sedona 2 Ann Kirkpatrick .......................................... Tucson 3 Raúl M. Grijalva .......................................... Tucson 4 Paul A. Gosar ............................................... Prescott 5 Andy Biggs ................................................... Gilbert 6 David Schweikert ........................................ Fountain Hills 7 Ruben Gallego ............................................ -

November 7, 2018 Pennsylvania Was One of the Most Closely Watched
Keep up to date with our blog: Follow us on Twitter @BuchananGov knowingGovernmentRelations.com November 7, 2018 Pennsylvania was one of the most closely watched states in the country on Election Day. Redistricting of Congressional seats meant a shakeup was coming for the Commonwealth’s 18-member delegation. At the statewide level, the Governor and one of two U.S. Senators were on the ballot. In the state legislature, half of the 50 Senate seats (even- numbered districts) and the entire 203-seat House of Representatives were up for grabs. During the 2017-18 legislative session the Pennsylvania House of Representatives was comprised of 121 Republicans and 82 Democrats. After last night’s election, the 2018-19 legislative session will have 109 Republicans and 94 Democrats, after the Democrats picked up 11 seats. In the Pennsylvania Senate, Republicans had a majority during the 2017-18 by a margin of 34-16. Yesterday, Senate Democrats picked up 5 seats, narrowing the Republican’s majority. Next session will have 29 Republican members and 21 Democratic members. The 18-member Pennsylvania delegation had only 6 Democrats during the 115th Congress (2017-19). When new members are sworn into the 116th Congress next year, Pennsylvania’s delegation will be split, with 9 Republicans and 9 Democrats. Governor Governor Tom Wolf (D) and his running mate for Lieutenant Governor John Fetterman (D) defeated the ticket of Scott Wagner (R) and Jeff Bartos (R). Wolf received 2,799,1559 votes (57.66%), while Wagner got 1,981,027 votes (40.81%). U.S. Senate Senator Bob Casey (D) defeated Lou Barletta (R) by a margin of over half a million votes. -
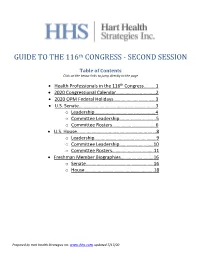
GUIDE to the 116Th CONGRESS
th GUIDE TO THE 116 CONGRESS - SECOND SESSION Table of Contents Click on the below links to jump directly to the page • Health Professionals in the 116th Congress……….1 • 2020 Congressional Calendar.……………………..……2 • 2020 OPM Federal Holidays………………………..……3 • U.S. Senate.……….…….…….…………………………..…...3 o Leadership…...……..…………………….………..4 o Committee Leadership….…..……….………..5 o Committee Rosters……….………………..……6 • U.S. House..……….…….…….…………………………...…...8 o Leadership…...……………………….……………..9 o Committee Leadership……………..….…….10 o Committee Rosters…………..…..……..…….11 • Freshman Member Biographies……….…………..…16 o Senate………………………………..…………..….16 o House……………………………..………..………..18 Prepared by Hart Health Strategies Inc. www.hhs.com, updated 7/17/20 Health Professionals Serving in the 116th Congress The number of healthcare professionals serving in Congress increased for the 116th Congress. Below is a list of Members of Congress and their area of health care. Member of Congress Profession UNITED STATES SENATE Sen. John Barrasso, MD (R-WY) Orthopaedic Surgeon Sen. John Boozman, OD (R-AR) Optometrist Sen. Bill Cassidy, MD (R-LA) Gastroenterologist/Heptalogist Sen. Rand Paul, MD (R-KY) Ophthalmologist HOUSE OF REPRESENTATIVES Rep. Ralph Abraham, MD (R-LA-05)† Family Physician/Veterinarian Rep. Brian Babin, DDS (R-TX-36) Dentist Rep. Karen Bass, PA, MSW (D-CA-37) Nurse/Physician Assistant Rep. Ami Bera, MD (D-CA-07) Internal Medicine Physician Rep. Larry Bucshon, MD (R-IN-08) Cardiothoracic Surgeon Rep. Michael Burgess, MD (R-TX-26) Obstetrician Rep. Buddy Carter, BSPharm (R-GA-01) Pharmacist Rep. Scott DesJarlais, MD (R-TN-04) General Medicine Rep. Neal Dunn, MD (R-FL-02) Urologist Rep. Drew Ferguson, IV, DMD, PC (R-GA-03) Dentist Rep. Paul Gosar, DDS (R-AZ-04) Dentist Rep. -

Russian Bounties on Us Troops: Why Hasn't the Administration Responded?
RUSSIAN BOUNTIES ON U.S. TROOPS: WHY HASN’T THE ADMINISTRATION RESPONDED? HEARING BEFORE THE COMMITTEE ON FOREIGN AFFAIRS HOUSE OF REPRESENTATIVES ONE HUNDRED SIXTEENTH CONGRESS SECOND SESSION JULY 9, 2020 Serial No. 116–119 Printed for the use of the Committee on Foreign Affairs ( Available: http://www.foreignaffairs.house.gov/, http://docs.house.gov, or http://www.govinfo.gov U.S. GOVERNMENT PUBLISHING OFFICE 41–240PDF WASHINGTON : 2020 COMMITTEE ON FOREIGN AFFAIRS ELIOT L. ENGEL, New York, Chairman BRAD SHERMAN, California MICHAEL T. MCCAUL, Texas, Ranking GREGORY W. MEEKS, New York Member ALBIO SIRES, New Jersey CHRISTOPHER H. SMITH, New Jersey GERALD E. CONNOLLY, Virginia STEVE CHABOT, Ohio THEODORE E. DEUTCH, Florida JOE WILSON, South Carolina KAREN BASS, California SCOTT PERRY, Pennsylvania WILLIAM KEATING, Massachusetts TED S. YOHO, Florida DAVID CICILLINE, Rhode Island ADAM KINZINGER, Illinois AMI BERA, California LEE ZELDIN, New York JOAQUIN CASTRO, Texas JIM SENSENBRENNER, Wisconsin DINA TITUS, Nevada ANN WAGNER, Missouri ADRIANO ESPAILLAT, New York BRIAN MAST, Florida TED LIEU, California FRANCIS ROONEY, Florida SUSAN WILD, Pennsylvania BRIAN FITZPATRICK, Pennsylvania DEAN PHILLIPS, Minnesota JOHN CURTIS, Utah ILHAN OMAR, Minnesota KEN BUCK, Colorado COLIN ALLRED, Texas RON WRIGHT, Texas ANDY LEVIN, Michigan GUY RESCHENTHALER, Pennsylvania ABIGAIL SPANBERGER, Virginia TIM BURCHETT, Tennessee CHRISSY HOULAHAN, Pennsylvania GREG PENCE, Indiana TOM MALINOWSKI, New Jersey STEVE WATKINS, Kansas DAVID TRONE, Maryland MIKE GUEST, Mississippi JIM COSTA, California JUAN VARGAS, California VICENTE GONZALEZ, Texas JASON STEINBAUM, Staff Director BRENDAN SHIELDS, Republican Staff Director (II) C O N T E N T S Page WITNESSES Morell, Michael, Former Acting Director and Deputy Director, Central Intel- ligence Agency ..................................................................................................... -

September 18, 2020 the Honorable Alex Azar Secretary U.S
September 18, 2020 The Honorable Alex Azar Secretary U.S. Department of Health and Human Services 200 Independence Avenue, SW Washington, DC 20201 Dear Secretary Azar: We are writing in support of Pennsylvania Governor Wolf’s letter of August 21, 2020, in which he raised concerns over the federal government’s actions to divert necessary COVID-19 testing supplies away from Pennsylvania. These actions—particularly the diversion of supplies and reagents manufactured by Hologic and Roche—have made it harder for hospitals and laboratories in our state to keep up with the demand for COVID-19 tests, thereby jeopardizing the progress Pennsylvania has made in curtailing the spread of this virus. We echo Governor Wolf’s concerns, and request your prompt attention to this matter. Pennsylvania was one of the earlier and harder-hit states in the pandemic. As of writing, the state has seen 148,683 confirmed cases of COVID-19 and 7,934 deaths.1 While the daily reported numbers of new cases and deaths has decreased significantly from their peak in April, hundreds of new COVID-19 cases continue to appear each day. The state’s ongoing containment efforts will be severely hampered if adequate testing is not available. Hospitals across Pennsylvania have reported testing supply diversions or stoppages at the order of the White House, forcing providers who would normally be able to obtain COVID-19 test results within 24 to 48 hours to send specimens to outside laboratories, including Quest and LabCorp. This increases the risk of delays in getting test results to patients, which in turn increases the risk of continued viral transmission in Pennsylvania homes and communities. -

State Delegations
STATE DELEGATIONS Number before names designates Congressional district. Senate Republicans in roman; Senate Democrats in italic; Senate Independents in SMALL CAPS; House Democrats in roman; House Republicans in italic; House Libertarians in SMALL CAPS; Resident Commissioner and Delegates in boldface. ALABAMA SENATORS 3. Mike Rogers Richard C. Shelby 4. Robert B. Aderholt Doug Jones 5. Mo Brooks REPRESENTATIVES 6. Gary J. Palmer [Democrat 1, Republicans 6] 7. Terri A. Sewell 1. Bradley Byrne 2. Martha Roby ALASKA SENATORS REPRESENTATIVE Lisa Murkowski [Republican 1] Dan Sullivan At Large – Don Young ARIZONA SENATORS 3. Rau´l M. Grijalva Kyrsten Sinema 4. Paul A. Gosar Martha McSally 5. Andy Biggs REPRESENTATIVES 6. David Schweikert [Democrats 5, Republicans 4] 7. Ruben Gallego 1. Tom O’Halleran 8. Debbie Lesko 2. Ann Kirkpatrick 9. Greg Stanton ARKANSAS SENATORS REPRESENTATIVES John Boozman [Republicans 4] Tom Cotton 1. Eric A. ‘‘Rick’’ Crawford 2. J. French Hill 3. Steve Womack 4. Bruce Westerman CALIFORNIA SENATORS 1. Doug LaMalfa Dianne Feinstein 2. Jared Huffman Kamala D. Harris 3. John Garamendi 4. Tom McClintock REPRESENTATIVES 5. Mike Thompson [Democrats 45, Republicans 7, 6. Doris O. Matsui Vacant 1] 7. Ami Bera 309 310 Congressional Directory 8. Paul Cook 31. Pete Aguilar 9. Jerry McNerney 32. Grace F. Napolitano 10. Josh Harder 33. Ted Lieu 11. Mark DeSaulnier 34. Jimmy Gomez 12. Nancy Pelosi 35. Norma J. Torres 13. Barbara Lee 36. Raul Ruiz 14. Jackie Speier 37. Karen Bass 15. Eric Swalwell 38. Linda T. Sa´nchez 16. Jim Costa 39. Gilbert Ray Cisneros, Jr. 17. Ro Khanna 40. Lucille Roybal-Allard 18. -

Representative Susan Wild 116Th United States Congress
476 380 80 80 209 80 80 81 Representative Susan Wild 116th United States Congress 209 80 Pennsylvania's 7TH Congressional District The 1 federally-funded health center209 organizations with a presence in Pennsylvania's 7th 209 46 Congressional District leverage476 $2,672,705 in federal investments to serve 5,226 patients. 81 §¨¦ §¨¦ §¨¦ 209 §¨¦ ¤£ 476 §¨¦ §¨¦ §¨¦ 22 78 22 ¤£ 78 22 §¨¦ 78 78 78 222 ¤£ 78 ¤£ §¨¦ ¤£ §¨¦ 476 Northampton County ¤£ 202 222 §¨¦ ¤£ !( Lehigh County Bethlehem §¨¦ Pennsylvania §¨¦ ¤£ ¤£ !( !( §¨¦ Allentown §¨¦ §¨¦ New Jersey §¨¦ ¤£ §¨¦ ¤£ 0 2.75 5.5 11¤£ Miles - Federally-funded site 116th Congressional (each color represents one organization) District Boundaries Major Highways County Boundaries NUMBER OF DELIVERY SITES IN Highways City or Town CONGRESSIONAL DISTRICT 3 Major Roads Notes | Delivery sites represent locations of organizations funded by the federal Health Center Program. Some locations may overlap due to scale or may otherwise not be visible when mapped. Federal investments represent the total funding from the federal Health Center Program to grantees with a presence in the state in 2017. Sources | Federally-Funded Delivery Site Locations: data.HRSA.gov, December 3, 2018. Health Center Patients and Federal Funding | 2017 Uniform Data System, Bureau of Primary Health Care, HRSA. © National Association of Community Health Centers, 2019. For more information, please contact [email protected]. Representative Susan Wild 116th United States Congress Pennsylvania's 7TH Congressional District NUMBER OF DELIVERY SITES IN 3 CONGRESSIONAL DISTRICT (main organization in bold) NEIGHBORHOOD HEALTH CENTERS OF THE LEHIGH VALLEY Neighborhood Health Centers of Lehigh Valley - Easton - 1101 Northampton St Ste 102 Easton, PA 18042-4152 Neighborhood Health Centers of the Lehigh Valley- Bethlehem - 1210 E 4th St Bethlehem, PA 18015 Vida Nueva at Casa Guadalupe - 218 N 2nd St Allentown, PA 18102-3508 Sources | Federally-Funded Delivery Site Locations: data.HRSA.gov, December 3, 2018. -

Congressional Delegation December 4, 2020 Page 2
December 4, 2020 The Honorable Bob Casey The Honorable Pat Toomey 393 Russell Senate Office Building 248 Russell Senate Office Building United States Senate United States Senate Washington, D.C. 20510 Washington, D.C 20510 The Honorable Brian Fitzpatrick The Honorable Brendan Boyle 1722 Longworth House Office Building 1133 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Dwight Evans The Honorable Madeleine Dean 1105 Longworth House Office Building 129 Cannon House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Mary Gay Scanlon The Honorable Chrissy Houlahan 1535 Longworth House Office Building 1218 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Susan Wild The Honorable Matthew Cartwright 1607 Longworth House Office Building 1034 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Daniel Meuser The Honorable Scott Perry 326 Cannon House Office Building 1207 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Lloyd Smucker The Honorable Fred Keller 127 Cannon House Office Building 1717 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 Pennsylvania’s Congressional Delegation December 4, 2020 Page 2 The Honorable John Joyce The Honorable Guy Reschenthaler 1337 Longworth House Office Building 531 Cannon House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Glenn Thompson The Honorable Mike Kelly 400 Cannon House Office Building 1707 Longworth House Office Building United States Congress United States Congress Washington, DC 20515 Washington, DC 20515 The Honorable Conor Lamb The Honorable Michael Doyle Jr. -

03/19/2021 the Honorable Thomas Vilsack Secretary United States Department of Agriculture 1400 Independence Ave., S.W
03/19/2021 The Honorable Thomas Vilsack Secretary United States Department of Agriculture 1400 Independence Ave., S.W. Washington, DC 20250 Dear Secretary Vilsack: We write to congratulate you on your confirmation and request your support in researching and combatting the Spotted Lanternfly (SLF), an invasive species of planthopper insect from southeast Asia. We have worked with the U.S. Department of Agriculture (USDA) on a bipartisan basis for the past two years to address the negative impacts of the SLF on our farmers and agricultural workers. Additional resources are still needed to rid our regions of this pest, and as you finalize your Fiscal Year 2022 (FY22) budget request, we urge you to request an increase in support to research and control the SLF. Spotted Lanternflies were first found in Berks County, Pennsylvania in 2014. Since that initial discovery, they have been found throughout the states of Pennsylvania, New York, Maryland, Virginia, New Jersey, Connecticut, West Virginia, Ohio and Delaware, and they continue to spread across the country. These invasive pests are threatening our agricultural industries including vineyards, orchards, ornamental nurseries, and hardwoods. According to economic research from the Center for Rural Pennsylvania, the damage caused by the SLF could cost the Commonwealth $324 million annually and cause the loss of over 2,800 jobs in Pennsylvania alone1. In Chester County alone, up to $66.9 million in orchards, vineyards, Christmas tree farms, and nursery products are potentially at risk from damage by SLF2. Grape growers are at a particularly significant risk of damage with reported yield losses, reduction in fruit quality, and even vine death. -

Key Committees for the 116Th Congress
TH KEY COMMITTEES FOR THE 116 CONGRESS APPROPRIATIONS COMMITTEES The Senate and House Appropriations Committees determine how federal funding for discretionary programs, such as the Older Americans Act (OAA) Nutrition Program, is allocated each fiscal year. The Subcommittees overseeing funding for OAA programs in both the Senate and the House are called the Labor, Health and Human Services, Education and Related Agencies Subcommittees. Listed below, by rank, are the Members of Congress who sit on these Committees and Subcommittees. Senate Labor, Health & Human Services, Education, and Related Agencies Appropriations Subcommittee Republicans (10) Democrats (9) Member State Member State Roy Blunt, Chairman Missouri Patty Murray, Ranking Member Washington Richard Shelby Alabama Dick Durbin Illinois Lamar Alexander Tennessee Jack Reed Rhode Island Lindsey Graham South Carolina Jeanne Shaheen New Hampshire Jerry Moran Kansas Jeff Merkley Oregon Shelley Moore Capito West Virginia Brian Schatz Hawaii John Kennedy Louisiana Tammy Baldwin Wisconsin Cindy Hyde-Smith Mississippi Chris Murphy Connecticut Marco Rubio Florida Joe Manchin West Virginia James Lankford Oklahoma Senate Appropriations Committee Republicans (16) Democrats (15) Member State Member State Richard Shelby, Chairman Alabama Patrick Leahy, Ranking Member Vermont Mitch McConnell Kentucky Patty Murray Washington Lamar Alexander Tennessee Dianne Feinstein California Susan Collins Maine Dick Durbin Illinois Lisa Murkowski Alaska Jack Reed Rhode Island Lindsey Graham South Carolina