Multicenter Randomized Controlled Trial of Vitamin K Antagonist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vitamin K: Double Bonds Beyond Coagulation Insights Into Differences Between Vitamin K1 and K2 in Health and Disease
International Journal of Molecular Sciences Review Vitamin K: Double Bonds beyond Coagulation Insights into Differences between Vitamin K1 and K2 in Health and Disease Maurice Halder 1,†, Ploingarm Petsophonsakul 2,†, Asim Cengiz Akbulut 2,†, Angelina Pavlic 2,† , Frode Bohan 3, Eric Anderson 3, Katarzyna Maresz 4, Rafael Kramann 1 and Leon Schurgers 1,2,* 1 Division of Nephrology, RWTH Aachen University, 52074 Aachen, Germany; [email protected] (M.H.); [email protected] (R.K.) 2 Department of Biochemistry, Cardiovascular Research Institute Maastricht, 6200MD Maastricht, The Netherlands; [email protected] (P.P.); [email protected] (A.C.A.); [email protected] (A.P.) 3 NattoPharma ASA, 0283 Oslo, Norway; [email protected] (F.B.); [email protected] (E.A.) 4 International Science & Health Foundation, 30-134 Krakow, Poland; [email protected] * Correspondence: [email protected]; Tel.: +31-43-3881680; Fax: +31-43-3884159 † These authors contributed equally to this work. Received: 24 January 2019; Accepted: 16 February 2019; Published: 19 February 2019 Abstract: Vitamin K is an essential bioactive compound required for optimal body function. Vitamin K can be present in various isoforms, distinguishable by two main structures, namely, phylloquinone (K1) and menaquinones (K2). The difference in structure between K1 and K2 is seen in different absorption rates, tissue distribution, and bioavailability. Although differing in structure, both act as cofactor for the enzyme gamma-glutamylcarboxylase, encompassing both hepatic and extrahepatic activity. Only carboxylated proteins are active and promote a health profile like hemostasis. Furthermore, vitamin K2 in the form of MK-7 has been shown to be a bioactive compound in regulating osteoporosis, atherosclerosis, cancer and inflammatory diseases without risk of negative side effects or overdosing. -

Randomised Controlled Trial of Nutritional Supplement on Bone Turnover Markers in Indian Premenopausal Women
nutrients Article Randomised Controlled Trial of Nutritional Supplement on Bone Turnover Markers in Indian Premenopausal Women Pramod B. Umarji 1, Pankaj Verma 2, Vivek Garg 2, Marian Schini 3,* and Richard Eastell 3 1 Umarji Healthcare, Pune, Maharashtra 411045, India; [email protected] 2 Hindustan Unilever Limited R&D, Gurugram, Haryana 122002, India; [email protected] (P.V.); [email protected] (V.G.) 3 Academic Unit of Bone Metabolism, University of Sheffield, Sheffield S10 2NR, UK; r.eastell@sheffield.ac.uk * Correspondence: m.schini@sheffield.ac.uk; Tel.: +44-0114-215-9667 Abstract: Young Indian women may be at risk of poor bone health due to malnutrition. The aim of this study was to examine the effects on bone metabolism of a nutritional supplement in women aged 25 to 44. The nutritional supplement was a protein-rich beverage powder fortified with multi- micronutrients including calcium (600 mg), vitamin D (400 IU), and vitamin K (55 mcg) per daily serving, while a placebo supplement was low-protein non-fortified isocaloric beverage powder. This 6-month randomised, controlled trial showed favorable changes in bone turnover markers (decreased) and calcium homeostasis; such changes in older adults have been associated with slowing of bone loss and reduced fracture risk. For example, serum CTX decreased by about 30% and PINP by about 20% as a result of the increase in calcium intake. There were also changes in the ratio of carboxylated to undercarboxylated osteocalcin and such changes have been linked to a slowing of bone loss in older subjects. For example, the ratio increased by about 60% after 3 months as a result in the improvement in vitamin K status. -

Vitamin K the “Forgotten” Vitamin
Vitamin K The “Forgotten” Vitamin Ask anybody what vitamins they know about, and you’re likely to hear Vitamin C, Vitamin D, Vitamin E, and many people will even know that there are multiple vitamins called B. But if you ask about Vitamin K, a lot of people will say “is that really a thing?” Well, we’re here to tell you that not only is it a thing, but it’s as essential as any of the other vitamins you may have heard of. That’s why it’s one of the so-called “13 Essential Vitamins,” which are actually REQUIRED by our bodies in order to Function. Complicating matters even more is the fact that Vitamin K is actually a COMPLEX of vitamins, each with its own distinct properties. In order to understand Vitamin K, its importance in our diet, how to make sure we’re getting all the benefits of it, and how it interacts with other vitamins, we need to know what it is, what it does, what foods it can be found in, and what the different types are. Not Just One Vitamin Just as Vitamin B is actually a whole group of vitamins (B6, B12, Niacin, Riboflavin, etc.), Vitamin K is also a group of compounds, and not just one vitamin. The two most important of these are K1 and K2. There is also a synthetic form of Vitamin K known a K3, but as it can be toxic, it is not generally used in supplementation. Clean, Quiet, & Dark To make things even more complicated, there are two different forms of Vitamin K2 – MK4 and MK7. -

Vitamin K2 Needs an RDI Separate from Vitamin K1
nutrients Review Vitamin K2 Needs an RDI Separate from Vitamin K1 1, 1, 1, Asim Cengiz Akbulut y, Angelina Pavlic y , Ploingarm Petsophonsakul y , 2, 3 2 1,2, Maurice Halder y , Katarzyna Maresz , Rafael Kramann and Leon Schurgers * 1 Department of Biochemistry, Cardiovascular Research Institute Maastricht, 6200MD Maastricht, The Netherlands; [email protected] (A.C.A.); [email protected] (A.P.); [email protected] (P.P.) 2 Division of Nephrology, RWTH Aachen University, 52074 Aachen, Germany; [email protected] (M.H.); [email protected] (R.K.) 3 International Science & Health Foundation, 30-134 Krakow, Poland; [email protected] * Correspondence: [email protected]; Tel.: +31-43-3881680; Fax: +31-43-3884159 These authors contributed equally to this work. y Received: 25 May 2020; Accepted: 17 June 2020; Published: 21 June 2020 Abstract: Vitamin K and its essential role in coagulation (vitamin K [Koagulation]) have been well established and accepted the world over. Many countries have a Recommended Daily Intake (RDI) for vitamin K based on early research, and its necessary role in the activation of vitamin K-dependent coagulation proteins is known. In the past few decades, the role of vitamin K-dependent proteins in processes beyond coagulation has been discovered. Various isoforms of vitamin K have been identified, and vitamin K2 specifically has been highlighted for its long half-life and extrahepatic activity, whereas the dietary form vitamin K1 has a shorter half-life. In this review, we highlight the specific activity of vitamin K2 based upon proposed frameworks necessary for a bioactive substance to be recommended for an RDI. -
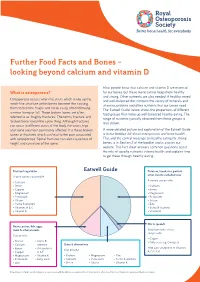
Further Food Facts and Bones – Looking Beyond Calcium and Vitamin D
Further Food Facts and Bones – looking beyond calcium and vitamin D Most people know that calcium and vitamin D are essential What is osteoporosis? for our bones, but these alone cannot keep them healthy and strong. Other nutrients are also needed. A healthy, mixed Osteoporosis occurs when the struts which make up the and well-balanced diet contains the variety of minerals and mesh-like structure within bones become thin causing vitamins, proteins and other nutrients that our bones need. them to become fragile and break easily, often following The ‘Eatwell Guide’ below shows the proportions of different a minor bump or fall. These broken bones are often food groups that make up well-balanced healthy eating. The referred to as ‘fragility fractures’. The terms ‘fracture’ and range of nutrients typically obtained from these groups is ‘broken bone’ mean the same thing. Although fractures also shown. can occur in different parts of the body, the wrists, hips and spine are most commonly affected. It is these broken A more detailed picture and explanation of the Eatwell Guide bones or fractures which can lead to the pain associated is in our booklet ‘All about osteoporosis and bone health’. with osteoporosis. Spinal fractures can also cause loss of This, and the central message on healthy eating for strong height and curvature of the spine. bones, is in Section 2 of the booklet and is also on our website. This fact sheet answers common questions about the role of specific nutrients in bone health and explains how to get these through healthy eating. -

Vitamin K, an Example of Triage Theory: Is Micronutrient Inadequacy Linked to Diseases of Aging?1–3
Perspective Vitamin K, an example of triage theory: is micronutrient inadequacy linked to diseases of aging?1–3 Joyce C McCann and Bruce N Ames ABSTRACT selection, metabolic resources are preferentially allocated to The triage theory posits that some functions of micronutrients (the functions necessary for reproductive survival at the expense of ’40 essential vitamins, minerals, fatty acids, and amino acids) are those required for survival beyond reproductive age. The triage restricted during shortage and that functions required for short-term theory is unique in that it proposes a mechanistic trigger for the survival take precedence over those that are less essential. Insidious reallocation of micronutrient-dependent metabolic resources and Downloaded from changes accumulate as a consequence of restriction, which increases suggests that age-related disease is easily preventable by en- the risk of diseases of aging. For 16 known vitamin K–dependent suring an adequate supply of micronutrients. (VKD) proteins, we evaluated the relative lethality of 11 known If the theory is correct, the implications for public health are mouse knockout mutants to categorize essentiality. Results indicate enormous. Virtually every metabolic pathway includes one or that 5 VKD proteins that are required for coagulation had critical more enzymes that require essential micronutrients for activity. functions (knockouts were embryonic lethal), whereas the knockouts Micronutrient intake below recommended concentrations, but not www.ajcn.org of 5 less critical VKD proteins [osteocalcin, matrix Gla protein severe enough to cause overt clinical symptoms, is widespread (Mgp), growth arrest specific protein 6, transforming growth factor not only in poor countries but also in the United States (especially b–inducible protein (Tgfbi or big-h3), and periostin] survived at in the poor, children, adolescents, the obese, and the elderly), least through weaning. -

VITAMINS D3 and K2 – Another Dynamic Duo!
VITAMINS D3 AND K2 – Another Dynamic Duo! By Dr Nyjon K. Eccles BSc MBBS MRCP PhD Introduction In my last article “Vitamin D: An Underestimated Ally”, I summarised the science behind the many beneFits oF Vitamin D and how in the light oF this accumulating scientiFic support that no-one can aFFord to be deFicient in this important hormone. And yet evidence would indicate that as many as 70% oF us may be deFicient or have too low levels oF this God-given molecule. People are becoming aware oF this and although they may not have checked their blood levels, have taken it upon themselves to large doses oF vitamin D3. Whilst undoubtedly there are benefits to correcting your vitamin D deficiency, there lies a hidden danger in taking large doses oF Vitamin D3 without its sister vitamin, Vitamin K2. This article aims to clariFy the synergy between these two important molecules and explain why we need them both together For optimum bone and cardiovascular health. To reiterate, Vitamin D has been shown to inFluence dozens of conditions, including: Cancer, Hypertension, Heart Disease, Obesity, Rheumatoid Arthritis, Autism, Type 1 and Type 2 Diabetes, Osteoporosis, Multiple Sclerosis, Crohn’s and other InFlammatory Bowel disease, Flu, Tuberculosis, Dementia and Alzheimers, Eczema and Psoriasis, Muscle pain, Peridontal disease, Macular degeneration, Pre-eclampsia, InFertility, Asthma, Cystic Fibrosis, Migraines, Depression, Schizophrenia and Seizures. Some of these have been discussed in more detail in my previous article referenced above. The RDA for vitamin D remains at a measly 600 IUs. This is despite the overwhelming evidence showing that vitamin D is extremely important for a wide variety of health conditions besides bone health, and that most people may need about ten times this amount or more. -

High-Dose Vitamins
BREASTFEEDING MEDICINE c Volume 14, Number 5, 2019 LactMed Update ª Mary Ann Liebert, Inc. DOI: 10.1089/bfm.2019.0077 High-Dose Vitamins Jason B. Sauberan1,2 oncentrations of most vitamins in breast milk are creases milk concentrations by 30–70 mcg/L in both under- Cdependent on maternal diet.1 Daily vitamin supple- and well-nourished lactating mothers. mentation to achieve adequate dietary intake is thus a re- The highest supplemental dose studied has been 10 mg/day; commended intervention for lactating mothers who are milk concentrations increased from 200 mcg/L at baseline to undernourished, or for those with dietary restrictions. Even in 750 mcg/L after several months of supplementation.8 There mothers with no known dietary deficiency risks, the use of have been no reports of milk concentrations or breastfed in- prenatal vitamins during lactation is commonplace and is fant safety during maternal high-dose riboflavin therapy. considered safe for the breastfed infant (Table 1).2,3 Some Intravenous high-dose riboflavin has been safely used in lactating mothers may elect to consume high-dose or hyperbilirubinemic newborns as an adjunct to phototherapy. ‘‘megadose’’ vitamin therapy, beyond that required for ade- Riboflavin is considered to have a wide safety margin in quate daily intake. Commonly used vitamins taken in humans and there is no established upper limit of tolerability. megadoses are listed in Table 2. Depending on the vitamin, A common benign side effect of larger doses is bright yellow dosage, and the mother’s underlying vitamin status, this urine discoloration.6,9 Owing to a lack of data, other drugs for practice could potentially lead to vitamin concentrations in migraine prophylaxis with good safety records during milk that are harmful to the infant. -

Brands and Types of Supplements We Recommend
Brands and Types of Supplements We Recommend Magnesium glycinate http://amzn.to/2mdZC4W Bifido bacteria http://amzn.to/2mTG1UG l-carnitine http://amzn.to/2mdWw0O l-tyrosine http://amzn.to/2mTGeHs Estrovera http://amzn.to/2nCrxZs Kaprex http://amzn.to/2nCqjgG Ultraflora Spectrum http://amzn.to/2mG7sk6 D-HIST http://amzn.to/2mTJvH1 Lipotain http://amzn.to/2mD1sYz SAMe (Do not take with antidepressant) http://amzn.to/2oqcgxC Vitamin B-6 http://amzn.to/2o07Yd7 Magnesium L-Threonate http://amzn.to/2nZRSk4 Siberian Ginseng http://amzn.to/2mD80Gq GLYCINE http://amzn.to/2wRbYVR l-glutamine http://amzn.to/2ojMBop GELATIN http://amzn.to/2nxHzHK The Green can doesn’t gel up (Red can does, like jello) if you prefer that. http://amzn.to/2nxSocC Emu Oil http://amzn.to/2w9VGpn Kelp (for iodine) http://amzn.to/2n8CzYJ Estrofactors http://amzn.to/2mefc0x potassium http://amzn.to/2mGqd6K Heath Tip: There are a couple of prescription medicines that you’ve got to be aware of if you significantly increase your potassium intake, so if you’re on blood pressure medicines, talk to your doctor before you to take potassium. Vitamin D Make sure to take WITH FOOD and in the AM. Take 1000iu per 25 pounds you weigh. http://amzn.to/2mTQwYb Vitamin K2 http://amzn.to/2mTT34F Selenium http://amzn.to/2nk8YM6 7-KETO http://amzn.to/2nCKjjs Resveratrol: http://amzn.to/2nknDqD CURCUMIN: http://amzn.to/2mTJItt B-Complex http://amzn.to/2nxKDDO chromium (with cinnamon) http://amzn.to/2nCDzBT Choline http://amzn.to/2n8Io8t Zinc: http://amzn.to/2mTGyWP OsteoVantiv http://amzn.to/2mG5wIp Berberine http://amzn.to/2mG6XGC Ultra Potent Vitamin C http://amzn.to/2nCLwau HCL with Pepsin http://amzn.to/2oYA5dC Ashwagahnda http://amzn.to/2ogIRWP GUGGAL http://amzn.to/2mTRGTE CoQ10. -
Vitamin K and Thrombosis
Vitamin K and thrombosis Rithik Raina, Ayush Karnik, Prasad Shetye, Atul Laddu, On Behalf of the Georgia Thrombosis Forum The role of the fat soluble vitamin K (VK) in thrombosis is getting more clear every day. VK plays a major role in the coagulation cascade. VK deficiency can occur in any age group, but is encountered most often in infancy. The body needs VK to use calcium to build bone. Low levels of VK may be associated with a higher risk of osteoarthritis. VK improves bone health and reduces the risk of bone fractures, particularly in postmenopausal women who are at risk for osteoporosis. Our research in the physiology, role in thrombosis and uses of VK tell us that VK is one of the very important vitamins in life. Although use of warfarin is gradually going down due to the discovery of NOAC’s, warfarin is there to stay, and therefore we know that vitamin K is going to stay. Introduction Following the discovery of warfarin, a Vitamin K Antagonist (VKA), the importance of Vitamin K has become more apparent. The “K” in Vitamin K originated from the German word, "koagulation". Millions of patients who take warfarin for atrial fibrillation, DVT, PE, and prosthetic cardiac valves. The wide use of warfarin, an agent with a very narrow therapeutic index, has resulted in significant risk for major bleeding. Vitamin K serves as one of the major reversing agents for patients over- anticoagulated with warfarin. We at GTF took a challenge of researching the physiology of vitamin K and its role in thrombosis. -

Association of Dietary Vitamin K and Risk of Coronary Heart Disease in Middle- Age Adults: the Hordaland Health Study Cohort
Open access Original research BMJ Open: first published as 10.1136/bmjopen-2019-035953 on 21 May 2020. Downloaded from Association of dietary vitamin K and risk of coronary heart disease in middle- age adults: the Hordaland Health Study Cohort Teresa R Haugsgjerd ,1 Grace M Egeland,1,2 Ottar K Nygård,3,4 Kathrine J Vinknes,5 Gerhard Sulo,6,7 Vegard Lysne,4 Jannicke Igland,1 Grethe S Tell1,8 To cite: Haugsgjerd TR, ABSTRACT Strengths and limitations of this study Egeland GM, Nygård OK, Objective The role of vitamin K in the regulation of et al. Association of dietary vascular calcification is established. However, the ► The study had a long follow-up time with minimal vitamin K and risk of coronary association of dietary vitamins K1 and K2 with risk of heart disease in middle- age competing risk from other causes of death. coronary heart disease (CHD) is inconclusive. adults: the Hordaland Health ► Linkage to a nationwide database assured complete Design Prospective cohort study. Study Cohort. BMJ Open cohort follow- up. Setting We followed participants in the community- based 2020;10:e035953. doi:10.1136/ ► We had information on history of coronary heart dis- Hordaland Health Study from 1997 - 1999 through 2009 bmjopen-2019-035953 ease (CHD) at baseline which enabled us to evaluate to evaluate associations between intake of vitamin K and incident (new onset) CHD. ► Prepublication history and incident (new onset) CHD. Baseline diet was assessed by additional material for this ► The Food Frequency Questionnaire was not validat- a past- year food frequency questionnaire. Energy- adjusted paper are available online. -

A•D•K2 Cardio Healthtm*
FEATURED PRODUCT TM A •D•K2 Cardio Health * For Vascular Elasticity and Strength* SUPPLEMENT FACTS ® Serving Size: 1 Softgel Strong Support for Servings Per Container: 60 Your Heart and Arteries* Amount Per 1 Softgel: %DV • Cardiovascular Health Vitamin A (as retinyl palmitate) 3,000 mcg (10,000 IU) 333% Vitamin D3 (as cholecalciferol) 125 mcg (5,000 IU) 625% • Blood Vessel Elasticity A•D•K2 Vitamin K2 45 mcg 38% [as menaquinone-7 (MK-7 as Mena Q7®)] ™ • Arterial Wall Strength* * Cardio Health Other Ingredients: extra virgin olive oil, gelatin, sunflower seed oil, glycerol, water, alpha tocopherol Recommendations: 1 softgel daily, For Vascular acetate, rosemary extract. No sugar, salt, yeast, wheat, gluten, corn, soy, or as recommended by your Elasticity and Strength* dairy products, artificial coloring, artificial flavoring, healthcare practitioner. or artificial preservatives. If pregnant or nursing, consult a healthcare practitioner before use. Product of Belgium Mena Q7® is a trademark of NattoPharma ASA, Norway. * THESE STATEMENTS HAVE NOT BEEN EVALUATED BY THE FOOD AND DRUG ADMINISTRATION. 60 Softgels Manufactured by a cGMP compliant facility exclusively for: THIS PRODUCT IS NOT INTENDED TO DIAGNOSE, TREAT, CURE OR PREVENT ANY DISEASE. EuroMedica 955 Challenger Drive Green Bay, WI 54311 L90586.03 NON-GMO DIETARY SUPPLEMENT 866-842-7256 euromedicausa.com Label Size 2.5”x 7” Bar Code Number: 3 67703 90586 6 Keep your arteries strong, smooth, and flexible with A•D•K2 Vitamin K2: Also known as menaquinone, vitamin K2 is Cardio Health. Your body needs the fat-soluble vitamins A, D3, essential to maintaining the healthy structure of the arterial and K2 to support vascular health and healthy calcium level wall and is a key player in directing calcium’s proper utilization.