Product Monograph Amatine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

1Hol=C2 Light Water (C2 > C1) Patent Application Publication May 1, 2008 US 2008/O103092 A1 5 (1H2O=C2
US 20080 103092A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0103092 A1 Pomytkin et al. (43) Pub. Date: May 1, 2008 (54) METHODS FOR INTRADERMAL, Publication Classification TRANSIDERMAL, ORTRANSMUCOSAL DELIVERY OF BIOLOGICALLY ACTIVE (51) Int. Cl. SUBSTANCES A6II 47/02 (2006.01) A6II 38/02 (2006.01) (76) Inventors: Igor Anatolievich Pomytkin, Moscow A6IR 48/00 (2006.01) (RU); Sergey Pavlovich Soloviev, (52) U.S. Cl. .................................... 514/8: 514/2: 514/769 Moscow (RU) (57) ABSTRACT Correspondence Address: NOTARO AND MICHALOS This invention relates to method for intradermal, transdermal 1OO DUTCH HILL ROAD or transmucosal delivering a biologically active Substance to a mammal in need thereof, which method comprises a step of SUTE 110 co-administering to said mammal with the biologically active ORANGEBURG, NY 10962-2100 (US) Substance an effective amount of an absorption enhancer, which is water comprising from about 99.760 to about 10 (21) Appl. No.: 11/817,919 99.999% of light isotopologue H, 0 and up to 100% of residual isotopologues H, '70, H., '80, HH'0, HH'70, (22) PCT Filed: Mar. 11, 2005 'HH'0, H, O, H, '70, and H 0. Such biologically (86) PCT NO.: PCT/RUOS/OO108 active substance is selected from the group consisting of drugs, physiologically active peptides, physiologically active S371(c)(1), proteins, glycoproteins, nucleic acid, nutrients, vitamins, and (2), (4) Date: Nov. 15, 2007 minerals. 5 1Hol=C2 Light Water (C2 > C1) Patent Application Publication May 1, 2008 US 2008/O103092 A1 5 (1H2O=C2 Light Water (C2 > C1) Licuid US 2008/O 103092 A1 May 1, 2008 METHODS FOR INTRADERMAL, TRANSDERMAL wherein the level of light water isotopologue 'H'Ois about ORTRANSMUCOSAL DELIVERY OF 99.7317% (Vienna Standard Mean Ocean Water, VSMOW), BIOLOGICALLY ACTIVE SUBSTANCES and wherein total level of all eight heavy isotopologues com prising at least one heavy isotopes H, O, and 'O is about TECHNICAL FIELD 0.2683% (e.g. -

Antihypotensive Agent Disrupts the Immune System in Sepsis 12 June 2020
Antihypotensive agent disrupts the immune system in sepsis 12 June 2020 Patients who go into septic shock are treated with with endotoxin, a bacterial cell-wall component. If the antihypotensive agent norepinephrine. mice were administered norepinephrine, their Researchers from Radboud University Medical immune response was strongly suppressed." Center published results in today's American Journal of Respiratory and Critical Care Medicine Furthermore, in mice with an actual bacterial revealing that its use is not without drawbacks: The infection, infusion of norepinephrine led to drug disrupts the immune system and increases increased bacterial growth in the spleen, liver, and susceptibility to infections. This may have negative blood, again indicating a weakened immune consequences for patients. Research into system. "We also studied the effect of vasopressin, alternatives is therefore justified. an alternative antihypotensive agent, on white blood cells and mice," Stolk says. "Interestingly, in Sepsis is a life-threatening inflammatory response contrast to norepinephrine, this drug has no effects spreading throughout the body due to an infection. on the immune system or defense against One in four patients with sepsis succumbs to it, infections." and it is the No. 1 cause of death around the globe. As such, sepsis was recently designated as Healthy volunteers a global health priority by the World Health Organization (WHO). Patients with sepsis have a "Next, we wanted to know whether the effects of severely dysregulated immune system, which norepinephrine also apply to humans," said Matthijs impairs clearance of the infection and leaves the Kox, head of the study. "We infused either body susceptible to new infections with an norepinephrine, vasopressin, or a placebo in three increased risk of death. -

Antiparasitic Properties of Cardiovascular Agents Against Human Intravascular Parasite Schistosoma Mansoni
pharmaceuticals Article Antiparasitic Properties of Cardiovascular Agents against Human Intravascular Parasite Schistosoma mansoni Raquel Porto 1, Ana C. Mengarda 1, Rayssa A. Cajas 1, Maria C. Salvadori 2 , Fernanda S. Teixeira 2 , Daniel D. R. Arcanjo 3 , Abolghasem Siyadatpanah 4, Maria de Lourdes Pereira 5 , Polrat Wilairatana 6,* and Josué de Moraes 1,* 1 Research Center for Neglected Diseases, Guarulhos University, Praça Tereza Cristina 229, São Paulo 07023-070, SP, Brazil; [email protected] (R.P.); [email protected] (A.C.M.); [email protected] (R.A.C.) 2 Institute of Physics, University of São Paulo, São Paulo 05508-060, SP, Brazil; [email protected] (M.C.S.); [email protected] (F.S.T.) 3 Department of Biophysics and Physiology, Federal University of Piaui, Teresina 64049-550, PI, Brazil; [email protected] 4 Ferdows School of Paramedical and Health, Birjand University of Medical Sciences, Birjand 9717853577, Iran; [email protected] 5 CICECO-Aveiro Institute of Materials & Department of Medical Sciences, University of Aveiro, 3810-193 Aveiro, Portugal; [email protected] 6 Department of Clinical Tropical Medicine, Faculty of Tropical Medicine, Mahidol University, Bangkok 10400, Thailand * Correspondence: [email protected] (P.W.); [email protected] (J.d.M.) Citation: Porto, R.; Mengarda, A.C.; Abstract: The intravascular parasitic worm Schistosoma mansoni is a causative agent of schistosomiasis, Cajas, R.A.; Salvadori, M.C.; Teixeira, a disease of great global public health significance. Praziquantel is the only drug available to F.S.; Arcanjo, D.D.R.; Siyadatpanah, treat schistosomiasis and there is an urgent demand for new anthelmintic agents. -

Identification of Designer Drugs Using Gas Chromatography High-Resolution Mass Spectrometry and a Soft-Ionization Source
Journal of Forensic Science & Criminology Volume 1 | Issue 3 ISSN: 2348-9804 Research Article Open Access Identification of Designer Drugs using Gas Chromatography High-Resolution Mass Spectrometry and A Soft-Ionization Source Lopez-Avila V* Agilent Technologies, USA *Corresponding author: Lopez-Avila V, Agilent Technologies, Santa Clara, CA 95051, USA, Fax: (408) 553- 3677, Tel: (408) 553-2709, E-mail: [email protected] Citation: Lopez-Avila V (2013) Identification of Designer Drugs using Gas Chromatography High-Resolution Mass Spectrometry and a Soft-Ionization Source. J Forensic Sci Criminol 1(3): 301. doi: 10.15744/2348- 9804.1.301 Received Date: September 27, 2013 Accepted Date: December 11, 2013 Published Date: December 16, 2013 Abstract A small set of amphetamines has been analyzed by gas chromatography (GC) high-resolution time-of-flight mass spectrometry (TOFMS) using a microplasma photoionization (MPPI) soft-ionization source. This plasma-based, wavelength selectable ionization source enables ionization of the test compounds and their corresponding derivatives at ~8-12 eV that is a softer alternative to electron ionization at 70 eV. Three plasma gases were used in this study: Xe plasma that emits photons at resonance lines of 9.57 eV and 8.44 eV; Kr plasma at 10.63 eV and 10.02 eV, and Ar plasma at 11.82 eV and 11.61 eV. Derivatization of the test compounds with trifluoroacetic anhydride and α-methoxy-α-(trifluoromethyl)-phenylacetyl pyrazole was evaluated because the MPPI mass spectra of the underivatized amphetamines yield primarily iminium ions, which make the identification of the test compounds by GC-TOFMS inconclusive. -

Midodrine Hydrochloride Tablets, USP Rx Only
MIDODRINE HCL- midodrine hydrochloride tablet Eon Labs, Inc. ---------- Midodrine Hydrochloride Tablets, USP Rx Only WARNING Because midodrine hydrochloride tablets can cause marked elevation of supine blood pressure, it should be used in patients whose lives are considerably impaired despite standard clinical care. The indication for use of midodrine hydrochloride tablets in the treatment of symptomatic orthostatic hypotension is based primarily on a change in a surrogate marker of effectiveness, an increase in systolic blood pressure measured one minute after standing, a surrogate marker considered likely to correspond to a clinical benefit. At present, however, clinical benefits of midodrine hydrochloride tablets, principally improved ability to carry out activities of daily living, have not been verified. DESCRIPTION Midodrine hydrochloride is a vasopressor/antihypotensive agent. Midodrine hydrochloride is an odorless, white, crystalline powder, soluble in water and sparingly soluble in methanol having a pKa of 7.8 (0.3% aqueous solution), a pH of 3.5 to 5.5 (5% aqueous solution) and a melting range of 200°C to 203°C. It is chemically described as: (1) Acetamide, 2-amino-N-[2-(2,5-dimethoxyphenyl)-2- hydroxyethyl]-monohydrochloride, (±)-; or (2) (±)-2-amino-N-(ß-hydroxy-2,5- dimethoxyphenethyl)acetamide monohydrochloride. Midodrine hydrochloride’s molecular formula is C12H18N2O4HCl, its molecular weight is 290.7 and its structural formula is: Each tablet for oral administration contains 2.5 mg, 5 mg or 10 mg of midodrine hydrochloride and the following inactive ingredients: pregelatinized starch (corn starch), microcrystalline cellulose, colloidal silicon dioxide, magnesium stearate. In addition, the 5 mg tablets contain FD&C yellow No. -

(12) Patent Application Publication (10) Pub. No.: US 2011/0263526 A1 SATYAM (43) Pub
US 20110263526A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0263526 A1 SATYAM (43) Pub. Date: Oct. 27, 2011 (54) NITRICOXIDE RELEASING PRODRUGS OF CD7C 69/96 (2006.01) THERAPEUTICAGENTS C07C 319/22 (2006.01) CD7C 68/02 (2006.01) (75) Inventor: Apparao SATYAM, Mumbai (IN) A6IP 29/00 (2006.01) A6IP 9/00 (2006.01) (73) Assignee: PIRAMAL LIFE SCIENCES A6IP37/08 (2006.01) LIMITED, Mumbai (IN) A6IP35/00 (2006.01) A6IP 25/24 2006.O1 (21) Appl. No.: 13/092.245 A6IP 25/08 308: A6IP3L/04 2006.O1 (22) Filed: Apr. 22, 2011 A6IP3L/2 308: Related U.S. Application Data 39t. O 308: (60) Provisional application No. 61/327,175, filed on Apr. A6IP3/10 (2006.01) 23, 2010. A6IPL/04 (2006.01) A6IP39/06 (2006.01) Publication Classification A6IP3/02 (2006.01) (51) Int. Cl. A6IP 9/06 (2006.01) A 6LX 3L/7072 (2006.01) 39t. W 308: A6 IK3I/58 (2006.01) A6IP II/08 (2006.015 A6 IK3I/55 (2006.01) A63/62 (2006.015 A6 IK 3/495 (2006.01) A6 IK 3/4439 (2006.01) (52) U.S. Cl. ........... 514/50: 514/166; 514/172: 514/217; A6 IK 3L/455 (2006.01) 514/255.04: 514/338; 514/356; 514/412; A6 IK 3/403 (2006.01) 514/420; 514/423: 514/510,536/28.53:540/67; A6 IK 3/404 (2006.01) 540/591; 544/396; 546/273.7: 546/318: 548/452: A6 IK 3/40 (2006.01) 548/500: 548/537; 549/464; 558/275 A6 IK3I/265 (2006.01) C7H 9/06 (2006.01) (57) ABSTRACT CO7I 71/00 (2006.01) CO7D 22.3/26 (2006.01) The present invention relates to nitric oxide releasing pro C07D 295/14 (2006.01) drugs of known drugs or therapeutic agents which are repre CO7D 40/12 (2006.01) sented herein as compounds of formula (I) wherein the drugs CO7D 213/80 (2006.01) or therapeutic agents contain one or more functional groups C07D 209/52 (2006.01) independently selected from a carboxylic acid, an amino, a CO7D 209/26 (2006.01) hydroxyl and a sulfhydryl group. -

Idiopathic Orthostatic Hypotension, Midodrine, and Anaesthesia
499 Idiopathic orthostatic hypotension, mido- P.J. Osborne MD, L.W. Lee MD drine, and anaesthesia A patient with idiopathic orthostatic hypotension receiving Idiopathic orthostatic hypotension (IOH), which was first chronic oral midodrine therapy required amwsthesia for coro- described in 1925, ~ manifests as postural hypotension, nary arter3., bypass grafting. A perioperative infusioo of phenyl- syncope, fixed heart rate, defective sweating, nocturia ephrine was substituted ,/'or midodrine, an alpha-2 agonist, and impotence. Urinary or faecal incontinence or consti- enabling hypotension resulting from low systemic vascular pation may also occur. Inappropriate cardiovascular resistance to be controlled easily. Anticipated adrenergic reflexes2 predispose to haemodynamic instability. Treat- receptor denert,ation hypersensitivi O, was noted. The only ment is symptomatic, and includes head-up body tilt at significant perioperative problem was one episode of ~Tncope night, elastic stockings, 9 o~-fludroconisone and mido- from orthostatic hypotension during the reambulation period. drine 3 (Gutron | - Chemie Linz AG, Linz, Austria), an oral oL-adrenergic agonist in use in Europe, but an Un patient atteint d'hypolension or/hostatique idiopathique investigational drug in North America. The anaesthetic recevant un traitement oral chronique tl la midodrine a requis management of patients with autonomic dysfunction has I'anesthe;sie pour pontage aortocoronarien. Une perfusion been described, 4-9 but this is the first report of a patient pEriop~ratoire de phEnyl~phrine fut substitude ti la midodrine, with IOH receiving chronic midodrine therapy undergo- un agoniste alpha 2, a permis ~ I'hypotension r~sultant d'une ing cardiac surgery. r~sistance vasculaire syst~mique basse d'e;tre contr~l(e facile- ment. -

View PDF Version
Green Chemistry View Article Online PAPER View Journal | View Issue Synthesis of pharmaceutical drugs from cardanol derived from cashew nut shell liquid†‡ Cite this: Green Chem., 2019, 21, 1043 Yiping Shi, Paul C. J. Kamer § and David J. Cole-Hamilton * Cardanol from cashew nut shell liquid extracted from cashew nut shells was successfully converted into various useful pharmaceutical drugs, such as norfenefrine, rac-phenylephrine, etilefrine and fenoprofene. 3-Vinylphenol, the key intermediate for the synthesis of these drugs, was synthesised from cardanol by ethenolysis to 3-non-8-enylphenol followed by isomerising ethenolysis. The metathesis reaction worked very well using DCM, but the greener solvent, 2-methyl tetrahydrofuran, also gave very similar results. Hydroxyamination of 3-vinylphenol with an iron porphyrin catalyst afforded norfenefrine in over 70% yield. Methylation and ethylation of norfenefrine afforded rac-phenylephrine and etilefrine respectively. A sequence of C–O coupling, isomerising metathesis and selective methoxycarbonylation afforded feno- profene in good yield. A comparison of the routes described in this paper with some standard literature Creative Commons Attribution 3.0 Unported Licence. syntheses of 3-vinylphenol and of the drug molecules shows significant environmental advantages in terms of precursors, yields, number of steps, conditions and the use of catalysts. The Atom Economy of our processes is generally similar or significantly superior to those of the literature processes mainly Received 7th December 2018, because the side products produced during synthesis of 3-vinylphenol (1-octeme, 1,4-cyclohexadiene Accepted 15th January 2019 and propene) are easily separable and of commercial value, especially as they are bio-derived. -

Medicines and Related Substances Act No. 101 of 1965
MEDICINES AND RELATED SUBSTANCES ACT NO. 101 OF 1965 [View Regulation] [ASSENTED TO 19 JUNE, 1965] [DATE OF COMMENCEMENT: 1 APRIL, 1966] (Afrikaans text signed by the State President) This Act was published in Government Gazette 40869 dated 26 May, 2017. as amended by Drugs Control Amendment Act, No. 29 of 1968 Drugs Control Amendment Act, No. 88 of 1970 Drugs Laws Amendment Act, No. 95 of 1971 Drugs Control Amendment Act, No. 65 of 1974 Medicines and Related Substances Control Amendment Act, No. 19 of 1976 Health Laws Amendment Act, No. 36 of 1977 Medicines and Related Substances Control Amendment Act, No. 17 of 1979 Medicines and Related Substances Control Amendment Act, No. 20 of 1981 Transfer of Powers and Duties of the State President Act, No. 97 of 1986 [with effect from 3 October, 1986] Businesses Act, No. 71 of 1991 [with effect from 24 May, 1991] Medicines and Related Substances Control Amendment Act, No. 94 of 1991 General Law Amendment Act, No. 49 of 1996 [with effect from 4 October, 1996] Abolition of Restrictions on the Jurisdiction of Courts Act, No. 88 of 1996 [with effect from 22 November, 1996] Medicines and Related Substances Control Amendment Act, No. 90 of 1997 Medicines and Related Substances Amendment Act, No. 59 of 2002 Judicial Matters Amendment Act, No. 66 of 2008 [with effect from 17 February, 2009] Medicines and Related Substances Amendment Act No. 72 of 2008 Medicines and Related Substances Amendment Act, No. 14 of 2015 GENERAL NOTE There is a discrepancy between the English and Afrikaans texts of section 1 of Act No. -
Postoperative Vasopressor Usage: a Prospective International Observational Study
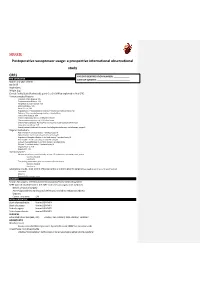
SQUEEZE Postoperative vasopressor usage: a prospective international observational study CRF1 PATIENT IDENTIFICATION NUMBER: _____________ PRE-OPERATIVE DATE OF SURGERY: ___________________________ Month and year of birth Sex [m/f] Height [cm] Weight [kg] Clinical Frailty Scale (Rockwood): point 0 to 9. (Will be explained in final CRF) Previous medical history: Coronary Artery Disease: Y/N Cerebrovascular Disease: Y/N Peripheral vascular disease: Y/N Atrial fibrillation: Y/N Heart failure: Y/N Hypertension: Y treated and controlled, Y treated but not controlled, No Diabetes: Takes insulin/managed without insulin/None Chronic liver disease: Y/N Chronic respiratory disease: COPD/other/None Chronic immunosuppression: HIV/other/none Chronic Kidney Disease: No/Yes/Yes and receives renal replacement therapy Long-term steroid use: Y/N Recent/current treatment for cancer (including chemotherapy, radiotherapy, surgery) Regular medications ACE inhibitor: Y and took today/ Y omitted today/N Alpha blocker: Y and took today/ Y omitted today/N Angiotensin Receptor Blocker: Y and took today/ Y omitted today/N Beta blocker: Y and took today/ Y omitted today/N Calcium channel blocker: Y and took today/ Y omitted today Diuretic: Y and took today/ Y omitted today/N Regular NSAIDs: Y/N Regular PPI: Y/N Haemodynamics Measurement in the past 6 months, at least 12h prior to the operating room, at rest: Systolic, Diastolic Heart rate The reading immediately prior to induction of anaesthesia: Systolic, Diastolic Heart rate Laboratory results, most recent (if known -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0