STARLIX (Nateglinide) Tablets, for Oral Use • Common Adverse Reactions Associated with STARLIX (3% Or Greater Initial U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetes Medications: Oral Medications
Diabetes Medications: Oral Medications Medication Types 1. Biguanides 2. Sulfonylureas 3. Thiazolidinediones (TZDs) 4. Alpha-Glucosidase Inhibitors 5. D-Phenylalanine Meglitinides 6. SGLT-2 inhibitors 7. DPP-4 inhibitors 8. Combination Oral Medications 1. Biguanides This works by lowering blood glucose by reducing the amount of glucose produced by the liver and helping the body respond better to the insulin made in the pancreas Metformin can be used with diet and exercise or with other agents, diet, and exercise. Types of Biguanides: • Metformin (Glucophage) 500mg/1000mg • Metformin (Glucophage XR) 500mg/1000mg • Fortamet (extended release) 500mg/1000mg • Riomet (oral solution) 500mg/5ml Side Effects: • Cramping • Gas • Diarrhea • Taking the pill before meals may decrease stomach upset 2. Sulfonylureas Sulfonylureas stimulate the pancreas to produce insulin and cause the body to respond better to the insulin it does produce. Sulfonylureas can be used alone or in combination with other medications. Types of Sulfonylureas: • Glimepiride (Amaryl) • Glipizide (Glucotrol, Glucotrol XL) • Glyburide (Diabeta, Micronase) • Glyburide, micronized (Glynase) • Tolbutamide (Orinase) 1st generation • Tolazamide (Tolinase) 1st generation • Acetohexamide (Dymelor) 1st generation • Chlorpropamide (Diabinese) 1st generation Side Effects: • Hypoglycemia • Upset stomach • Weight gain • Skin rash 3. Thiazolidinediones (TZDs) TZDs primarily reduce insulin resistance by improving target cell response (sensitivity) to insulin. They also can decrease glucose output from the liver and increase glucose disposal in the skeletal muscles. Types of TZDs: • Pioglitazione (Actos) 15-45 mg Actos may be taken with or without food • Avandia—off the market Side Effects: • Jaundice • Nausea and vomiting • Stomach pain • Dark urine • Swelling • These medicines are generally safe and do not cause hypoglycemia when used alone. -

Orange Book Patent Listing Dispute List
Patent Listing Disputes Current through September 10, 2021 Established Drug Product Due Date for NDA Holder NDA Holder NDA Number NDA Holder Strength(s) Relevant U.S. Patent Number(s) Type of Patent Claim Original Use Code (if applicable) Revised Use Code (if applicable) Dispute Outcome Name Response Response Date Disputes Not Related to epinephrine 205029 Belcher 1mg/mL 10,004,700 and 10,039,728 N/A N/A 7/24/2021 Pending Pending Use Code 7 mg 14 mg 8,168,209, 8,173,708, 8,283,379, Disputes Not Related to memantine hydrochloride 22525 Allergan Sales LLC N/A N/A 5/28/2021 5/28/2021 Patent Listing Updated 21 mg 8,329,752, 8,362,085 and 8,598,233 Use Code 28 mg 0.1 mg Disputes Not Related to epinephrine 201739 Kaleo Inc 0.15 mg 10,824,938 N/A N/A 2/28/2021 2/3/2021 Patent Listing Updated Use Code 0.3 mg Disputes Not Related to netarsudil and latanoprost 208259 Aerie Pharms Inc 0.02%/0.005% 10,654,844 N/A N/A 11/18/2020 10/30/2020 Patent Listing Updated Use Code Disputes Not Related to netarsudil 208254 Aerie Pharms Inc 0.02% 10,654,844 N/A N/A 11/18/2020 10/30/2020 Patent Listing Updated Use Code U-2869: IV Administration of cangrelor before U-2979: Method comprising IV administration PCI and continuous infusion for at least 2 of cangrelor before PCI then continuous hours or the duration of the PCI and, during infusion for at least 2 hours or the duration of cangrelor 204958 Chiesi 50 mg/vial 8,680,052 Method of Use 11/8/2020 11/3/2020 Patent Listing Updated or after the continuous infusion, PCI and, during or after continuous infusion, -

Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly with Insulin Secretagogues
Research Letter | Diabetes and Endocrinology Association Between Serious Hypoglycemia and Calcium-Channel Blockers Used Concomitantly With Insulin Secretagogues Young Hee Nam, PhD; Colleen M. Brensinger, MS; Warren B. Bilker, PhD; James H. Flory, MD; Charles E. Leonard, MSCE, PharmD; Sean Hennessy, PhD, PharmD Introduction + Supplemental content Serious hypoglycemia is a major, potentially fatal adverse event caused by insulin secretagogues.1 Author affiliations and article information are Previous case reports suggested that calcium-channel blockers (CCBs) might reduce the risk of listed at the end of this article. serious hypoglycemia in patients with hyperinsulinemic hypoglycemia.2,3 However, the association of serious hypoglycemia and CCBs used with insulin secretagogues has remained unclear. Because insulin secretion by the pancreas is mediated by calcium influx in beta cells through calcium channels,4 we conducted a population-based observational study on the hypothesis that concomitant use of CCBs may be associated with reduced rates of serious hypoglycemia in insulin secretagogue users. Methods This self-controlled case series study was approved by the institutional review board of the University of Pennsylvania, which waived the requirement for informed consent because the use or disclosure of the protected health information involved no more than minimal risk to the privacy of individuals, and the research could not practicably be conducted without the waiver or alteration and without access to and use of the protected health information. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. We used claims data from the Medicaid programs of 5 US states (California, Florida, New York, Ohio, and Pennsylvania, encompassing more than a third of the nationwide Medicaid population), supplemented with Medicare claims for dual enrollees, from January 1, 1999, to December 31, 2011, and used the self- controlled case series design. -

Oregon Drug Use Review / Pharmacy & Therapeutics Committee
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program OHA Division of Medical Assistance Programs 500 Summer Street NE, E35; Salem, OR 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Oregon Drug Use Review / Pharmacy & Therapeutics Committee Thursday, July 26, 2018 1:00 - 5:00 PM HP Conference Room 4070 27th Ct. SE Salem, OR 97302 MEETING AGENDA NOTE: Any agenda items discussed by the DUR/P&T Committee may result in changes to utilization control recommendations to the OHA. Timing, sequence and inclusion of agenda items presented to the Committee may change at the discretion of the OHA, P&T Committee and staff. The DUR/P&T Committee functions as the Rules Advisory Committee to the Oregon Health Plan for adoption into Oregon Administrative Rules 410-121-0030 & 410-121-0040 as required by 414.325(9). I. CALL TO ORDER 1:00 PM A. Roll Call & Introductions R. Citron (OSU) B. Conflict of Interest Declaration R. Citron (OSU) C. Approval of Agenda and Minutes T. Klein (Chair) D. Department Update T. Douglass (OHA) E. Legislative Update T. Douglass (OHA) F. Mental Health Clinical Advisory Group Discussion K. Shirley (MHCAG) 1:40 PM II. CONSENT AGENDA TOPICS T. Klein (Chair) A. P&T Methods B. CMS and State Annual Reports C. Quarterly Utilization Reports 1. Public Comment III. DUR ACTIVITIES 1:45 PM A. ProDUR Report R. Holsapple (DXC) B. RetroDUR Report D. Engen (OSU) C. Oregon State Drug Reviews K. Sentena (OSU) 1. A Review of Implications of FDA Expedited Approval Pathways, Including the Breakthrough Therapy Designation IV. -

Download Product Insert (PDF)
PRODUCT INFORMATION Nateglinide Item No. 23320 CAS Registry No.: 105816-04-4 Formal Name: N-[[trans-4-(1-methylethyl)cyclohexyl] O OH carbonyl]-D-phenylalanine Synonyms: A-4166, SDZ-DJN 608 O MF: C H NO 19 27 3 N FW: 317.4 Purity: ≥98% H UV/Vis.: λmax: 207 nm Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Nateglinide is supplied as a crystalline solid. A stock solution may be made by dissolving the nateglinide in the solvent of choice. Nateglinide is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide, which should be purged with an inert gas. The solubility of nateglinide in these solvents is approximately 30 mg/ml. Description Nateglinide is a hypoglycemic agent.1-3 It induces insulin and somatostatin release from perfused rat pancreas when used at concentrations ranging from 0.03 to 3 μM.1 Nateglinide (3 µM) increases intracellular calcium levels in isolated rat pancreatic β cells, an effect that can be inhibited by the L-type calcium channel blocker nitrendipine (Item No. 17549). Nateglinide-induced secretion of insulin and somatostatin and calcium influx is also reversed by the potassium channel activator diazoxide (Item No. 14576). Oral administration of nateglinide (1.6 mg/kg) reduces blood glucose levels by 20% in fasted mice.2 It also decreases blood glucose levels in an oral glucose tolerance test in normal rats, genetically diabetic KK mice, and a rat model of diabetes induced by streptozotocin (STZ; Item No. -

Ambetter 90-Day-Maintenance Drug List- 2020
Ambetter 90-Day-Maintenance Drug List Guide to this list: What is Ambetter 90‐Day‐Maintenance Drug List? Ambetter 90‐Day‐Supply Maintenance Drug List is a list of maintenance medications that are available for 90 day supply through mail order or through our Extended Day Supply Network. How do I find a pharmacy that is participating in Extended Day Supply Network? To find a retail pharmacy that is participating in our Extended Day Supply Network please consult information available under Pharmacy Resources tab on our webpage. Alternatively, you can utilize our mail order pharmacy. Information on mail order pharmacy is available in Pharmacy Resources tab on our webpage. Are all formulary drugs covered for 90 day supply? No, certain specialty and non‐specialty drugs are excluded from 90 day supply. Please consult 90‐Day‐ Supply Maintenance Drug List for information if your drug is included. A Amitriptyline HCl Acamprosate Calcium Amlodipine Besylate Acarbose Amlodipine Besylate-Atorvastatin Calcium Acebutolol HCl Amlodipine Besylate-Benazepril HCl Acetazolamide Amlodipine Besylate-Olmesartan Medoxomil Albuterol Sulfate Amlodipine Besylate-Valsartan Alendronate Sodium Amlodipine-Valsartan-Hydrochlorothiazide Alendronate Sodium-Cholecalciferol Amoxapine Alfuzosin HCl Amphetamine-Dextroamphetamine Aliskiren Fumarate Anagrelide HCl Allopurinol Anastrozole Alogliptin Benzoate Apixaban Alosetron HCl Arformoterol Tartrate Amantadine HCl Aripiprazole Amiloride & Hydrochlorothiazide Armodafinil Amiloride HCl Asenapine Maleate Amiodarone HCl Aspirin-Dipyridamole -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Medications Used to Treat Type 2 Diabetes
Medications Used to Treat Type 2 Diabetes This handout shows the different medications that your healthcare provider may prescribe to treat your type 2 diabetes, and where and how these medications work in your body to lower blood glucose. Type 2 diabetes medications are taken orally (by mouth), by injection (inserted into the fat under your skin), or inhaled (breathed in). Oral Injectable Alpha-glucosidase inhibitors (acarbose, miglitol) Amylin mimetic (pramlintide) Help to slow down the breakdown of starches (such Helps to decrease the amount of glucose made by your liver. as bread and potatoes) and certain types of sugar (such as table sugar) from your food in your intestines: Helps to slow down the breakdown of foods in your stomach this slows down increases in blood glucose. and intestines: this slows down increases in blood glucose Biguanide (metformin) GLP-1 receptor agonists (albiglutide, dulaglutide, exenatide, liraglutide) Helps to decrease the amount of glucose made by your liver Help your pancreas to make more insulin: insulin helps to lower blood glucose Helps to improve the way that insulin works in your Help to decrease the amount of glucose made by your muscles: if your muscles are more sensitive to insulin, it liver is easier for insulin to bring glucose from your blood into Helps to slow down the breakdown of foods in your muscles where glucose can be used for energy your stomach and intestines: this slows down increases in blood glucose DPP-4 inhibitors (alogliptin, linagliptin, saxagliptin, sitagliptin) Fat Tissue -
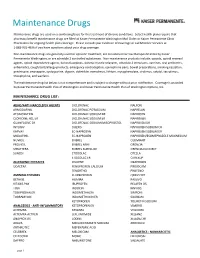
Maintenance Drug List Below Is Not Comprehensive and Is Subject to Change Without Prior Notification
Maintenance Drugs Maintenance drugs are used on a continuing basis for the treatment of chronic conditions. Select health plans require that pharmacy benefit maintenance drugs are filled at Kaiser Permanente Washington Mail Order or Kaiser Permanente Clinic Pharmacies for ongoing health plan coverage. Please consult your Evidence of Coverage or call Member Services at 1-888-901-4636 if you have questions about your drug coverage. Non-maintenance drugs are generally used for episodic treatment, are considered narrow therapeutic index by Kaiser Permanente Washington, or are schedule 2 controlled substances. Non-maintenance products include: opioids, opioid reversal agents, opioid dependence agents, benzodiazepines, skeletal muscle relaxants, schedule 2 stimulants, vaccines, oral antibiotics, antiemetics, cough/cold/allergy products, emergency contraception, epinephrine pens, bowel preparations, smoking cessation, prednisone, enoxaparin, cyclosporine, digoxin, dofetilide, everolimus, lithium, mycophenolate, sirolimus, sotalol, tacrolimus, theophylline, and warfarin. The maintenance drug list below is not comprehensive and is subject to change without prior notification. Coverage is provided by Kaiser Permanente Health Plan of Washington and Kaiser Permanente Health Plan of Washington Options, Inc. MAINTENANCE DRUG LIST: ADHD/ANTI-NARCOLEPSY AGENTS DICLOFENAC NALFON ARMODAFINIL DICLOFENAC POTASSIUM NAPRELAN ATOMOXETINE DICLOFENAC SODIUM DR NAPROSYN CLONIDINE HCL ER DICLOFENAC SODIUM ER NAPROXEN GUANFACINE ER DICLOFENAC SODIUM/MISOPROSTOL NAPROXEN -

The Role of Nateglinide and Repaglinide, Derivatives of Meglitinide, in the Treatment of Type 2 Diabetes Mellitus
State of the art paper The role of nateglinide and repaglinide, derivatives of meglitinide, in the treatment of type 2 diabetes mellitus Rodolfo Guardado-Mendoza 1, Annamaria Prioletta 2 , Lilia M. Jiménez-Ceja 1, Aravind Sosale 3, Franco Folli 4 1Department of Medicine and Nutrition, Division of Health Sciences, University Corresponding author: of Guanajuato, México Franco Folli MD, PhD 2Diabetes Center, ACISMOM Associazione Cavalieri Italiani Sovrano Militare Ordine University of Texas Health Di Malta, Italy Science Center 3Diacon Hospital, Bangalore, India Department of Medicine 4Department of Medicine, Diabetes Division, University of Texas Health Science Center Diabetes Division at San Antonio, Texas, USA Mail Stop 7886–7703 Floyd Curl Drive-San Antonio Submitted: 13 November 2012 TX 78229-3900, USA Accepted: 31 January 2013 Phone: 210-567-4826. E-mail: [email protected] Arch Med Sci 2013; 9, 5: 936–943 DOI: 10.5114/aoms.2013.34991 Copyright © 2013 Termedia & Banach Abstract Type 2 diabetes mellitus (T2DM) is one of the most common chronic diseases worldwide, presenting a great challenge to the public health systems due to high morbidity and mortality, because of frequent micro-/macro-vascular com - plications. Many treatment options are now available, with different efficacy as well as mechanisms of action to improve deranged glucose metabolism. We review some of the available data on derivatives of meglitinide, namely nateglin - ide and repaglinide. These two compounds increase insulin secretion by a mech - anism similar to the one of sulfonylureas, but with a shorter half-life. Nateglinide and repaglinide, derivatives of meglitinides, have characteristic pharmacody - namic and pharmacokinetic properties that, together with their proposed mech - anism of action, make them useful for type 2 diabetes mellitus, especially when used in combination therapy. -

Starlix, INN-Nateglinide
SCIENTIFIC DISCUSSION This module reflects the initial scientific discussion for the approval of Starlix. This scientific discussion has been updated until 1 February 2004. For information on changes after this date please refer to module 8B. 1. Introduction Starlix (nateglininde) is indicated for combination therapy with metformin of type 2 diabetes patients inadequately controlled despite a maximally tolerated dose of metformin alone. The daily dose is 60- 180 mg daily. Nateglinide is an aminoacid derivative of phenylalanine. Nateglinide is not structurally related to sulphonylureas. However, the mechanism of action is similar: nateglinide is an insulin secretagogue, decreasing blood glucose levels. 2. Chemical, pharmaceutical and biological aspects Composition Starlix film-coated tablets are available in 60 mg, 120 mg and 180 mg strengths containing nateglinide INN as the active substance. In addition to the active substance, the film-coated tablets contain standard excipients that are commonly used in solid oral dosage forms, chiefly lactose and microcrystalline cellulose. The remaining core ingredients are croscarmellose sodium, povidone and magnesium stearate. The primary packaging consists of a thermoformed blister using rigid plastic films, PVC/PE/PVDC backed with a heat-sealable lacquered aluminium foil: thermolacquer/aluminium/external protective coating. Active substance Nateglinide is N-(trans-4-Isopropylcyclohexanecarbonyl)-D-phenylalanine, a chiral molecule which has no structural resemblance to other antidiabetic drugs. It is manufactured by a third party and information was supplied in the form of an open and closed DMF. The process validation and investigation of potential critical parameters was satisfactory to assure a consistent good quality and purity of the active substance. -

ACCEPTABLE COMBINATIONS of DIABETES MEDICATIONS (Updated 01/27/2021)
ACCEPTABLE COMBINATIONS OF DIABETES MEDICATIONS (Updated 01/27/2021) The chart on the following page outlines acceptable combinations of medications for treatment of diabetes. Please note: • Initial certification of all applicants with diabetes mellitus (DM) requires FAA decision; • Use no more than one medication from each group (A-F); • Fixed-dose combination medications - count each component as an individual medication. (e.g., Avandamet [rosiglitazone + metformin] is considered 2-drug components); • Up to 3 medications total are considered acceptable for routine treatment according to generally accepted standards of care for diabetes (American Diabetes Association, American Association of Clinical Endocrinologists); • For applicants receiving complex care (e.g., 4-drug therapy), refer the case to AMCD; • For applicants on AASI for diabetes mellitus, follow the AASI; • Consult with FAA for any medications not on listed on the chart; • Observation times: When initiating NEW diabetes therapy using monotherapy or combination medications: Adding Medication Observation Time Group A ONLY 14 days Group B-D 30 days Group E1 60 days When ADDING a new medication to an ESTABLISHED TREATMENT regimen: Current Medication Adding Medication Observation Time on Group A-D + new Group A-D 14 days on Group E1 + new Group A-D 30 days on Group A-D + new Group E1 60 days Note: If transitioning between injectable GLP-1 RA and oral GLP-1 RA formulation = 72 hours When initiating NEW or ADDING therapy for any regimen (new or established therapy): Adding Medication Observation Time Group F (SGLT2 inhibitors) 90 days Group E2 (insulin): • For agency ATCSs (non-CGM or CGM protocol) 90 days • For Pilots / Part 67 applicants, class 3 non-CGM 90 days protocol only: 180 days • For Pilots / Part 67 applicants, any class CGM protocol: ACCEPTABLE COMBINATIONS OF DIABETES MEDICATIONS (Updated 01/27/2021) Biguanides A -metformin (e.g.