An Investigation Into the Effects and Possible
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Complete Dissertation
VU Research Portal Histamine H-receptor agonists and antagonists ter Laak, A.M. 1995 document version Publisher's PDF, also known as Version of record Link to publication in VU Research Portal citation for published version (APA) ter Laak, A. M. (1995). Histamine H-receptor agonists and antagonists: molecular modeling and drug design. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ? Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. E-mail address: [email protected] Download date: 06. Oct. 2021 Histamine H1~receptor Agonists and Antagonists Molecular Modeling and Drug Design , Ton tel' Laak Histamine HI-receptor Agonists and Antagonists Molecular Modeling and Drug Design VRIJE UNIVERSlTEIT Histamine HI-receptor Agonists and Antagonists Molecular Modeling and Drug Design ACADEMISCH PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Vrije Universiteit te Amsterdam, op gezag van de rector magnificus prof.dr E. Boeker, in het openbaar te verdedigen ten overstaan van de promotiecommissie van de faculteit der scheikunde op maandag 16 oktober 1995 te 13.45 uur in het hoofdgebouw van de universiteit, De Boelelaan 1105 door Antonius Marinus ter Laak geboren te Delft Promotor prof.dr H. -

Drug-Induced Sexual Dysfunction in Men and Women
VOLUME 36 : NUMBER 2 : APRIL 2013 ARTICLE Drug-induced sexual dysfunction in men and women Helen M Conaglen whether the clinician is willing to ask about sexual Clinical psychologist and SUMMARY issues and does so in a sensitive way.7,8 Senior research fellow Many medical conditions and their treatments Patients on long-term medications may not be John V Conaglen aware that their sexual problems have developed Endocrinologist and contribute to sexual dysfunction. as a result of their treatment. Conversely some may Associate professor in Commonly implicated drugs include Medicine blame their drugs for sexual problems which are due Sexual Health Research Unit antihypertensives, antidepressants, to relationship difficulties or other stressors. Some Waikato Clinical School antipsychotics and antiandrogens. doctors consider that asking patients if they had Faculty of Medical and Understanding the potential for drug-induced noticed any sexual adverse effects from their drugs Health Sciences University of Auckland sexual problems and their negative impact may ‘suggest’ them to the patient, and possibly result on adherence to treatment will enable the in non-adherence. Patients attributing their sexual clinician to tailor treatments for the patient problems to their drugs are less likely to continue the Key words treatment even when necessary for their health.9 The antidepressants, and his or her partner. consultation should include discussion of the patient’s antihypertensives, Encouraging a discussion with the patient sexual issues so these can be considered in treatment antipsychotics, arousal, about sexual function and providing erectile dysfunction, decisions. hypoactive sexual desire strategies to manage the problem are critical disorder, male impotence, to good clinical care. -

Dative Metabolism of Cortisol in Humans Kunihi
臨 床 薬 理JPn J Clin Pharmacol Ther 18 (3) Sept 1987 509 Comparison of the Inhibitory Effects of Famotidine and Cimetidine on Hepatic Oxi- dative Metabolism of Cortisol in Humans Kunihiko MORITA* Hiroki KONISHI* Takeshi ONO* and Harumi SHIMAKAWA* (Receivedon Dec.19, 1986) * Hospital Pharmacy, Shiga Universityof Medical Science, Tsukinowa-cho,Seta, Ohtsu520-21, Japan The inhibitory effect of famotidine, a new H2-receptor antagonist, on hepatic oxidative metabolism of cortisol in six healthy volunteers was compared with that of cimetidine by monitoring the change in urinary 6ƒÀ-hydroxycortisol (6ƒÀ-OHF), an oxidative metabolite of cortisol. The ratio of 6ƒÀ-OHF to 17-hydroxycorticosteroids (17-OHCS) in urine was measured before, during, and after treatment with famotidine and cimetidine for 3 days in a cross-over study. The ratio was decreased by 25% -35% of the original level after 1-3 days of oral treatment with cimetidine (800 mg, b. i. d.). The reduction vanished within 2 days after the last dose of cimetidine. The ratio was not significantly changed during oral treatment with famotidine (40 mg, b. i. d.). These findings indicate that famotidine, in contrast to cimetidine, does not affect the hepatic oxidative metabolism of cortisol in man, and it is suggested that famotidine does not affect the hepatic drug-metabolizing capacity in humans. Key words: famotidine, cimetidine, H2-receptor antangonist, 6ƒÀ-hydroxycortisol, enzyme inhibition been shown to inhibit the hepatic elimination of a Introduction number of drugs coadministred.1-4) A number of Cimetidine, a histamine H2-receptor antagonist studies have demonstrated that this inhibitory widely used for the treatment of peptic ulcer, has action of cimetidine is based on its high affinity for cytochrome P-450 in hepatic microsomes *滋 賀医科大学医学部附属病院薬剤部 arising from imidazole and cyano groups.5-7) 〓520-21滋 賀県大津市瀬田月輪町 Ranitidine, an H2-receptor antagonist developed 510 hospital pharmacists, aged 24 to 35 years old (mean 28), participated in the study. -
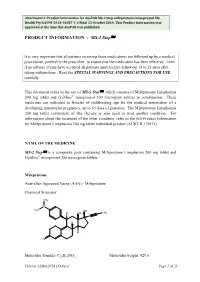
Auspar Attachment 1. Product Information for Mifepristone
Attachment 1: Product information for AusPAR MS-2 Step mifepristone/misoprostol MS Health Pty Ltd PM-2013-01037-1-5 Final 13 October 2014. This Product Information was approved at the time this AusPAR was published. PRODUCT INFORMATION - MS-2 StepÔ It is very important that all patients receiving these medications are followed up by a medical practitioner, preferably the prescriber, to ensure that the medication has been effective. Even if no adverse events have occurred all patients must receive follow-up 14 to 21 days after taking mifepristone. Read the SPECIAL WARNINGS AND PRECAUTIONS FOR USE carefully. This document refers to the use of MS-2 StepÔ, which consists of Mifepristone Linepharma 200 mg tablet and GyMiso® misoprostol 200 microgram tablets in combination. These medicines are indicated in females of childbearing age for the medical termination of a developing intrauterine pregnancy, up to 63 days of gestation. The Mifepristone Linepharma 200 mg tablet component of this therapy is also used to treat another condition. For information about the treatment of the other condition, refer to the full Product Information for Mifepristone Linepharma 200 mg tablet individual product (AUST R 175671). NAME OF THE MEDICINE MS-2 StepÔ is a composite pack containing Mifepristone Linepharma 200 mg tablet and GyMiso® misoprostol 200 microgram tablets. Mifepristone Australian Approved Name (AAN): Mifepristone Chemical Structure: CH3 N CH 3 OH CH H CH3 3 H H O Molecular formula: C29H35NO2 Molecular weight: 429.6 Version:22May2014 [63days] Page 1 of 23 Attachment 1: Product information for AusPAR MS-2 Step mifepristone/misoprostol MS Health Pty Ltd PM-2013-01037-1-5 Final 13 October 2014. -

Clinical Pharmacological Studies with a New H2-Receptor Antagonist
Gut: first published as 10.1136/gut.23.2.157 on 1 February 1982. Downloaded from Gut, 1982, 23, 157-163 Oxmetidine: clinical pharmacological studies with a new H2-receptor antagonist JANE G MILLS, P L BRUNET, R GRIFFITHS, R H HUNT, DIANA VINCENT, G J MILTON-THOMPSON, AND W L BURLAND From the Research Institute, Smith Kline and French Research 4td, Welwyn Garden City, Herts, and The Royal Naval Hospital, Haslar, Hampshire SUMMARY The gastric antisecretory effects ofoxmetidine, a new H2-receptor antagonist, have been studied in 33 healthy subjects. The relative potency of oxmetidine compared with that of cimetidine depended on the route ofadministration and the experimental conditions. Oxmetidine intravenously infused was approximately four times as potent as cimetidine, weight for weight, in inhibiting impromidine stimulated gastric acid secretion but was twice as potent when food was used as a stimulus. After oral administration there were no differences in the weight-for-weight potency of oxmetidine and cimetidine, although oxmetidine was twice as potent on a molar basis. These apparent differences according to the route of drug administration are probably due to first pass metabolism of oxmetidine There were no differences in the duration of action of oxmetidine and cimetidine. Twenty-four hour monitoring of intragastric pH showed that oxmetidine 400 mg twice daily reduced mean hourly 24 hour intragastric pH by 59%, suggesting that a twice daily dosage regimen should be evaluated in the treatment of duodenal ulceration. http://gut.bmj.com/ Oxmetidine dihydrochloride (Fig. 1) is an example showing variation with respect to route of of a new type of H2-receptor antagonist which is administration and species studied. -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -

The Organic Chemistry of Drug Synthesis
THE ORGANIC CHEMISTRY OF DRUG SYNTHESIS VOLUME 3 DANIEL LEDNICER Analytical Bio-Chemistry Laboratories, Inc. Columbia, Missouri LESTER A. MITSCHER The University of Kansas School of Pharmacy Department of Medicinal Chemistry Lawrence, Kansas A WILEY-INTERSCIENCE PUBLICATION JOHN WILEY AND SONS New York • Chlchester • Brisbane * Toronto • Singapore Copyright © 1984 by John Wiley & Sons, Inc. All rights reserved. Published simultaneously in Canada. Reproduction or translation of any part of this work beyond that permitted by Section 107 or 108 of the 1976 United States Copyright Act without the permission of the copyright owner is unlawful. Requests for permission or further information should be addressed to the Permissions Department, John Wiley & Sons, Inc. Library of Congress Cataloging In Publication Data: (Revised for volume 3) Lednicer, Daniel, 1929- The organic chemistry of drug synthesis. "A Wiley-lnterscience publication." Includes bibliographical references and index. 1. Chemistry, Pharmaceutical. 2. Drugs. 3. Chemistry, Organic—Synthesis. I. Mitscher, Lester A., joint author. II. Title. [DNLM 1. Chemistry, Organic. 2. Chemistry, Pharmaceutical. 3. Drugs—Chemical synthesis. QV 744 L473o 1977] RS403.L38 615M9 76-28387 ISBN 0-471-09250-9 (v. 3) Printed in the United States of America 10 907654321 With great pleasure we dedicate this book, too, to our wives, Beryle and Betty. The great tragedy of Science is the slaying of a beautiful hypothesis by an ugly fact. Thomas H. Huxley, "Biogenesis and Abiogenisis" Preface Ihe first volume in this series represented the launching of a trial balloon on the part of the authors. In the first place, wo were not entirely convinced that contemporary medicinal (hemistry could in fact be organized coherently on the basis of organic chemistry. -

Cimetidine Tablets 200Mg, 400Mg and 800Mg
PACKAGE LEAFLET: INFORMATION FOR THE USER Cimetidine Tablets 200mg, 400mg and 800mg [Cimetidine] Read all of this leaflet carefully before you start ! Are taking other medicines (see Section 'Other taking this medicine because it contains medicines and Cimetidine Tablets '). important information for you. ! Keep this leaflet. You may need to read it again. Other medicines and Cimetidine Tablets ! If you have any further questions, ask your doctor or pharmacist or nurse. Tell your doctor or pharmacist if you are taking, have ! This medicine has been prescribed for you only. recently taken or might take any other medicines. Do not pass it on to others. It may harm them, In particular tell your doctor if you are taking any of even if their signs of illness are the same as the following: yours. ! Anticoagulants to thin your blood e.g. warfarin ! If you get any side effects, talk to your doctor, or ! Anticonvulsants to prevent fits e.g. phenytoin pharmacist or nurse. This includes any possible ! Bronchodilators for breathing difficulties e.g. side effects not listed in this leaflet. See section 4. theophylline ! Anti-arrhythmics to slow heart rate e.g. lidocaine, What is in this leaflet: propranolol 1. What Cimetidine Tablets are and what they ! Antidepressants to treat anxiety e.g. diazepam are used for ! Immunosuppresants to prevent organ rejection 2. What you need to know before you take or rheumatism (e.g. ciclosporin) Cimetidine Tablets ! Medicines that cause a fall in blood cell count 3. How to take Cimetidine Tablets ! Antifungals used to treat fungal infections (e.g. 4. -

(12) United States Patent (10) Patent No.: US 9,040,685 B2 Buchanan Et Al
USOO904O685B2 (12) United States Patent (10) Patent No.: US 9,040,685 B2 Buchanan et al. (45) Date of Patent: May 26, 2015 (54) CELLULOSE INTERPOLYMERS AND (2013.01); A61 K9/4891 (2013.01); A61 K METHOD OF OXDATION 47/38 (2013.01); C08B3/04 (2013.01); C08B 3/16 (2013.01); C08B3/22 (2013.01); C08B (71) Applicant: Eastman Chemical Company, 3/24 (2013.01); C08L 1/10 (2013.01); C08L Kingsport, TN (US) I/I2 (2013.01); C08L 1/14 (2013.01); C09D 17/00 (2013.01); C08B 15/02 (2013.01); C08B (72) Inventors: Charles Michael Buchanan, Bluff City, I5/04 (2013.01); C08B 3/08 (2013.01); A61 K TN (US); Norma Lindsey Buchanan, 9/19 (2013.01); A61 K9/2866 (2013.01) Bluff City, TN (US); Susan Northrop (58) Field of Classification Search Carty, Kingsport, TN (US); CPC ......................................................... CO8E33A16 Chung-Ming Kuo, Kingsport, TN (US); USPC ...................................................... 536/64, 65 Juanelle Little Lambert, Gray, TN See application file for complete search history. (US); Michael Orlando Malcolm, Kingsport, TN (US); Jessica Dee Posey-Dowty, Kingsport, TN (US); (56) References Cited Thelma Lee Watterson, Kingsport, TN (US); Matthew Davie Wood, Gray, TN U.S. PATENT DOCUMENTS (US); Margaretha Soderqvist 2,363,091 A 11/1944 Seymour et al. Lindblad, Vallentuna (SE) 2,758,111 A 8, 1956 Roth 3,414,640 A 12, 1968 Garetto et al. .................. 264/13 (73) Assignee: EASTMAN CHEMICAL COMPANY., 3,489,743 A 1/1970 Crane Kingsport, TN (US) 3,845,770 A 11/1974 Theeuwes et al. 3,859,228 A 1/1975 Morishita et al. -

Complete Inhibition of Food-Stimulated Gastric Acid Secretion by Combined Application of Pirenzepine and Ranitidine*
Gut: first published as 10.1136/gut.22.7.542 on 1 July 1981. Downloaded from Gut, 1981, 22, 542-548 Complete inhibition of food-stimulated gastric acid secretion by combined application of pirenzepine and ranitidine* W LONDONG,t V LONDONG, C RUTHE, AND P WEIZERT From the Medizinische Klinik Innenstadt, University ofMunich, Munich, W Germany SUMMARY In a double-blind, placebo controlled and randomised secretory study the effectiveness of pirenzepine, ranitidine, and their combination was compared intraindividually in eight healthy subjects receiving intravenous bolus injections. Pirenzepine (0.15 mg/kg) plus ranitidine (0-6 mg/kg) suppressed peptone-stimulated gastric acid secretion from 69±11 to 2±0-4 mmol H+/3 h; the mean percentage inhibition was 97%. Postprandial gastrin was unaffected. There were only minor side-effects in a few experiments (reduction of salivation, brief blurring of vision), but no prolactin stimulation after ranitidine or ranitidine plus pirenzepine. The combined application of ranitidine and pirenzepine inhibited meal-stimulated acid secretion more effectively and produced fewer side-effects than the combination of cimetidine plus pirenzepine studied previously. The combined application ofclassical anticholinergics Methods and H2-receptor antagonists inhibits basal and http://gut.bmj.com/ stimulated gastric acid secretion in man more than Each subject had four tests which had to be carried either drug alone.' In double-blind, placebo con- out within a fortnight; the interval between two tests trolled and randomised investigations we have was at least three days. On separate days each subject demonstrated79 that combined intravenous bolus received pirenzepine, ranitidine, pirenzepine plus injections ofthe antimuscarinic drug pirenzepine with ranitidine, and placebo in random order by slow cimetidine suppressed peptone-stimulated acid out- intravenous bolus on a double-blind basis according put more effectively (on average by 90%) than either to a predetermined randomisation code. -

These Highlights Do Not Include All the Information Needed to Use PRASTERA® Safely and Effectively
PRASTERA- prasterone and ibuprofen Health Science Funding, LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use PRASTERA® safely and effectively. See full prescribing information for PRASTERA® . PRASTERA® prasterone oral softgels 200mg are for oral use only. Initial U.S. Approval INDICATIONS AND USAGE PRASTERA® prasterone 200 mg oral softgels is indicated in female patients with mild to moderate, active (SLEDAI ≥2) systemic lupus erythematosus (SLE) to restore serum 5-dehydroandrosterone sulfate to levels typical of women without SLE. In Phase III clinical trials in female patients with mild to moderate active SLE, prasterone 200 mg was associated with reduced risk of auto-immune flare, reduced risk of breast cancer and reduced risk of death from any cause. (§§1, 6.2, 6.4, 6.5) DOSAGE AND ADMINISTRATION The recommended dose is one (1) softgel daily. (§2) DOSAGE FORMS AND STRENGTHS 200mg oral softgel capsules supplied in a convenience package with ibuprofen oral tablets 400mg. (§3) CONTRAINDICATIONS Known hypersensitivity to any of its ingredients. (§4) Undiagnosed abnormal genital bleeding. (§4) Known, suspected or history of breast cancer. (§4, §6.5) History of, or known, deep vein thrombosis, pulmonary embolism, arterial thromboembolic disease (e.g., stroke, myocardial infarction). (§4) Hypercholesterolemia or ischemic heart disease. (§4, §7.2.4) Hepatic or renal impairment (pharmacokinetic data lacking). (§4, §7.2) Breast-feeding or known or suspected pregnancy. -

(12) Patent Application Publication (10) Pub. No.: US 2002/0102215 A1 100 Ol
US 2002O102215A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2002/0102215 A1 Klaveness et al. (43) Pub. Date: Aug. 1, 2002 (54) DIAGNOSTIC/THERAPEUTICAGENTS (60) Provisional application No. 60/049.264, filed on Jun. 6, 1997. Provisional application No. 60/049,265, filed (75) Inventors: Jo Klaveness, Oslo (NO); Pal on Jun. 6, 1997. Provisional application No. 60/049, Rongved, Oslo (NO); Anders Hogset, 268, filed on Jun. 7, 1997. Oslo (NO); Helge Tolleshaug, Oslo (NO); Anne Naevestad, Oslo (NO); (30) Foreign Application Priority Data Halldis Hellebust, Oslo (NO); Lars Hoff, Oslo (NO); Alan Cuthbertson, Oct. 28, 1996 (GB)......................................... 9622.366.4 Oslo (NO); Dagfinn Lovhaug, Oslo Oct. 28, 1996 (GB). ... 96223672 (NO); Magne Solbakken, Oslo (NO) Oct. 28, 1996 (GB). 9622368.0 Jan. 15, 1997 (GB). ... 97OO699.3 Correspondence Address: Apr. 24, 1997 (GB). ... 9708265.5 BACON & THOMAS, PLLC Jun. 6, 1997 (GB). ... 9711842.6 4th Floor Jun. 6, 1997 (GB)......................................... 97.11846.7 625 Slaters Lane Alexandria, VA 22314-1176 (US) Publication Classification (73) Assignee: NYCOMED IMAGING AS (51) Int. Cl." .......................... A61K 49/00; A61K 48/00 (52) U.S. Cl. ............................................. 424/9.52; 514/44 (21) Appl. No.: 09/765,614 (22) Filed: Jan. 22, 2001 (57) ABSTRACT Related U.S. Application Data Targetable diagnostic and/or therapeutically active agents, (63) Continuation of application No. 08/960,054, filed on e.g. ultrasound contrast agents, having reporters comprising Oct. 29, 1997, now patented, which is a continuation gas-filled microbubbles stabilized by monolayers of film in-part of application No. 08/958,993, filed on Oct.