Shoulder Instability and Labral Tears
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SLAP Repairs Versus Biceps Tenodesis in Athletes 15 Min Power Points
SLAP Repairs Versus Biceps Tenodesis in Athletes 15 min Power Points • Not all SLAP tears need surgery • Preservation of Native Anatomy GOAL • Not all labral repairs are equal • Kinetic chain MUST be addressed Power Points • Biceps DOES have a function • Tenodesis has consequences • Tenodesis relieves pain reliably BUT……long term effects uncertain ‘SLAPAHOLIC’ T. Romeo • One who fixes EVERY SLAP TEAR and anything that remotely looks like one! Not all SLAP Tears Need Surgery • SLAP tears way overdiagnosed • Beware of positive imaging study - negative exam • Slight labral separation may allow thrower to ‘get the slot’ MRI May OVERDIAGNOSE • Specificity ranges from 63% to 91% MRI and Anatomic Variants • Meniscoid labrum • Buford complex • Cord like MGHL • Age related attritional tear • ALL CAN LOOK LIKE SLAP TEARS ON MRI!! Meniscoid Labrum ‘Buford’ Complex Labral Tears are Part of the Aging Process! Pfahler et al JSES 2003 MANY LABRAL TEARS RESPOND TO REHAB!!!! Nonoperative Treatment of Superior Labrum Anterior Posterior Tears Improvements in Pain, Function, and Quality of Life Edwards et al • Approx. 50% of non operatively treated patients avoided surgery! Scapular strengthening, posterior capsular stretching Overtreat >>>> NIGHTMARE Make Sure History Consistent with SLAP “event” • Sudden loss of velocity (dead arm) • Large increase in pain • “mechanical symptoms” usually present • Rehab no longer effective Exam Hold Key!!! • Load Shift • Passive Distraction test • Mayo Shear • O’Brien’ Test (anterior) • Kim test • Relocation Test Mayo Shear -
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G
THE MANAGEMENT of SLAP INJURIES in the OVERHEAD ATHLETE Michael G. Ciccotti, MD The Everett J. and Marian Gordon Professor of Orthopaedics Chief, Division of Sports Medicine Rothman Institute Thomas Jefferson University Head Team Physician, Philadelphia Phillies Faculty Disclosure Consultant – Stryker Endoscopy Consultant – Venture MD Research Support – Arthrex Board/Committee Membership – Orthopaedic Learning Center BOD MLB Medical Advisory Committee MLB Elbow Research Study Group AOSSM Fellowship Committee Rothman Institute of Orthopaedics at Thomas Jefferson University Shoulder Injury in the Athlete History Exam 27 y.o. RHD MLB 30 deg. less ABD, FF pitcher 25 deg. less INT ROT Chronic, progressive + Hawkin’s Test right shoulder pain + O’Brien’s & DLS while throwing Tests Worsened acutely + mild-mod supraspinatus Pain is deep and post weakness Unable to throw Rothman Institute of Orthopaedics at Thomas Jefferson University ShoulderDiagnosis: Injury SLAP in the Athlete Tear Rothman Institute of Orthopaedics at Thomas Jefferson University Superior Labrum is Important for the Overhead Athlete! Biceps attachment site Deepens glenoid Distributes contact pressure between humerus & glenoid Harryman, 1992 – Washer Effect Pagnani, 1995 Lee, 2005 Attachment site for glenohumeral Veeger, 2007 ligaments & capsule Lee, 2008 Kibler, 2011 Pressure sensor for proprioception Rothman Institute of Orthopaedics at Thomas Jefferson University Predictable Series of Events in Throwers Progressive Osseous changes Scapular and Cuff -

Rehab for Bicep Tendon Problems
Rehabilitation for Biceps Tendon Disorders and SLAP Lesions 117 capsulitis will suffer long-term ROM defi cits that may arthroscopic release (5); or MUA and arthroscopic last more than 10 years. Clarke et al. (1975) reported hydrodistension (20). During the long-term follow-up that 42% of patients continued to have motion loss (mean 52.3 months) 59% of patients reported hav- after 6 years of follow-up. Likewise, Schaffer et al. ing normal or near-normal shoulders, 35% reported (1992) reported that 50% of patients managed non- persistent mild/moderate symptoms, and 6% still had operatively remained symptomatic during their long- severe symptoms. Persistent symptoms were reported term follow-up, which occurred 2–11 years after their as mild in 94% of patients, with pain being the most initial visit (mean = 7 years). Of these patients, 60% common complaint. Only 6% of patients complained had a measurable restriction of shoulder motion. of severe pain and/or functional loss. Patients with External rotation was the most chronically restricted the most severe symptoms at condition onset had the movement, providing further evidence that the rotator worst long-term prognosis. In general, patients with interval and coracohumeral ligament are particularly comorbid factors, particularly diabetes, hyperthyroid- affected by adhesive capsulitis. Hand et al. (2008) ism, hypothyroidism, hypoadrenalism, Parkinson's tracked outcomes in 269 shoulders affected by pri- disease, cardiac disease, pulmonary disease, or cere- mary adhesive capsulitis who received no treatment brovascular accident, tend to have more severe and (95); physical therapy (55); steroid injection (139); longer lasting symptoms and tend to be more recalci- manipulation under anesthesia (MUA) (5); MUA and trant to treatment. -
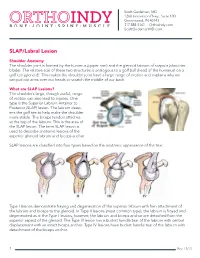
SLAP Lesions? the Shoulder’S Large, Though Useful, Range of Motion Can Also Lead to Injuries
Scott Gudeman, MD 1260 Innovation Pkwy., Suite 100 Greenwood, IN 46143 317.884.5161 OrthoIndy.com ScottGudemanMD.com SLAP/Labral Lesion Shoulder Anatomy The shoulder joint is formed by the humerus (upper arm) and the glenoid labrum of scapula (shoulder blade). The relative size of these two structures is analogous to a golf ball (head of the humerus) on a golf tee (glenoid). This makes the shoulder joint have a large range of motion and explains why we can put our arms over our heads or scratch the middle of our back. What are SLAP Lesions? The shoulder’s large, though useful, range of motion can also lead to injuries. One type is the Superior Labrum Anterior to Posterior (SLAP) lesion. The labrum deep- ens the golf tee to help make the shoulder more stable. The biceps tendon attaches at the top of the labrum. This is the area of the SLAP lesion. The term SLAP lesion is used to describe anatomic lesions of the superior glenoid labrum and biceps anchor. SLAP lesions are classified into four types based on the anatomic appearance of the tear. Type I lesions demonstrate fraying and degeneration of the superior labrum with firm attachment of the labrum and biceps to the glenoid. In Type II lesions (most common type), the labrum is frayed and degenerated as in the Type I lesions; however, the labrum and biceps anchor are detached from the superior aspect of the glenoid. The Type III lesion has a bucket handle tear of the labrum with central displacement with an intact biceps anchor. -

Evaluation of Humeral and Glenoid Bone Deformity in Glenohumeral Arthritis 5
Evaluation of Humeral and Glenoid Bone Deformity 1 in Glenohumeral Arthritis Brian F. Grogan and Charles M. Jobin Introduction glenoid bone wear helps the surgeon formulate a successful treatment plan and surgical goals Glenohumeral arthritis is the sequela of a vari- to address the pathoanatomy and improve the ety of pathologic shoulder processes, most durability of shoulder arthroplasty. The evalu- commonly degenerative osteoarthritis, but may ation of humeral and glenoid bone deformity also be secondary to post-traumatic conditions, in glenohumeral arthritis has profound surgical inflammatory arthritis, rotator cuff tear arthrop- implications and is fundamental to successful athy, and postsurgical conditions most com- shoulder arthroplasty. monly post-capsulorrhaphy arthritis. Patients with glenohumeral arthritis commonly demon- strate patterns of bony deformity on the glenoid Glenoid Deformity in Osteoarthritis and humerus that are caused by the etiology of the arthritis. For example, osteoarthritis com- Glenoid deformity and glenohumeral subluxation monly presents with posterior glenoid wear, are commonly seen in the setting of primary osteo- secondary glenoid retroversion, and posterior arthritis of the glenohumeral joint. The glenoid humeral head subluxation, while inflammatory wear tends to occur posteriorly and may be best arthritis routinely causes concentric glenoid viewed on axial radiographs or computed tomog- wear with central glenoid erosion. A thorough raphy (CT) axial images. Glenoid erosion, as first history and physical, as well as laboratory and characterized by Walch, is noted to be either central radiographic workup, are keys to understanding or posterior, with varying degrees of wear and pos- the etiology of arthritis and understanding the terior subluxation of the humerus [1, 2] (Fig. -

Peroneal Tendon Subluxation
CHAPTER 4 Peroneal Tendon Subluxation Jessica Lickiss, DPM Jay D. Ryan, DPM INTRODUCTION Peroneal tendon subluxation/ instability can be challenging IMAGING AND CLASSIFICATION to diagnose depending on the level of disruption and deformity present. Subtle cases will appear in the clinical Radiographs can be used to identify an avulsion and rule out setting similar to a lateral ankle sprain. This can cause a delay fracture. Computed tomography (CT) scan and MRI are in care and poorer outcomes for patients. both viable options for evaluation. MRI better evaluates the health of the peroneal tendons and CT scan demonstrates ANATOMY the shape and position of the fibula and fibular groove. While advanced imaging is a great adjunct, the diagnosis is mainly The peroneus longus and brevis muscle bellies travel clinical. For more subtle injuries where the tendons do not posterior to the fibula and fibular groove. At the fibular completely sublux or dislocate the fibula, dynamic ultrasound groove they are combined into one sheath; they separate can be used for diagnosing intrasheath instability (5). usually at the level of the peroneal tubercle. They are bound Eckert and Davis created a classification in 1976 for superiorly by the superior peroneal retinaculum (SPR) and SPR injuries (6). Grade I injuries involve elevation of the inferiorly by the calcaneofibular ligament (CFL) and the retinaculum from the lateral malleolus and the tendons inferior peroneal retinaculum (IPR). The superior peroneal can dislocate between the bone and periosteum. Grade II retinaculum has fibers that extend superiorly, posteriorly, injuries involve the fibrocartilaginous ridge elevating with and medially approximately 3.5 cm from the distal tip of the the retinaculum and tendon subluxed between it and the fibula (1). -

Sacroiliac Joint Injury and Dysfunction: an Overlooked Cause of Low Back and Buttock Pain
Sacroiliac Joint Injury and Dysfunction: An overlooked cause of Low Back and Buttock Pain. Author: Shannon P. Goossen, AP, LMT, CMTPT- 2003 The sacroiliac joint can be the cause of debilitating low back and buttock pain. It can additionally be the culprit of pseudo-sciatica, which was described by Smith- Peterson in 1926. Unfortunately, in as much as muscles are the “orphan organ” in the diagnosis of chronic pain, the sacroiliac joint is the “orphan joint” in the differential diagnosis of spinal disorders and low back pain. What is more disturbing is that in order to effectively treat SIJ injury and dysfunction, one must have an understanding of both myofascial and joint dysfunction. This could easily explain the controversy in evaluation, diagnosis and treatment. Fortunately, studies in the last decade have validated that the SIJ may be the primary pain generator in up to 30% of patients reporting low back pain below the level of L5 –S1 (Schwarzer, A et. al). Other studies and physicians treating SIJ have supported this conclusion as well. The sacroiliac joint is complex. It has the characteristics of a synovial joint with hyaline cartilage lining the sacral side of the joint, and fibrocartilage lining the ilial side of the joint. It is also defined as a synarthrosis and amphiarthrosis. It has more mobility early in life, and generally between 40-50 years of age, degenerative changes take place, and the joint stiffens in men and women. Although the actual amount of movement in the SIJ has been a source of controversy, up to 4 degrees of rotation and 1.6 mm of translation is expected in young adults (Vleeming et. -

Thumb Carpometacarpal Arthritis 952-920-0970
Douglas Drake, MD Orthopedic Surgeon and Hand Specialist 3250 W. 66th St. Suite #100 Edina, MN 55435 Thumb Carpometacarpal Arthritis 952-920-0970 Thumb CMC Arthritis: Idiopathic thumb basal joint aka thumb CMC arthritis StageIII: Continued joint narrowing with cystic changes is a result of anatomic factors that predispose the CMC and sclerotic bone formarion. Prominent osteophytes joint instability, such as joint configuration and ligamen- are present wiht moderate subluxation at the cmc joint tous laxity. CMC joint instability results in shear forces and subluxation at the MCP joint. at the joint surfaces and subsequent joint degeneration. Stage IV: All the components of stage III along with destruction of the scaphotrapezial joint. At this stage the CMC joint is usually fixed and some patients may have little to no pain. Treatment: In early stages, stage I and sometimes stage II, con- servative treatment should be considered. Conservative treatment consists of a period of thumb immobilization in a removable splint, see picture below, and use of NSAID’s. If splinting fails to relieve the pain then a corticosteroid injection may be performed. Of note, corticosteroid injections will not alter the progression of Prevalence: the disease but it may provide a few months of relief. Idiopathic thumb CMC arthritis is most common If conservative treatment fails to provide relief and pain amount women 40-70 years old. Women are 15 to 20 is making it difficult for the patient to perform daily times more likely than men to have thumb CMC arthri- functions or disease has progressed to stage III or IV tis; this is most likely secondary to increased joint laxity then surgical treatment in healthy patients should be found in women when compared to men. -

Prolotherapy: a Non-Invasive Approach to Lesions of the Glenoid Labrum; a Non-Controlled Questionnaire Based Study Ross A
Send Orders for Reprints to [email protected] The Open Rehabilitation Journal, 2013, 6, 69-76 69 Open Access Prolotherapy: A Non-Invasive Approach to Lesions of the Glenoid Labrum; A Non-Controlled Questionnaire Based Study Ross A. Hauser*, Erin Dolan and Amos Orlofsky Caring Medical and Rehabilitation Services, 715 Lake Street, Suite 600, Oak Park, IL 60301, USA Abstract: Lesions of the glenoid labrum are a common cause of shoulder instability and a frequent finding in patients with shoulder pain. Management of these patients typically involves an attempt to avoid surgery through conservative treatment. However, there is currently a dearth of conservative options that promote labral healing. Regenerative injection therapies, including prolotherapy, have shown promise in the treatment of several musculoskeletal disorders, but have not previously been applied to glenoid labral tear. Here we review several important aspects of these lesions and present an initial case series of 33 patients with labral tear that were treated in our clinic with intra-articular injections of hypertonic dextrose. Patient-reported assessments were collected by questionnaire at a mean follow-up time of 16 months. Treated patients reported highly significant improvements with respect to pain, stiffness, range of motion, crunching, exercise and need for medication. All 31 patients who reported pain at baseline experienced pain relief, and all 31 who reported exercise impairment at baseline reported improved exercise capability. Patients reported complete relief of 69% of recorded symptoms. One patient reported worsening of some symptoms. Prolotherapy for glenoid labral tear appears to be a safe procedure that merits further investigation. Keywords: Prolotherapy, glenoid labrum lesions, shoulder, hypertonic dextrose, musculosketetal repair, case report, regenerative injection therapy, glenoid labral tear. -

Biceps Tenodesis and Superior Labrum Anterior to Posterior (SLAP) Tears
5 Points on Biceps Tenodesis and Superior Labrum Anterior to Posterior (SLAP) Tears Mandeep S. Virk, MD, Annemarie K. Tilton, BS, and Brian J. Cole, MD, MBA njuries of the superior labrum–biceps complex (SLBC) presentation of SLAP tears, though localization and character- have been recognized as a cause of shoulder pain since ization of pain are variable and nonspecific.7 The mechanism Ithey were first described by Andrews and colleagues1 in of injury is helpful in acute presentation (traction injury; fall 1985. Superior labrum anterior to posterior (SLAP) tears are on outstretched, abducted arm), but an overhead athlete may relatively uncommon injuries of the shoulder, and their true present with no distinct mechanism other than chronic, re- incidence is difficult to establish. However, recently there petitive use of the shoulder.8-11 Numerous provocative physi- has been a significant increase in the reported incidence and cal examination tests have been used to assist in the diagnosis operative treatment of SLAP tears.2 SLAP tears can occur in of SLAP tear, yet there is no consensus regarding the ideal isolation, but they are commonly seen in association with physical examination test, with high sensitivity, specificity, other shoulder lesions, including rotator cuff tear, Bankart and accuracy.12-14 Magnetic resonance arthrography, the gold lesion, glenohumeral arthritis, acromioclavicular joint pa- standard imaging modality, is highly sensitive and specific thology, and subacromial impingement. (>95%) for diagnosing SLAP tears. Although SLAP tears are well described and classified,3-6 SLAP tear management is based on lesion type and se- our understanding of symptomatic SLAP tears and of their verity, age, functional demands, and presence of coexisting contribution to glenohumeral instability is limited. -

Marfan Syndrome: Jeffrey Welder MSIII, Erik L
Marfan Syndrome: Jeffrey Welder MSIII, Erik L. Nylen MSE, Thomas Oetting MS MD May 6, 2010 Chief Complaint: Decreased vision and glare in both eyes. History of Present Illness: A 28 year old woman with a history of Marfan syndrome presented to the comprehensive ophthalmology clinic reporting a progressive decrease in vision and worsening glare in both eyes. She had been seen by ophthalmologists in the past, and had been told that her crystalline lenses were subluxed in both eyes. She had not had problems with her vision until recent months. Past Medical History: Marfan syndrome with aortic stenosis followed by cardiology Medications: Oral beta blocker Family History: No known family members with Marfan Syndrome. Grandmother with glaucoma. Social History: The patient is a graduate student. Ocular Exam: External Exam normal. VA (with correction): OD 20/40 OS 20/50 Current glasses: OD: 6.75+ 5.00 x 135 OS: -5.25 + 4.25 x 60 Pupils: No anisocoria and no relative afferent pupillary defect Motility: Ocular motility full OU. Anterior segment exam: Inferiorly subluxed lenses OU (figure 1 and 2). The angle was deep OU and there was no lens apposition to the cornea in either eye. Dilated funduscopic exam: Posterior segment was normal OU with no peripheral retinal degeneration . Course: The patient’s subluxed lenses led to poor vision from peripheral lenticular irregular astigmatism and glare. She was taken to the operating room where her relatively clear lenses were removed and iris sutured intraocular lenses were placed. The surgical video for one of the eyes may be viewed at http://www.facebook.com/video/video.php?v=153379281140 Page | 1 Figure One: Note the inferiorly subluxed lens. -

Peroneal Tendon Disorders
Dr Todd Gothelf www.orthosports.com.au 47‐49 Burwood Road, Concord 29‐31 Dora Street, Hurstville 119‐121 Lethbridge Street, Penrith 160 Belmore Road, Randwick Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Peroneal Tendon Disorders Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Peroneal Tendon Disorders • Tenosynovitis •Tears • Snapping Peroneal Tendons Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Cause of injury •Occur during acute ankle sprain •Can occur as well by attrition over time. • Multiple ankle sprains/recurrent instability Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Lateral Ankle Sprain •“Complete Rupture of the ATFL Ligament” •Treated Non‐ operatively Dr Todd Gothelf Shoulder, Foot & Ankle Surgery ACL Rupture/ Rotator Cuff Tear •“Complete Rupture of the ACL ligament” •“Full Thickness tear of the Rotator Cuff • Usually require surgery Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Lateral Ankle Sprains •Treat the complete ATFL rupture NON‐ operatively • Similar outcomes to surgical treatment with LESS RISK. •Can Always do surgery later on. Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Causes of Pain after Lateral Ankle Sprain‐ NOT ATFL •Talardome lesions •Intra‐articular scar tissue, impingement • Peroneal tendon tears • Peroneal tendon dislocations •Missed achilles •Missed Syndesmosis •Missed Lis Franc Dr Todd Gothelf Shoulder, Foot & Ankle Surgery Anatomy Peroneal Tendons •Acute Angle around fibula • Eversion/Flexion •SPR‐