DHCS Is Submitting State Plan Amendments PA 12
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Californiachoice® Small Group Advantage PPO Three-Tier Hospital Network
CaliforniaChoice® Small Group Advantage PPO three-tier hospital network With the CaliforniaChoice Advantage PPO plans, you have a choice of tiers (or levels) of hospitals to visit. Tier one hospitals offer the greatest savings to you. Tier two hospitals have the second best level of savings. Tier three hospitals — or out-of-network hospitals — offer the least out-of-pocket savings, but you’ll still be covered. Keep in mind that the tier levels aren’t based on the quality of care given at each hospital. They’re based on which hospitals have shown they’re better able to give quality care that’s also cost effective. Our three-tier levels* are: }}Tier 1 — PPO network hospitals with lower-negotiated hospital reimbursement rates. }}Tier 2 — the remaining PPO network hospitals. }}Tier 3 — non-network hospitals. * The tier levels are not based on the quality of care given at each hospital. Instead, each level stands for the hospitals that show 19685CABENABC 08/15 the best use of health care dollars. CaliforniaChoice® Small Group Advantage PPO three-tier hospital network Here is a list of the Tier-1 and Tier-2 hospitals included in the network. Any hospital not listed is considered out of network. Hospital County Tier St Rose Hospital Alameda 1 Alameda Hospital Alameda 1 Children’s Hospital Oakland Alameda 2 Valleycare Medical Center Alameda 2 Washington Hospital Alameda 2 Sutter Amador Health Center Pioneer 1 Sutter Amador Health Center Plymouth 1 Sutter Amador Hospital Amador 1 Oroville Hospital & Medical Center Butte 1 Feather River Hospital -

Access+ HMO 2021Network
Access+ HMO 2021Network Our Access+ HMO plan provides both comprehensive coverage and access to a high-quality network of more than 10,000 primary care physicians (PCPs), 270 hospitals, and 34,000 specialists. You have zero or low copayments for most covered services, plus no deductible for hospitalization or preventive care and virtually no claims forms. Participating Physician Groups Hospitals Butte County Butte County BSC Admin Enloe Medical Center Cohasset Glenn County BSC Admin Enloe Medical Center Esplanade Enloe Rehabilitation Center Orchard Hospital Oroville Hospital Colusa County Butte County BSC Admin Colusa Medical Center El Dorado County Hill Physicians Sacramento CalPERS Mercy General Hospital Mercy Medical Group CalPERS Methodist Hospital of Sacramento Mercy Hospital of Folsom Mercy San Juan Medical Center Fresno County Central Valley Medical Medical Providers Inc. Adventist Medical Center Reedley Sante Community Physicians Inc. Sante Health Systems Clovis Community Hospital Fresno Community Hospital Fresno Heart and Surgical Hospital A Community RMCC Fresno Surgical Hospital San Joaquin Valley Rehabilitation Hospital Selma Community Hospital St. Agnes Medical Center Glenn County Butte County BSC Admin Glenn Medical Center Glenn County BSC Admin Humboldt County Humboldt Del Norte IPA Mad River Community Hospital Redwood Memorial Hospital St. Joseph Hospital - Eureka Imperial County Imperial County Physicians Medical Group El Centro Regional Medical Center Pioneers Memorial Hospital Kern County Bakersfield Family Medical -

Los Angeles County: 2015 Data
Using Data to Drive Change: California Continues to Increase In-hospital Exclusive Breastfeeding Rates A Policy Update on California Breastfeeding and Hospital Performance Produced by California WIC Association and the UC Davis Human Lactation Center Los Angeles County: 2015 Data Exclusive breastfeedng protects California’s success is driven by mothers' and babies' health evidence Breast milk provides all the nutrients infants need For more than 15 years, decision-makers and as well as specific factors needed to build a strong advocates in California have used hospital-level immune system.1 surveillance data to coordinate and monitor efforts to improve the quality of perinatal care. In-hospital support is crucial to breastfeeding mothers’ success.2-4 The greatest health benefits are Data show that mothers who experience more seen when exclusive breastfeeding continues for 6 supportive practices (such as early breastfeeding months. It is estimated that $3.0 billion in medical initiation and limited supplementation) are more costs would be saved if all U.S. infants were fed likely to breastfeed exclusively in the hospital and according to the current guidelines.5 beyond.6 Hospitals that have instituted Baby-Friendly policies California has the most Baby-Friendly Hospitals have high rates of breastfeeding, no matter where they in the nation and legislation requiring that all are located or what populations they serve.4,6 As more maternity hospitals adopt these or similar policies California hospitals have adopted these evidence- by -

Hospital Name City Staffed Beds Total Discharges
Gross Patient Staffed Total Patient Hospital Name City Revenue Beds Discharges Days ($000) Travis Air Force 60th Medical Group - David Grant USAF Medical Center 0 0 0 $0 Base Adventist Medical Center - Hanford Hanford 196 11,678 50,344 $869,494 Adventist Medical Center - Reedley Reedley 49 1,975 5,903 $69,121 Adventist Medical Center-Selma Selma 0 0 0 $0 Alameda Hospital Alameda 118 2,527 10,443 $244,188 Alhambra Hospital Medical Center Alhambra 144 3,910 17,589 $362,983 Alta Bates Summit Medical Center - Alta Bates Campus Berkeley 527 18,403 92,965 $2,136,597 Alta Bates Summit Medical Center - Herrick Campus Berkeley 0 0 0 $0 Alta Bates Summit Medical Center - Summit Campus Oakland 399 13,311 64,272 $1,778,929 Alvarado Hospital Medical Center San Diego 304 8,240 30,394 $577,818 Anaheim General Hospital Anaheim 112 762 3,387 $86,916 Anaheim Regional Medical Center Anaheim 223 12,930 58,195 $1,189,816 Antelope Valley Hospital Lancaster 399 25,285 115,259 $1,133,464 Antioch Medical Center Antioch 146 7,646 30,202 $0 Arrowhead Regional Medical Center Colton 452 18,115 96,586 $1,338,515 Arroyo Grande Community Hospital Arroyo Grande 67 2,727 9,441 $282,668 Bakersfield Heart Hospital Bakersfield 47 3,983 15,951 $333,450 Bakersfield Memorial Hospital Bakersfield 418 17,647 74,604 $1,228,503 Barstow Community Hospital Barstow 50 2,615 7,932 $285,538 Barton Memorial Hospital South Lake Tahoe 117 2,227 7,885 $245,205 Bear Valley Community Hospital Big Bear Lake 30 254 747 $36,273 Beverly Hospital Montebello 214 8,727 36,551 $283,788 Brotman Medical -

A Survey of California Hospitals Assisting Low-Income Uninsured Patients: a Survey of California Hospitals
ASSISTING LOW-INCOME UNINSURED PATIENTS: A SURVEY OF CALIFORNIA HOSPITALS ASSISTING LOW-INCOME UNINSURED PATIENTS: A SURVEY OF CALIFORNIA HOSPITALS HOSPITAL CHARITY CARE 1 INTRODUCTION 3 BROKEN HEALTH CARE SYSTEM 3 RIGID CHARITY CARE REQUIREMENTS 4 COMMITMENT TO CHARITY CARE PRINCIPLES AND GUIDELINES 5 HELPING HOSPITALS DEVELOP AND IMPLEMENT CHARITY CARE POLICIES 6 SURVEY OF HOSPITALS 8 SURVEY METHODOLOGY 8 SUMMARY OF FINDINGS 9 CONCLUSION 13 VOLUNTARY PRINCIPLES AND GUIDELINES FOR ASSISTING LOW-INCOME UNINSURED PATIENTS 2 PRINCIPLES AND GUIDELINES 15 APPENDIX SURVEY RESULTS 21 HOSPITAL CHARITY CARE INTRODUCTION Every hour of every day, medical miracles occur in hospitals throughout California. Whether it’s life-saving trauma care for the victim of a violent act or the joy of a precious newborn taking its first breath, hospitals are the cornerstones of our communities. For the vast majority of Californians—the more than 80 percent who have some form of governmental or private health insurance coverage—the sophisticated technologies of a modern hospital are often taken for granted. But for a patient who is uninsured and at the lower end of the economic scale, what was once a miraculous occasion can turn into a financial quagmire. A hospital’s job—first and foremost—is to provide care to all patients. California hospitals fulfill this mission every day. Hospitals are the providers of health care, not the financiers. However, because we take our mission to BROKEN HEALTH CARE SYSTEM serve seriously, California hospitals also are committed to assisting those patients who truly cannot afford the health care they need. A key element being overlooked in the public debate about hospital charity care is the underlying This report, as promised to the administration cause of the problem: a broken health care system of Governor Arnold Schwarzenegger, the that has left nearly 7 million people—one out of Legislature and other key policymakers, offers five Californians—with no health insurance. -
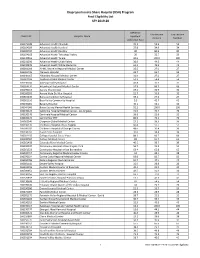
Disproportionate Share Hospital (DSH) Program Final Eligibility List SFY 2019-20
Disproportionate Share Hospital (DSH) Program Final Eligibility List SFY 2019-20 Medicaid Low Income Low Income OSHPD ID Hospital Name Inpatient Percent Number Utilization Rate 106171049 Adventist Health Clearlake 35.3 54.9 54 106164029 Adventist Health Hanford 37.8 34.9 34 106100797 Adventist Health Reedley 80 80.9 80 106154168 Adventist Health Tehachapi Valley 20 50.7 50 106540816 Adventist Health Tulare 30.6 100.0 100 106231396 Adventist Health Ukiah Valley 36.9 44.5 44 106190878 Adventist Health White Memorial 63.1 45.5 45 106301098 AHMC Anaheim Regional Medical Center 35.5 27.9 27 106010735 Alameda Hospital 33.7 53.7 53 106190017 Alhambra Hospital Medical Center 31.6 27.2 27 106301188 Anaheim Global Medical Center 54.3 54.4 54 106190034 Antelope Valley Hospital 43.8 37.2 37 106364231 Arrowhead Regional Medical Center 57.9 69.7 69 106190163 Aurora Charter Oak 19.4 32.9 32 106560203 Aurora Vista Del Mar Hospital 22.7 33.9 33 106364430 Barstow Community Hospital 39.1 27.2 27 106361110 Bear Valley Community Hospital 9.3 42.7 42 106190081 Beverly Hospital 40.1 56.1 56 106044006 Butte County Mental Health Services 92.2 100.0 100 106190125 California Hospital Medical Center - Los Angeles 72.5 70.7 70 106190148 Centinela Hospital Medical Center 38.8 32.6 32 106105125 Central Star PHF 86.6 76.2 76 106301140 Chapman Global Medical Center 13.1 36.3 36 106190170 Children's Hospital of Los Angeles 60.8 55.7 55 106300032 Children's Hospital of Orange County 48.6 30.4 30 106190766 Coast Plaza Hospital 37.6 34.4 34 106301155 College Hospital Costa -

The World's Most Active Hospital & Healthcare
The USA's Most Active Hospital & Healthcare Professionals on Social - August 2021 Industry at a glance: Why should you care? So, where does your company rank? Position Company Name LinkedIn URL Location Employees on LinkedIn No. Employees Shared (Last 30 Days) % Shared (Last 30 Days) 1 symplr https://www.linkedin.com/company/symplr/United States 1,101 204 18.53% 2 Covenant Care https://www.linkedin.com/company/covenant-care-corp/United States 509 88 17.29% 3 Johnson & Johnson Consumer Health https://www.linkedin.com/company/johnson-johnson-consumer-health/United States 727 112 15.41% 4 Phreesia https://www.linkedin.com/company/phreesia/United States 1,201 185 15.40% 5 Labcorp Drug Development https://www.linkedin.com/company/labcorpdrugdev/United States 4,362 661 15.15% 6 BrightSpring Health Services https://www.linkedin.com/company/brightspringhealth/United States 17,110 2,500 14.61% 7 Teladoc Health https://www.linkedin.com/company/teladoc-health/United States 3,932 572 14.55% 8 Alto Pharmacy https://www.linkedin.com/company/altopharmacy/United States 749 104 13.89% 9 Quantum Health https://www.linkedin.com/company/quantum-health/United States 899 119 13.24% 10 Imprivata https://www.linkedin.com/company/imprivata/United States 612 78 12.75% 11 American College of Cardiology https://www.linkedin.com/company/american-college-of-cardiology/United States 771 97 12.58% 12 VillageMD https://www.linkedin.com/company/villagemd/United States 862 108 12.53% 13 Oak Street Health https://www.linkedin.com/company/oak-street-health/United States 1,692 211 12.47% 14 ECRI https://www.linkedin.com/company/ecri-org/United States 539 64 11.87% 15 Shields Health Solutions https://www.linkedin.com/company/shields-health-solutions/United States 603 70 11.61% 16 Amwell https://www.linkedin.com/company/amwellcorp/United States 1,104 125 11.32% 17 St. -

County Hospital CMQCC Member Maternal Data Center Participant System Alameda Alta Bates Yes Yes Sutter Health Alameda Eden Medic
Maternal Data Center County Hospital CMQCC Member Participant System Alameda Alta Bates Yes Yes Sutter Health Alameda Eden Medical Center Yes Yes Sutter Health Alameda Highland Hospital Yes Yes Alameda Kaiser-Oakland Yes Yes KP Northern California Region Alameda Kaiser-San Leandro Yes Yes KP Northern California Region Alameda St. Rose Hospital No No Alameda Stanford-ValleyCare-Pleasanton Yes Yes Alameda Washington Hospital Yes Yes Amador Sutter Amador Yes Yes Sutter Health Butte Enloe Medical Center Yes Yes Butte Oroville Hospital No No Contra Costa Contra Costa Regional Yes Yes Contra Costa John Muir-Walnut Creek Yes Yes Contra Costa Kaiser-Antioch Yes Yes KP Northern California Region Contra Costa Kaiser-Walnut Creek Yes Yes KP Northern California Region Contra Costa San Ramon Regional Medical Center Yes Yes Tenet Healthcare Contra Costa Sutter Delta Yes Yes Sutter Health Del Norte Sutter Coast Yes Yes Sutter Health El Dorado Barton Memorial Hospital Yes Yes El Dorado Marshall Medical Center Yes Yes Fresno Adventist Health Reedley Yes Yes Adventist Fresno Clovis Community Medical Center Yes Yes Community Medical Centers Fresno Community Regional Yes Yes Community Medical Centers Fresno Kaiser-Fresno Yes Yes KP Northern California Region Fresno Saint Agnes Medical Center Yes Yes Humboldt Mad River Community Hospital Yes Yes Humboldt Redwood Memorial Hospital Yes Yes Providence St. Joseph Health Humboldt St. Joseph Hospital-Eureka Yes Yes Providence St. Joseph Health Imperial El Centro Regional Medical Center Yes Yes Imperial Pioneers Memorial Healthcare District No No Inyo Northern Inyo Hospital Yes Yes Updated January 12, 2021: There are 213 CMQCC members with 207 members actively submitting data to the Maternal Data Center. -

PPO Select Narrow Hospital Network
PPO Select Narrow Hospital Network Hospital County Tier ALAMEDA HOSPITAL ALAMEDA 1 ST ROSE HOSPITAL ALAMEDA 1 CHILDREN'S HOSPITAL OAKLAND ALAMEDA 2 VALLEYCARE MEDICAL CENTER ALAMEDA 2 WASHINGTON HOSPITAL ALAMEDA 2 SUTTER AMADOR HOSPITAL AMADOR 1 BIGGS MEMORIAL HOSPITAL BUTTE 1 FEATHER RIVER HOSPITAL BUTTE 1 OROVILLE HOSPITAL & MEDICAL CENTER BUTTE 1 ENLOE MEDICAL CENTER INC BUTTE 2 MARK TWAIN ST JOSEPH'S HOSPITAL CALAVERAS 1 COLUSA REGIONAL MEDICAL CENTER COLUSA 1 DOCTORS MEDICAL CENTER – SAN PABLO/PINOLE CONTRA COSTA 1 SAN RAMON REGIONAL MEDICAL CENTER CONTRA COSTA 1 JOHN MUIR MEDICAL CENTER – CONCORD CAMPUS CONTRA COSTA 2 JOHN MUIR MEDICAL CENTER – WALNUT CREEK CONTRA COSTA 2 SUTTER COAST HOSPITAL DEL NORTE 1 MARSHALL MEDICAL CENTER EL DORADO 1 BARTON MEMORIAL HOSPITAL EL DORADO 2 CLOVIS COMMUNITY HOSPITAL FRESNO 1 COALINGA REGIONAL MEDICAL CENTER FRESNO 1 COMMUNITY MEDICAL CENTER – FRESNO FRESNO 1 FRESNO HEART HOSPITAL FRESNO 1 FRESNO SURGICAL HOSPITAL FRESNO 1 SAN JOAQUIN VALLEY REHABILITATION HOSPITAL FRESNO 1 SIERRA KINGS DISTRICT HOSPITAL FRESNO 1 ST AGNES MEDICAL CENTER FRESNO 1 KINGSBURG DISTRICT HOSPITAL FRESNO 2 GLENN MEDICAL CENTER GLENN 1 MAD RIVER COMMUNITY HOSPITAL HUMBOLDT 1 JEROLD PHELPS COMMUNITY HOSPITAL HUMBOLDT 2 REDWOOD MEMORIAL HOSPITAL HUMBOLDT 2 ST JOSEPH HOSPITAL – EUREKA HUMBOLDT 2 EL CENTRO REGIONAL MEDICAL CENTER IMPERIAL 1 PIONEERS MEMORIAL HEALTHCARE DISTRICT IMPERIAL 1 NORTHERN INYO HOSPITAL INYO 1 SOUTHERN INYO HOSPITAL INYO 1 GOOD SAMARITAN HOSPITAL KERN 1 HEALTHSOUTH BAKERSFIELD REHABILITATION HOSPITAL -

OSHPD FACILITY CODES -- Sorted by Hospital CPQCC Centers Indicated in Bold Italics
OSHPD FACILITY CODES -- Sorted by Hospital CPQCC Centers Indicated in Bold Italics OSHPD CENTER NAME CITY COUNTY 700564 30TH MEDICAL GROUP (700564) 700597 60TH MEDICAL GROUP (700597) 700431 722ND MEDICAL GROUP (700431) 700103 95TH MEDICAL GROUP (700103) 190323 ADVENTIST HEALTH - GLENDALE (190323) GLENDALE LOS ANGELES 190878 ADVENTIST HEALTH - WHITE MEMORIAL (190878) LOS ANGELES LOS ANGELES 150788 ADVENTIST HEALTH BAKERSFIELD (150788) BAKERSFIELD KERN 171049 ADVENTIST HEALTH CLEARLAKE (171049) CLEARLAKE LAKE 040875 ADVENTIST HEALTH FEATHER RIVER (040875) PARADISE BUTTE 164029 ADVENTIST HEALTH HANFORD (164029) HANFORD KINGS 390923 ADVENTIST HEALTH LODI MEMORIAL (390923) LODI SAN JOAQUIN 150808 ADVENTIST HEALTH MEDICAL CENTER TEHACHAPI VALLEY (150808) TEHACHAPI KERN 560525 ADVENTIST HEALTH SIMI VALLEY (560525) SIMI VALLEY VENTURA 554011 ADVENTIST HEALTH SONORA - GREENLEY (554011) SONORA TUOLUMNE 281078 ADVENTIST HEALTH ST. HELENA (281078) ST. HELENA NAPA 231396 ADVENTIST HEALTH UKIAH VALLEY (231396) UKIAH MENDOCINO 160787 ADVENTIST MEDICAL CENTER - CENTRAL VALLEY (160787) 100797 ADVENTIST MEDICAL CENTER - REEDLEY (100797) REEDLEY FRESNO 100793 ADVENTIST MEDICAL CENTER-SELMA (100793) SELMA FRESNO 301098 AHMC ANAHEIM REGIONAL MEDICAL CENTER (301098) ANAHEIM ORANGE 010735 ALAMEDA HOSPITAL (010735) ALAMEDA ALAMEDA 010989 ALAMEDA HOSPITAL AT WATERS EDGE (010989) ALAMEDA ALAMEDA 190017 ALHAMBRA HOSPITAL MEDICAL CENTER (190017) ALHAMBRA LOS ANGELES 010844 ALTA BATES SUMMIT MED CTR-HERRICK CAMPUS (010844) BERKELEY ALAMEDA 010937 ALTA BATES SUMMIT -

Emanate- Intercommunity Hospital Angio Suite Remodel
ACUTE CARE HOSPITAL OSHPD PROJECT NAME SQUARE FEET CITY Yes AHMC - Garfield Pharmacy Remodel Monterey Park Yes AHMC - San Gabriel Pharmacy San Gabriel Yes Alhambra Community Hospital - 2nd Floor Isolation Yes Alhambra Community Hospital - Med. Surg. Yes Alhambra Community Hospital - Radiology Remodel Yes Alta Bellflower - 3 HVAC Bellflower Yes Alta Foothill - Steam Line Replacement Tustin Yes Alta-Foothill Fan Coil Replacement - Phase 1, 2 &3 Tustin Yes Alta-Foothill Fan Coil Replacement - Phase 4 & 5 Tustin Yes Alta-Foothill Fan Coil Replacement - Phase III Tustin Kitchen OSHPD PROJECT NAME SQUARE FEET CITY Yes Alta-Foothill Fan Coil Replacement - Phase IV Tustin Material Mgmt American Golf Corp. - Elevator Addition AMI TSS Phase II Mobile Scanner Facility Yes Antelope Valley Hospital - 3rd Floor Pathology Lancaster Yes Antelope Valley Hospital - Elevator Lobby Lancaster, CA Antelope Valley Hospital - Lab/Blood Donor Yes Antelope Valley Hospital - Mental Health Patient Lancaster Safety Upgrades Antelope Valley Hospital - OPIC, Suite 207 Lancaster Yes Antelope Valley Hospital - Pharmacy IV Room Lancaster Yes Antelope Valley Medical Center - 5th Floor Med. Surgery Yes Antelope Valley Medical Center - CCU Yes Antelope Valley Medical Center - ER Doors Yes Antelope Valley Medical Center - Mental Health Ward Yes Antelope Valley Medical Center - Steam Pipe Replacement Yes Arcadia Methodist Hospital - Pharmacy Addition Yes Arcadia Methodist Hospital - Zonac Unit Arcadia Radiology - Mammo Aspen Center - Administrative Remodel Aspen Center - Blood -

CHPSO Member Listing Members As of March 30, 2017 7Th Avenue
CHPSO Member Listing Leandro Mills-Peninsula Health Services, Burlingame Southern California Hospital at Culver City, Culver City Members as of March 30, 2017 Feather River Hospital, Paradise Mills-Peninsula Medical Center, Burlingame Southern California Hospital at Hollywood, Los Angeles Foothill Presbyterian Hospital, Glendora Mission Heritage Medical Group, Mission Viejo Southern California Hospital at Van Nuys, Van Nuys 7th Avenue Family Center, Phoenix, AZ Frank R. Howard Memorial Hospital, Willits Mission Hospital Laguna Beach, Laguna Beach Southern Inyo Hospital, Lone Pine 7th Avenue Walk-in Clinic, Phoenix, AZ Fremont Medical Center, Yuba City Modoc Medical Center, Alturas Stanford Health Care — ValleyCare, Pleasanton Adventist Health, Roseville French Hospital Medical Center, San Luis Obispo Montclair Hospital Medical Center, Montclair Stanford Health Care — ValleyCare-Livermore, Livermore Adventist Medical Center — Hanford, Hanford Fresno Heart & Surgical Hospital, Fresno Monterey Park Hospital, Monterey Park Stanford Health System, Palo Alto Adventist Medical Center — Portland, Portland, OR Garden Grove Hospital and Medical Center, Garden MPHS Senior Focus, Burlingame St. Bernardine Medical Center, San Bernardino Adventist Medical Center — Reedley, Reedley Grove Natividad Medical Center, Salinas St. Elizabeth Community Hospital, Red Bluff Adventist Medical Center — Selma, Selma Garfield Medical Center, Monterey Park Nix Behavioral Health, San Antonio, TX St. Francis Medical Center, Lynwood AHMC Anaheim Regional Medical Center, Anaheim Gateways Hospital and Mental Health Center, Los Nix Hospitals System, LLC, San Antonio, TX St. Helena Hospital Center for Behavioral Health, Vallejo AHMC Healthcare, Inc., Alhambra Angeles Nix Medical Center, San Antonio, TX St. Helena Hospital Clear Lake, Clearlake Alameda Hospital, Alameda General Hospital Campus of St. Joseph Hospital, Eureka Nix Specialty Health Center, San Antonio, TX St.