Stimulants and Related Agents Review 10/11/2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Methylphenidate Hydrochloride
Application for Inclusion to the 22nd Expert Committee on the Selection and Use of Essential Medicines: METHYLPHENIDATE HYDROCHLORIDE December 7, 2018 Submitted by: Patricia Moscibrodzki, M.P.H., and Craig L. Katz, M.D. The Icahn School of Medicine at Mount Sinai Graduate Program in Public Health New York NY, United States Contact: [email protected] TABLE OF CONTENTS Page 3 Summary Statement Page 4 Focal Point Person in WHO Page 5 Name of Organizations Consulted Page 6 International Nonproprietary Name Page 7 Formulations Proposed for Inclusion Page 8 International Availability Page 10 Listing Requested Page 11 Public Health Relevance Page 13 Treatment Details Page 19 Comparative Effectiveness Page 29 Comparative Safety Page 41 Comparative Cost and Cost-Effectiveness Page 45 Regulatory Status Page 48 Pharmacoepial Standards Page 49 Text for the WHO Model Formulary Page 52 References Page 61 Appendix – Letters of Support 2 1. Summary Statement of the Proposal for Inclusion of Methylphenidate Methylphenidate (MPH), a central nervous system (CNS) stimulant, of the phenethylamine class, is proposed for inclusion in the WHO Model List of Essential Medications (EML) & the Model List of Essential Medications for Children (EMLc) for treatment of Attention-Deficit/Hyperactivity Disorder (ADHD) under ICD-11, 6C9Z mental, behavioral or neurodevelopmental disorder, disruptive behavior or dissocial disorders. To date, the list of essential medications does not include stimulants, which play a critical role in the treatment of psychotic disorders. Methylphenidate is proposed for inclusion on the complimentary list for both children and adults. This application provides a systematic review of the use, efficacy, safety, availability, and cost-effectiveness of methylphenidate compared with other stimulant (first-line) and non-stimulant (second-line) medications. -

The Stimulants and Hallucinogens Under Consideration: a Brief Overview of Their Chemistry and Pharmacology
Drug and Alcohol Dependence, 17 (1986) 107-118 107 Elsevier Scientific Publishers Ireland Ltd. THE STIMULANTS AND HALLUCINOGENS UNDER CONSIDERATION: A BRIEF OVERVIEW OF THEIR CHEMISTRY AND PHARMACOLOGY LOUIS S. HARRIS Dcparlmcnl of Pharmacology, Medical College of Virginia, Virginia Commonwealth Unwersity, Richmond, VA 23298 (U.S.A.) SUMMARY The substances under review are a heterogenous set of compounds from a pharmacological point of view, though many have a common phenylethyl- amine structure. Variations in structure lead to marked changes in potency and characteristic action. The introductory material presented here is meant to provide a set of chemical and pharmacological highlights of the 28 substances under con- sideration. The most commonly used names or INN names, Chemical Abstract (CA) names and numbers, and elemental formulae are provided in the accompanying figures. This provides both some basic information on the substances and a starting point for the more detailed information that follows in the individual papers by contributors to the symposium. Key words: Stimulants, their chemistry and pharmacology - Hallucinogens, their chemistry and pharmacology INTRODUCTION Cathine (Fig. 1) is one of the active principles of khat (Catha edulis). The structure has two asymmetric centers and exists as two geometric isomers, each of which has been resolved into its optical isomers. In the plant it exists as d-nor-pseudoephedrine. It is a typical sympathomimetic amine with a strong component of amphetamine-like activity. The racemic mixture is known generically in this country and others as phenylpropanolamine (dl- norephedrine). It is widely available as an over-the-counter (OTC) anti- appetite agent and nasal decongestant. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Oregon Dur Board Newsletter a N E Vidence B Ased D Rug T Herapy R Esource Copyright 2002 Oregon State University
OREGON DUR BOARD NEWSLETTER A N E VIDENCE B ASED D RUG T HERAPY R ESOURCE COPYRIGHT 2002 OREGON STATE UNIVERSITY. ALL RIGHTS RESERVED Volume 4, Issue 2 Also available on the web and via e-mail list-serve at April 2002 http://pharmacy.orst.edu/drug_policy/drug_policy.html A Review of Stimulant Medications By Ann Hamer, Pharm. D., OSU College of Pharmacy Attention deficit hyperactivity disorder (ADHD) is a psychiatric disorder four hours (5,6). Measures of efficacy included behavior frequency, characterized by inattention, hyperactivity, or impulsivity that is more completion and accuracy of academic problems, independent frequent or severe than is appropriate for the patient’s developmental observations, as well as teacher and counselor ratings. The extended level(1). It is estimated that 3 to 7 % of children have ADHD making it one release property of Concerta is based on its OROS delivery system (an of the most common psychiatric disorders of childhood and osmotically active trilayer core surrounded by a semipermeable membrane adolescence(2). with an immediate-release drug overcoat)(7). PHARMACOTHERAPY Patients new to methylphenidate should start Concerta at a dose of 18mg Stimulants are considered first-line agents for the treatment of children once daily. The dose may be adjusted based on the patient’s response in (greater than six years of age) with ADHD and are the only agents increments of 18mg per week to a maximum recommended dose of approved by the Food and Drug Administration (FDA) for this purpose(3). 54mg/day. The recommended dose conversion for patients currently Stimulant medications (including methylphenidate preparations, taking methylphenidate is summarized as follows: dextroamphetamine preparations, and pemoline) have CNS and RECOMMENDED CURRENT METHYLPHENIDATE DOSE respiratory stimulant properties and weak sympathomimetic activity. -
Enhanced Reporting
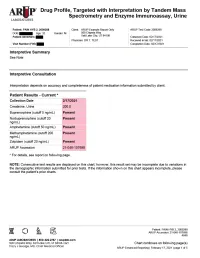
Drug Profile, Targeted with Interpretation by Tandem Mass Spectrometry and Enzyme Immunoassay, Urine Patient: PAIN HYB 2, 2009288 | Date of Birth: | Gender: M | Physician: DR T. TEST Patient Identifiers: | Visit Number (FIN): Drug Analyte Result Cutoff Notes Meperidine metabolite Not Detected 50 ng/mL normeperidine Tapentadol Not Detected 100 ng/mL --Tapentadol-o-sulfate Not Detected 200 ng/mL tapentadol metabolite AMPHETAMINE-LIKE, MASS SPEC Amphetamine Present 50 ng/mL eg, Vyvanse; also a metabolite of methamphetamine Methamphetamine Present 200 ng/mL d- and l- isomers are not distinguished by this test; may reflect Vicks inhaler, Desoxyn, Selegiline, or illicit source MDMA - Ecstasy Not Detected 200 ng/mL MDA Not Detected 200 ng/mL also a metabolite of MDMA and MDEA MDEA - Eve Not Detected 200 ng/mL Phentermine Not Detected 100 ng/mL Methylphenidate Not Detected 100 ng/mL eg, Ritalin, Dexmethylphenidate, Focalin, Concerta BENZODIAZEPINE-LIKE, MASS SPEC Alprazolam Not Detected 40 ng/mL eg, Xanax --Alpha-hydroxyalprazolam Not Detected 20 ng/mL alprazolam metabolite Clonazepam Not Detected 20 ng/mL eg, Klonopin --7-aminoclonazepam Not Detected 40 ng/mL clonazepam metabolite Diazepam Not Detected 50 ng/mL eg, Valium Nordiazepam Not Detected 50 ng/mL metabolite of chlordiazepoxide (Librium), clorazepate (Tranxene), diazepam, halazepam (Alapryl), prazepam (Centrax) and others Oxazepam Not Detected 50 ng/mL eg, Serax; also metabolite of nordiazepam and temazepam Temazepam Not Detected 50 ng/mL eg, Restoril; also a metabolite of diazepam Lorazepam Not Detected 60 ng/mL eg, Ativan Midazolam Not Detected 20 ng/mL eg, Versed Zolpidem Present 20 ng/mL eg, Ambien Reference interval Creatinine value (mg/dL) 200.0 20.0 - 400.0 mg/dL Patient: PAIN HYB 2, 2009288 ARUP Accession: 21-048-107698 4848 Chart continues on following page(s) ARUP Enhanced Reporting | February 17, 2021 | page 4 of 5 Drug Profile, Targeted with Interpretation by Tandem Mass Spectrometry and Enzyme Immunoassay, Urine Patient: PAIN HYB 2, 2009288 | Date of Birth | Gender: M | Physician: DR T. -

Amphetamine/Dextroamphetamine IR Generic
GEORGIA MEDICAID FEE-FOR-SERVICE STIMULANT AND RELATED AGENTS PA SUMMARY Preferred Non-Preferred Amphetamine/dextroamphetamine IR generic Adzenys ER (amphetamine ER oral suspension) Armodafinil generic Adzenys XR (amphetamine ER dispersible tab) Atomoxetine generic Amphetamine/dextroamphetamine ER (generic Concerta (methylphenidate ER/SA) Adderall XR) Dextroamphetamine IR tablets generic Aptensio XR (methylphenidate ER) Focalin (dexmethylphenidate) Clonidine ER generic Focalin XR (dexmethylphenidate ER) Cotempla XR (methylphenidate ER disintegrating Guanfacine ER generic tablet) Methylin oral solution (methylphenidate) Daytrana (methylphenidate TD patch) Methylphenidate CD/CR/ER generic by Lannett Desoxyn (methamphetamine) [NDCs 00527-####-##] and Kremers Urban [NDCs Dexmethylphenidate IR generic 62175-####-##] (generic Metadate CD) Dexmethylphenidate ER generic Methylphenidate IR generic Dextroamphetamine ER capsules generic Modafinil generic Dextroamphetamine oral solution generic Quillichew ER (methylphenidate ER chew tabs) Dyanavel XR (amphetamine ER oral suspension) Quillivant XR (methylphenidate ER oral suspension) Evekeo (amphetamine tablets) Vyvanse (lisdexamfetamine) Methamphetamine generic Zenzedi 5 mg, 10 mg IR tablets (dextroamphetamine) Methylphenidate IR chewable tablets generic Methylphenidate ER/SA (generic Concerta) Methylphenidate ER/LA/SR (generic Ritalin LA, Ritalin SR, Metadate ER) Methylphenidate ER/SA 72 mg generic Methylphenidate oral solution generic Mydayis (amphetamine/dextroamphetamine ER) Ritalin LA 10 mg -
Current Topics in Behavioral Neurosciences
Current Topics in Behavioral Neurosciences Series Editors Mark A. Geyer, La Jolla, CA, USA Bart A. Ellenbroek, Wellington, New Zealand Charles A. Marsden, Nottingham, UK For further volumes: http://www.springer.com/series/7854 About this Series Current Topics in Behavioral Neurosciences provides critical and comprehensive discussions of the most significant areas of behavioral neuroscience research, written by leading international authorities. Each volume offers an informative and contemporary account of its subject, making it an unrivalled reference source. Titles in this series are available in both print and electronic formats. With the development of new methodologies for brain imaging, genetic and genomic analyses, molecular engineering of mutant animals, novel routes for drug delivery, and sophisticated cross-species behavioral assessments, it is now possible to study behavior relevant to psychiatric and neurological diseases and disorders on the physiological level. The Behavioral Neurosciences series focuses on ‘‘translational medicine’’ and cutting-edge technologies. Preclinical and clinical trials for the development of new diagostics and therapeutics as well as prevention efforts are covered whenever possible. Cameron S. Carter • Jeffrey W. Dalley Editors Brain Imaging in Behavioral Neuroscience 123 Editors Cameron S. Carter Jeffrey W. Dalley Imaging Research Center Department of Experimental Psychology Center for Neuroscience University of Cambridge University of California at Davis Downing Site Sacramento, CA 95817 Cambridge CB2 3EB USA UK ISSN 1866-3370 ISSN 1866-3389 (electronic) ISBN 978-3-642-28710-7 ISBN 978-3-642-28711-4 (eBook) DOI 10.1007/978-3-642-28711-4 Springer Heidelberg New York Dordrecht London Library of Congress Control Number: 2012938202 Ó Springer-Verlag Berlin Heidelberg 2012 This work is subject to copyright. -

Provider Notice
Mental Health Provider Quick Reference ▪ For current information visit http://kentucky.fhsc.com/pharmacy/default.asp ▪ To access the complete Preferred Drug List, click on the "Providers" tab and select "Drug Information" ▪ Managed Access Program/Prior Authorization: 800-477-3071 ▪ Mental Health Provider Prior Authorization FAX line: 800-453-2273 Class All are covered first tier with PA which may be obtained electronically (or by fax) within appropriate dosage, duplicate therapy Atypical Antipsychotics and ICD9 requirements Class First Generation Antipsychotics All are covered first tier without restriction Class Anticonvulsants All generic products are covered first tier without restriction. Brand products are second tier. CNS Stimulants for Patients <= 18 years old DRUG COPAY TIER PA MAXIMUM QUANTITY COMMENTS REQUIRED AVAILABLE WITHOUT (CLINICAL OR PRIOR AUTHORIZATION PDL) ALONE COMBINED SHORT-ACTING CNS STIMULANTS Adderall N/A NO 90 Any Patient may receive a total of up to 90 Amphetamine salt combo combination of dosage units/30 days alone, or in short-acting combination with other short-acting Dexmethylphenidate CNS stimulants (Adderall, Amphetamine Salt Focalin Stimulants not Combo, Dexmethylphenidate, and Focalin), to exceed 90 independent of long-acting stimulants dosage units (Adderall XR, Concerta, Focalin XR, and Vyvanse) and Strattera quantities LONG-ACTING CNS STIMULANTS Adderall XR N/A NO 60 Any Patient may receive a total of up to 60 Concerta combination of dosage units/30 days alone, or in Focalin XR extended combination -

A Brief Overview of Psychiatric Pharmacotherapy
A Brief Overview of Psychiatric Pharmacotherapy Joel V. Oberstar, M.D. Chief Executive Officer Disclosures • Some medications discussed are not approved by the FDA for use in the population discussed/described. • Some medications discussed are not approved by the FDA for use in the manner discussed/described. • Co-Owner: – PrairieCare and PrairieCare Medical Group – Catch LLC Disclaimer The contents of this handout are for informational purposes only and are not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical or psychiatric condition. Never disregard professional/medical advice or delay in seeking it because of something you have read in this handout. Material in this handout may be copyrighted by the author or by third parties; reasonable efforts have been made to give attribution where appropriate. Caveat Regarding the Role of Medication… Neuroscience Overview Mind Over Matter, National Institute on Drug Abuse, National Institutes of Health. Available at: http://teens.drugabuse.gov/mom/index.asp. http://medicineworld.org/images/news-blogs/brain-700997.jpg Neuroscience Overview Mind Over Matter, National Institute on Drug Abuse, National Institutes of Health. Available at: http://teens.drugabuse.gov/mom/index.asp. Neurotransmitter Receptor Source: National Institute on Drug Abuse Common Diagnoses and Associated Medications • Psychotic Disorders – Antipsychotics • Bipolar Disorders – Mood Stabilizers, Antipsychotics, & Antidepressants • Depressive Disorders – Antidepressants • Anxiety Disorders – Antidepressants & Anxiolytics • Attention Deficit Hyperactivity Disorder – Stimulants, Antidepressants, 2-Adrenergic Agents, & Strattera Classes of Medications • Anti-depressants • Stimulants and non-stimulant alternatives • Anti-psychotics (a.k.a. -

Dexmethylphenidate
MICROMEDEX® Healthcare Series : Document Page 1 of 31 Case 3:09-cv-00080-TMB Document 78-23 Filed 03/24/2010 Page 1 of 105 DRUGDEX® Evaluations DEXMETHYLPHENIDATE 0.0 Overview 1) Class a) This drug is a member of the following class(es): Amphetamine Related CNS Stimulant 2) Dosing Information a) Dexmethylphenidate Hydrochloride 1) Adult a) Attention deficit hyperactivity disorder 1) extended-release: methylphenidate-naive patients, initial 10 mg ORALLY daily in the morning; adjust dose weekly in 10 mg increments; MAX 20 mg/day 2) extended-release: patients currently using methylphenidate, one-half the total daily dose of racemic methylphenidate; patients currently using dexmethylphenidate immediate-release may be switched to the same daily dose of dexmethylphenidate extended-release; MAX 20 mg/day 2) Pediatric a) safety and efficacy not established in patients under 6 years of age 1) Attention deficit hyperactivity disorder a) immediate-release (ages 6 years and older): methylphenidate-naive patients, initial 2.5 mg ORALLY twice daily; adjust dose weekly in 2.5 to 5 mg increments; MAX 20 mg/day (10 mg twice a day) b) immediate-release (ages 6 years and older): patients currently using methylphenidate, one-half the dose of racemic methylphenidate; MAX 20 mg/day (10 mg twice a day) c) extended-release (ages 6 years and older): methylphenidate-naive patients, initial 5 mg ORALLY in the morning; adjust dose weekly in 5 mg increments; MAX 20 mg/day(Prod Info FOCALIN XR(R) extended-release oral capsules, 2008) d) extended-release (ages 6 years -

Drug Abuse Urine Tests: False-Positive Results Joseph A
University of the Pacific Scholarly Commons School of Pharmacy and Health Sciences Faculty Thomas J. Long School of Pharmacy and Health Articles Sciences 3-1-2005 Drug abuse urine tests: false-positive results Joseph A. Woelfel University of the Pacific, [email protected] Follow this and additional works at: https://scholarlycommons.pacific.edu/phs-facarticles Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Woelfel, J. A. (2005). Drug abuse urine tests: false-positive results. Pharmacist’s Letter & Prescriber’s Letter, 21(3), 1–5. https://scholarlycommons.pacific.edu/phs-facarticles/49 This Article is brought to you for free and open access by the Thomas J. Long School of Pharmacy and Health Sciences at Scholarly Commons. It has been accepted for inclusion in School of Pharmacy and Health Sciences Faculty Articles by an authorized administrator of Scholarly Commons. For more information, please contact [email protected]. ® Detail-Document #210314 ® −This Detail-Document accompanies the related article published in− PHARMACIST’S LETTER / PRESCRIBER’S LETTER March 2005 ~ Volume 21 ~ Number 210314 Drug Abuse Urine Tests: False-positive Results Lead author: Joseph A. Woelfel, Ph.D., FASCP, R.Ph., Assistant Editor Health care professionals are frequently asked questions about false-positive drug testing results. Testing is a common practice in work settings, rehabilitation programs, the military, and legal and judicial venues. Home testing is popular with the availability of test kits to alleviate parental or job-seeker concerns. Federally regulated workplace drug testing and most private sector workplace programs specify urine testing as their initial standard test. Other expanded tests may be required in some settings. -
Controlled Drug Schedules, Violations & Penalties
CONTROLLED DRUG SCHEDULES, VIOLATIONS & PENALTIES A REFERENCE FOR THE LAW ENFORCEMENT COMMUNITY April 2015 Prepared by the DEPARTMENT OF CONSUMER PROTECTION Drug Control Division TABLE OF CONTENTS SECTION I CONTROLLED DRUG SCHEDULES & VIOLATIONS An alphabetical listing of controlled drugs by their brand, generic and/or street name that includes each drug’s schedule and the violation(s) from the Connecticut General Statutes (CGS) that are associated with each drug’s sale and/or possession. SECTION II CONTROLLED DRUG VIOLATIONS & PENALTIES A numerical listing of controlled drug violations by their section number in the Connecticut General Statutes (CGS) and the penalty(ies) associated with each violation. SECTION III SUMMARY OF FEDERAL METHAMPHETAMINE STATUTES 2 S E C T I O N I CONTROLLED DRUG SCHEDULES & VIOLATIONS The ‘Schedules of Controlled Substances’ may be found in Sections 21a-243-7 through 21a-243-11, inclusive, of the Regulations of Connecticut State Agencies. www.ct.gov/dcp/lib/dcp/dcp_regulations/21a-243_designation_of_controlled_drugs.pdf 3 Drug State CS Drug Type AKA Sale or Quantity Person Drug- CGS Schedule Possession? Dependent or Not Violation APAP = Acetaminophen APAP = Acetaminophen Drug-Dependent ? ASA = Aspirin ASA = Aspirin “2C-C” Designer Drug - Stimulant “Bath Salts” Federal CS Schedule 1 “2C-D” Designer Drug - Stimulant “Bath Salts” Federal CS Schedule 1 “2C-E” Designer Drug - Stimulant “Bath Salts” Federal CS Schedule 1 “2C-H” Designer Drug - Stimulant “Bath Salts” Federal CS Schedule 1 “2C-I” Designer Drug - Stimulant