View This Issue As A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dundee Women's Trail Want to Know More?
Dundee Women’s Trail Many have made history worldwide. 21 Bella Keyzer 24 Janet Keiller Dundee Women’s Trail celebrates just a few amazing women whose lives touched 1922 - 1992 1737 - 1813 this city. Those we mark along this Trail are testimony to Dundee’s reputation for During World War Two, women took over She and her husband ran a cake and sweetie the jobs of the men who were fighting shop. One day, faced with a consignment of strong women. abroad, and Bella found her vocation as a unwanted bitter oranges, she boiled them welder in Caledon Shipyard. She was paid up to make the first chip marmalade. When The 25 women commemorated by bronze plaques in the city include artists, trades off four years later, but as soon as the Equal the menfolk died, she and her daughter- unionists, social reformers, suffragettes, a shipyard welder and a marine engineer. Opportunities Act was passed in 1975, she in-law Margaret ran the business - very was back. She was a loyal Labour Party successfully. member, and in 1992 Dundee District Take a walk through the streets they knew and glimpse the lives they led. Council, as it was then, gave her an award 25 Emma Caird (or Marryat) for promoting women’s equality. 1849 - 1927 Daughter of a mega-rich mill owner, she 22 Ethel Moorhead was a bright spark in her youth. In old 1869 - 1955 age, she was better known as ‘the greatest Ethel studied art in Paris and exhibited in benefactress Dundee has ever seen’, as she prestigious galleries. -

December 2009 (PDF)
The magazine of the University of Dundee • December 09 www.dundee.ac.uk/pressoffice Visions of Discovery contact•dec 09 1 contents news................. 03 from the principal... Those of you who attended my presentations in late September/early October will have heard me speak of my vision for the future of the University, and of how this vision is underpinned by the three watchwords of Excellence, Focus and Impact. The University must strive for excellence in everything it does, whether teaching, research or the professionalism of its botanic gardens... 06 support staff and services. In order to achieve this, the University must focus investment and resource in those areas with the proven record or the potential to sustain excellence. By focusing on our strengths and by aspiring to be the best, the University will inevitably increase its impact, whether social, economic, scientific or intellectual. November saw the publication of two significant documents affecting higher education in the UK. The first, Higher Ambitions, published on 3rd November to the fanfare of a speech by Lord Mandelson, sets out the UK Government’s framework for sustaining the strength of higher education in an ‘increasingly demanding and competitive environment’. The second, The impact of universities on the UK economy, was commissioned by Universities UK and presents the key benefits of higher education to the UK’s economy. It strikes me that our vision resonates with aspects of both of these documents. The Universities discovery day...... 12 UK report emphasises and demonstrates conclusively the huge financial impact that the combined activities of the higher education sector have on the economy, generating over £59 billion of output and over 668,500 fte jobs in 2007-8. -
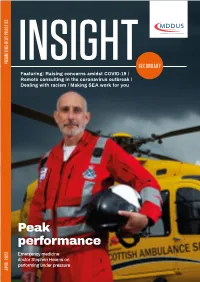
Insight-Secondary-Q2-2020.Pdf
Featuring: Raising concerns amidst COVID-19 / Remote consulting in the coronavirus outbreak / Dealing with racism / Making SEA work for you Peak performance Emergency medicine doctor Stephen Hearns on performing under pressure Welcome Dr Greg Dollman Editor WELCOME to the first issue of Insight Secondary Care – one of three new quarterly magazines we are launching at MDDUS to broaden the scope of content we produce for all our medical and dental members. I am excited to take on the role of editor and hope you find this inaugural issue both interesting and useful. All comments and suggestions are most welcome. Coronavirus is presenting an enormous challenge for the health service, so in this issue we feature relevant, practical advice for clinicians. On page 4 risk adviser Kay Louise Grant highlights key points when raising safety concerns in times of crisis. Remote consulting has become a crucial part of coronavirus care. On page 5 risk adviser Alan Frame explores how to minimise risk in treating patients online or via telephone or video. If anyone knows how to perform under pressure it’s emergency medicine MEDICATION physician and helicopter rescue medic Dr Stephen Hearns. He talks fighting fatigue and avoiding “frazzle” on page 8. HIV treatment roll-out Significant event analysis is not easy to get right and many of the SEAs we see at MDDUS are more description THE preventative HIV treatment PrEP is to be rolled out across than analysis. On page 10, Liz Price offers tips on making England thanks to a £16 million funding boost. them more than just box-ticking exercises. -

The Magazine of the University of Dundee • December 2012
The magazine of the University of Dundee • December 2012 www.dundee.ac.uk/pressoffice contact•December 12 1 contents news......................03 from the principal... It is good to feel the sense of excitement and interest across the University in our new vision and ambitious 25-year goal to become Scotland’s leading university. The University strategy is our roadmap as we begin the journey towards achieving this goal; it charts the way forward and monitors our performance against key targets during the next five years (available on My Dundee). For the first time and perhaps uniquely for a Scottish university equal emphasis has transforming lives...14 been placed on three elements of academic strategy: learning & teaching, research and wider impact. The last refers to our knowledge exchange and public engagement agenda which is being led by our new Vice-Principal & Head of the College of Art, Science and Engineering, Professor Stephen Decent. The idea behind this is simple: universities operate on the principle that teaching and research enhance one another. It seems to me to be self-evident that wider impact both informs and is informed by teaching and research and more importantly connects the university to the world outside. It helps to accelerate the take-up of new knowledge to drive the development of innovative businesses and at the same time can ensure our students are educated in an engaged environment which contributes to their employability after graduation. It is important to appreciate, however, that the kind of engaged university that I am talking about velvet venom..........19 is not one that has simply replaced fundamental research with applied research and introduced court news..............20 to the curriculum a module or two on entrepreneurism. -

Fairwood in the Making
In the Making Fairwood In the Making Tam Fairlie Duxpress 2017 1 Fairwood www.duxpress.com 2 In the Making A Brief History of Fairwood page 5 Some Fairlie Family History page 12 Alternative Facts page 56 The Fraser / Home / Hardy Connections page 60 A History of the Seafaring Woods page 75 The Patriotic Company page 100 Brigs, Brigantines, Schooners and Sloops page 116 Wood Properties and Landmarks page 119 The Shaws of Bermuda and Philadelphia page 128 Richard Shaw-Wood page 138 Woodholm page 145 The Pointe au Baril Story page 174 The Early Fairwood Years page 187 The Samuel de Champlain expedition of 1616 page 212 Historical Artefacts in the Curiosity Box page 222 The Fairwood Woodlands Plan page 224 3 Fairwood for Isabel Shaw-Wood Fairlie June 20, 2017 Heraclitus: Sow a character and reap a destiny 4 In the Making A Brief History of Fairwood Five generations of descendants of Mary Shaw-Wood have known Fairwood as their summer home. Between 1902 and 1905, Mary visited Pointe au Baril and in the summer of 1906 built a cottage on Push-Wah Island, for her three children, Isabel, Richard and Joe. Other properties were purchased speculatively in the names of each of the children. Richard who died on his Sopwith Machine in 1917 was given Olive Island in Shawanaga Bay. Joe owned Hopewell Island in Shawanaga Bay, named after Captain Thomas Wood’s ship which had brought early Adventurers to the New World in the 1630’s. Isabel was given OK Point on Richmond Island and Champlain Point on Monument Island. -
The Forfar Directory and Year Book
THE FORFAR for year 1939 PRICE THREEPENCE. FORFAR PRINTED AND PUBLISHED BY W. SHEPHERD. 1939 AS USED BY THE MASTERS STEINWAY. BECHSTEIN. CRAMER. CHALLEN. BROADWOOD. ROGERS. REIBACH. BLUTHNER. Reconditioned Instruments at Reduced Prices. ^^^^dundee} LIMITED. 18-24 WHITEHALL STREET, DUNDEE. Also at 7 County Place, PERTH, and 135 High Street, MONTROSE. Mean most — last longest.' --mwiWF Friends getting married appreci- ate most the utility gift with lasting beauty and value. There is a lifetime's service in the large range of Wedding Gifts which we offer. There is a host of fine Suggestions in our Showcases. =^^^= JOHN A. CLARK, Jeweller & Silversmith, 40 CASTLE STREET, FORFAR. tnr c/*ln idJ^^ i< yy Ctjc Betoon iFire IN VARIOUS DESIGNS AND COLOURS SUITABLE FOR BEDROOMS, SITTING ROOMS, DINING ROOMS, LOUNGES, PUBLIC ROOMS &c, &c. FULL PARTICULARS ON APPLICATION TELEPHONE No. 61 EDNIE & KININMONTH FURNISHING IRONMONGERS 14 CASTLE STREET . FORFAR Take the Bus It's more CONVENIENT Regular Services to Perth, Blairgowrie, Coupar Angus, Alyth, Meigle, Glamis, Kirriemuir, Forfar, Brechin, Arbroath, &c. Direct Motor Coach connections with Edinburgh and the South, to London. Private Parties specially catered for at Moderate Cost. WEEKLY AND SEASON TICKETS ISSUED. FULL PARTICULARS FROM SCOTTISH MOTOR TRACTION Co. Ltd., 13 Nethergate, .... DUNDEE. 'PHONE 4409. COMMERCIAL STREET, 93 EAST HIGH STREET, BLAIRGOWRIE, FORFAR. 'Phone 131. 'Phone 144. : COPYRIGHT. 37th Year of Issue. THE FORFAR DIRECTORY «/(5X AND YEAR BOOK X^ 1939 1939 CONTAINING LIST HOUSEHOLDERS OF THE BURGH, OF THE , DIRECTORY OF TRADES AND PROFESSIONS, LIST OF PUBLIC BOARDS, SOCIETIES, ETC ETC. ETC. ALSO, LIST OF FARMERS AND OTHERS IN THE ADJOINING PARISHES. -

Mccall Phd 2013
University of Dundee DOCTOR OF PHILOSOPHY The Lass o' Pairts Social mobility for women through education in Scotland, 1850-1901. McCall, Alison Taylor Award date: 2013 Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 28. Sep. 2021 DOCTOR OF PHILOSOPHY The Lass o' Pairts Social mobility for women through education in Scotland, 1850-1901. Alison Taylor McCall 2013 University of Dundee Conditions for Use and Duplication Copyright of this work belongs to the author unless otherwise identified in the body of the thesis. It is permitted to use and duplicate this work only for personal and non-commercial research, study or criticism/review. You must obtain prior written consent from the author for any other use. Any quotation from this thesis must be acknowledged using the normal academic conventions. It is not permitted to supply the whole or part of this thesis to any other person or to post the same on any website or other online location without the prior written consent of the author.